J Korean Ophthalmol Soc.
2019 Jun;60(6):606-611. 10.3341/jkos.2019.60.6.606.
Papilledema with Cerebral Venous Sinus Thrombosis
- Affiliations
-
- 1Department of Ophthalmology, Dankook University College of Medicine, Cheonan, Korea. kseeye@hanmail.net
- KMID: 2449716
- DOI: http://doi.org/10.3341/jkos.2019.60.6.606
Abstract
- PURPOSE
We report two patients diagnosed with a sinus thrombosis with papillary edema.
CASE SUMMARY
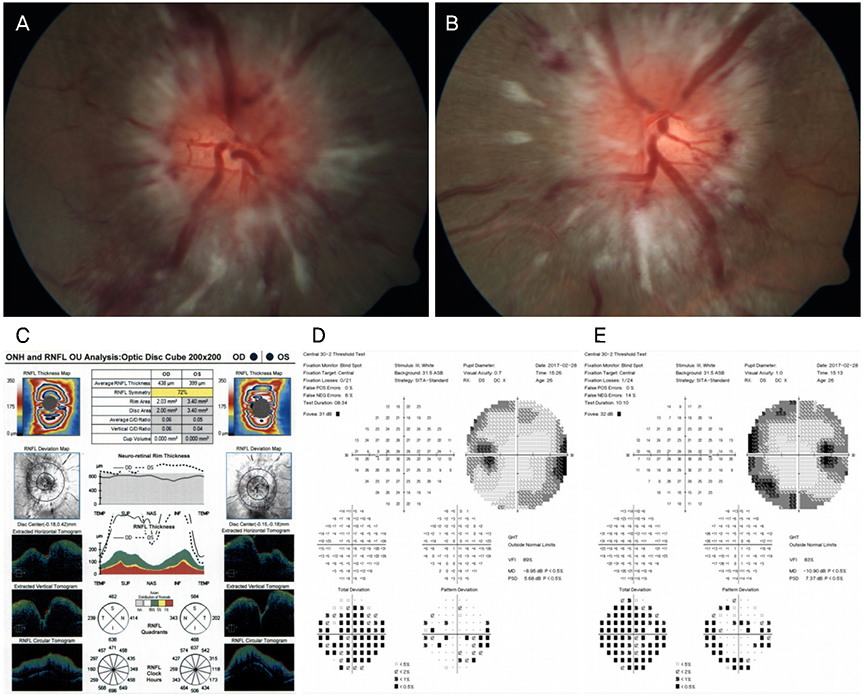
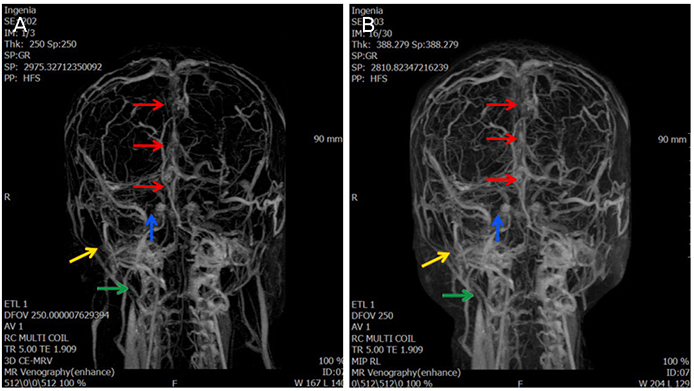
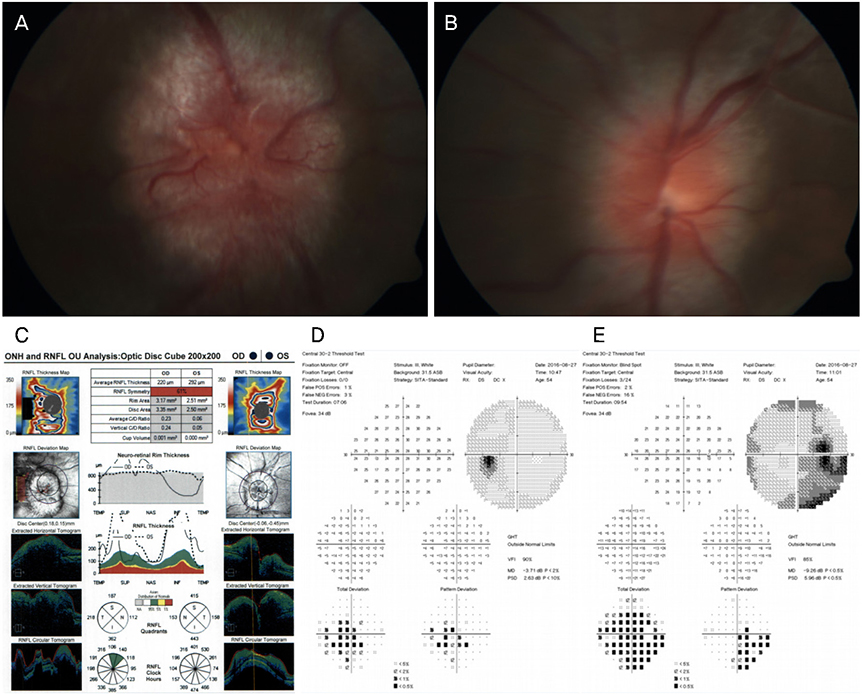
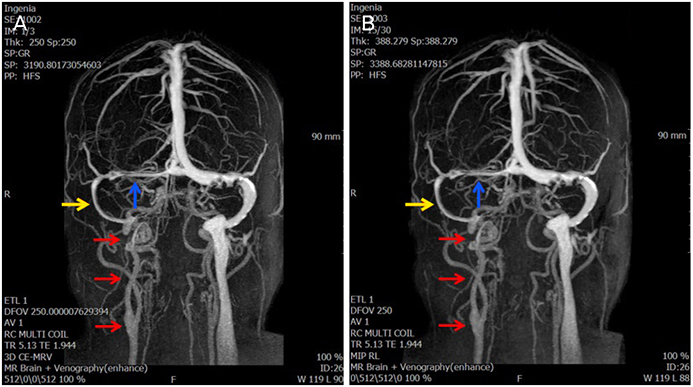
Case 1 was a 27-year-old male who presented with complaints of headache and vomiting for 2 months and blurred vision in both eyes. The best-corrected visual acuity (BCVA) was 1.0 in the right eye and 1.0 in the left eye. A visual field (VF) examination revealed a binocular peripheral VF defect and optical coherence tomography (OCT) and a fundus examination indicated optic disc swelling in both eyes. Brain magnetic resonance imaging (MRI) showed no specific finding but magnetic resonance venography revealed filling defect signs in the transverse sinus and a cerebrospinal fluid examination indicated elevated intracranial pressure (ICP). Case 2 was a 54-year-old female who came to our hospital with suspicion of bilateral optic disc swelling. The BCVA was 0.9 in the right eye and 1.0 in the left eye. A VF examination revealed an inferior-temporal VF defect and blind spot enlargement in the right eye. OCT and a fundus examination showed optic disc swelling in both eyes. Brain MRI showed no specific finding but magnetic resonance venography revealed a decrease in blood flow in the transverse sinus, sigmoid sinus. A cerebrospinal fluid examination indicated elevated ICP.
CONCLUSIONS
In the case of optic disc swelling in both eyes, a secondary cause of ICP elevation and the possibility of optic disc swelling due to sinus thrombosis should be considered, and brain MRI and venography are needed to distinguish these possibilities.
MeSH Terms
Figure
Reference
-
1. Einhäupl K, Bousser MG, de Bruijn SF, et al. EFNS guideline on the treatment of cerebral venous and sinus thrombosis. Eur J Neurol. 2006; 13:553–559.
Article2. Ferro JM, Canhão P, Stam J, et al. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004; 35:664–670.3. Kimber J. Cerebral Venus Thrombosis. QJM. 2002; 95:137–142.4. Keane JR. Cavernous sinus syndrome. Analysis of 151 cases. Arch Neurol. 1996; 53:967–971.
Article5. Van Stavern GP. Optic disc edema. Semin Neurol. 2007; 27:233–243.
Article6. Singh RJ, Saini J, Varadharajan S, et al. Headache in cerebral venous sinus thrombosis revisited: exploring the role of vascular congestion and cortical vein thrombosis. Cephalalgia. 2018; 38:503–510.
Article7. Lessell S, Rosman NP. Permanent visual impairment in childhood pseudotumor cerebri. Arch Neurol. 1986; 43:801–804.
Article8. Baker RS, Carter D, Hendrick EB, Buncic JR. Visual loss in pseudotumor cerebri of childhood. A follow-up study. Arch Ophthalmol. 1985; 103:1681–1686.9. Corbett JJ, Savino PJ, Thompson HS, et al. Visual loss in pseudotumor cerebri. Follow-up of 57 patients from five to 41 years and a profile of 14 patients with permanent severe visual loss. Arch Neurol. 1982; 39:461–474.
Article10. Wall M, George D. Visual loss in pseudotumor cerebri. Incidence and defects related to visual field strategy. Arch Neurol. 1987; 44:170–175.11. Corbett JJ, Nerad JA, Tse DT, Anderson RL. Results of optic nerve sheath fenestration for pseudotumor cerebri: the lateral orbitotomy approach. Arch Ophthalmol. 1988; 106:1391–1397.12. Dersh J, Schlezinger NS. Inferior nasal quadrantanopia in pseudotumor cerebri. Trans Am Neurol Assoc. 1959; 84:116–118.13. Orcutt JC, Page NG, Sanders MD. Factors affecting visual loss in benign intracranial hypertension. Ophthalmology. 1984; 91:1303–1312.
Article14. O'Rourke TL, Slagle WS, Elkins M, et al. Papilloedema associated with dural venous sinus thrombosis. Clin Exp Optom. 2014; 97:133–139.15. Ozsvath RR, Casey SO, Lustrin ES, et al. Cerebral venography: comparison of CT and MR projection venography. AJR Am J Roentgenol. 1997; 169:1699–1707.
Article16. Shah S, Saxena D. Bilateral papilledema: a case of cerebral venous sinus thrombosis. Oman J Ophthalmol. 2014; 7:33–34.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Leptomeningeal Metastasis Associated with Cerebral Venous Thrombosis
- Papilledema and Cere b ral Venous Thrombosis in a Patient with Systemic Lupus Ery thematosis
- Cerebral Venous Sinus Thrombosis Associated with Antithrombin III Deficiency: A Case Report
- Development of Subdural Hemorrhage in a Patient With Cerebral Venous Sinus Thrombosis
- Neuro-Behcet's Disease Presented with Cerebral Venous Sinus Thrombosis: A Case Report