Anat Cell Biol.
2019 Jun;52(2):115-119. 10.5115/acb.2019.52.2.115.
Ossification of the mamillo-accessory ligament: a review of the literature and clinical considerations
- Affiliations
-
- 1Seattle Science Foundation, Seattle, WA, USA. joei@seattlesciencefoundation.org
- 2Swedish Neuroscience Institute, Swedish Medical Center, Seattle, WA, USA.
- 3Department of Trauma Surgery, BG University Hospital Bergmannsheil, Ruhr University Bochum, Bochum, Germany.
- 4Department of Anatomical Sciences, St. George's University, St. Georg's, Grenada, West Indies.
- KMID: 2451213
- DOI: http://doi.org/10.5115/acb.2019.52.2.115
Abstract
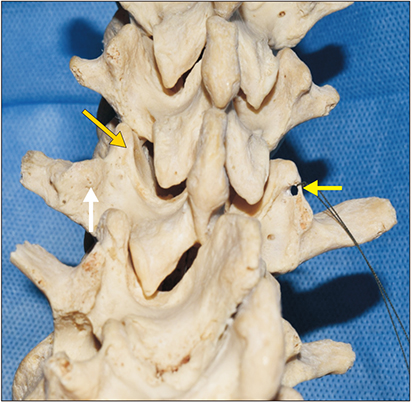
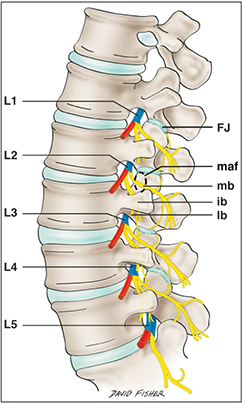
- Ossification of the mamillo-accessory ligament (MAL) is a misunderstood phenomenon; however, many have posited that it can result in nerve entrapment of the medial branch of the dorsal ramus causing zygapophyseal joint related low back pain. The MAL has been studied anatomically by few, yet the data indicate possible associations between ossification of this ligament and spondylosis. It has been proposed that mechanical stress upon the lumbar spine may also lead to progressive ossification of the MAL into a bony foramen.
Keyword
MeSH Terms
Figure
Reference
-
1. Bogduk N. Clinical and radiological anatomy of the lumbar spine. New York: Elsevier Health Sciences;2012.2. Vetter M, Oskouian RJ, Tubbs RS. “False” ligaments: a review of anatomy, potential function, and pathology. Cureus. 2017; 9:e1853.
Article3. Bogduk N. The lumbar mamillo: accessory ligament. Its anatomical and neurosurgical significance. Spine (Phila Pa 1976). 1981; 6:162–167.4. Provenzano DA. Lumbar facet nerve blocks: ultrasound. In : Narouze SN, editor. Multimodality Imaging Guidance in Interventional Pain Management. Oxford: Oxford University Press;2016. p. 254–264.5. Francois RJ, Bywaters EG, Aufdermaur M. Illustrated glossary for spinal anatomy. With explanations and a French and German translation. Rheumatol Int. 1985; 5:241–245.6. Odonkor CA, Shin BC, Cohen SP. The effect and role of steroids in facet joint radiofrequency denervation: a narrative review. Curr Phys Med Rehabil Rep. 2017; 5:180–185.
Article7. Moriggl B. Spine sonoanatomy for pain physicians. In : Narouze SN, editor. Atlas of Ultrasound-Guided Procedures in Interventional Pain Management. New York, NY: Springer;2018. p. 59–81.8. Mahato NK. Mamillo-accessory notch and foramen: distribution patterns and correlation with superior lumbar facet structure. Morphologie. 2014; 98:176–181.
Article9. Bogduk N. The innervation of the lumbar spine. Spine (Phila Pa 1976). 1983; 8:286–293.
Article10. Standring S. Gray's anatomy: the anatomical basis of clinical practice. 41st ed. New York: Elsevier;2016.11. Singh H, Chang Chien G, Bolash R. Anatomy of the spine. In : Pope JE, Deer TR, editors. Treatment of Chronic Pain Conditions. New York, NY: Springer;2017. p. 11–20.12. Gore S. Lumbar facet denervation for degenerative symptomatic functional spinal unit: overview. J Orthop Allied Sci. 2018; 6:8–12.
Article13. Maigne JY, Maigne R, Guerin-Surville H. The lumbar mamillo-accessory foramen: a study of 203 lumbosacral spines. Surg Radiol Anat. 1991; 13:29–32.
Article14. Anatomical observations on lumbar nerve posterior rami. Chin Med J (Engl). 1978; 4:492–496.15. Panjabi MM, Goel VK, Takata K. Physiologic strains in the lumbar spinal ligaments: an in vitro biomechanical study 1981 Volvo Award in Biomechanics. Spine (Phila Pa 1976). 1982; 7:192–203.16. Videman T, Nurminen M, Troup JD. 1990 Volvo Award in clinical sciences. Lumbar spinal pathology in cadaveric material in relation to history of back pain, occupation, and physical loading. Spine (Phila Pa 1976). 1990; 15:728–740.
Article17. Yang KH, King AI. Mechanism of facet load transmission as a hypothesis for low-back pain. Spine (Phila Pa 1976). 1984; 9:557–565.
Article18. Schultz A, Andersson G, Ortengren R, Haderspeck K, Nachemson A. Loads on the lumbar spine: validation of a biomechanical analysis by measurements of intradiscal pressures and myoelectric signals. J Bone Joint Surg Am. 1982; 64:713–720.
Article19. Bellew JW. Lumbar facets: an anatomic framework for low back pain. J Man Manip Ther. 1996; 4:149–156.
Article20. Jay G. Neuropathic low back pain: practical guide to chronic pain syndromes. Boca Raton, FL: CRC Press;2016.21. Cavanaugh JM, Lu Y, Chen C, Kallakuri S. Pain generation in lumbar and cervical facet joints. J Bone Joint Surg Am. 2006; 88:Suppl 2. 63–67.
Article22. Ehara S, Shimamura T, Nakamura R, Yamazaki K. Paravertebral ligamentous ossification: DISH, OPLL and OLF. Eur J Radiol. 1998; 27:196–205.
Article23. Shim JK, Moon JC, Yoon KB, Kim WO, Yoon DM. Ultrasound-guided lumbar medial-branch block: a clinical study with fluoroscopy control. Reg Anesth Pain Med. 2006; 31:451–454.
Article24. DePalma M. iSpine: evidence-based interventional spine care. New York: Demos Medical Publishing;2011.25. Dreyfuss P, Schwarzer AC, Lau P, Bogduk N. Specificity of lumbar medial branch and L5 dorsal ramus blocks: a computed tomography study. Spine (Phila Pa 1976). 1997; 22:895–902.26. Maddali P, Moisi M, Page J, Chamiraju P, Fisahn C, Oskouian R, Tubbs RS. Anatomical complications of epidural anesthesia: a comprehensive review. Clin Anat. 2017; 30:342–346.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ossification of the Posterior Longitudinal Ligament: 2 cases report
- Does Ossification of the Posterior Longitudinal Ligament Progress after Fusion?
- Ossification of the Coracoacromial Ligament in Subacromial Impingement Syndrome: A Case Report
- Simple Cyst Occurred in an Accessory Ovary
- A Case of Diffuse Idiopathic Skeletal Hyperostosis ( DISH ) Associated with Ossification of the Posterior Longuitudinal Ligament ( OPLL