Int J Thyroidol.
2019 May;12(1):58-63. 10.11106/ijt.2019.12.1.58.
Concurrent Medullary Thyroid Carcinoma and Primary Thyroid Lymphoma (Diffuse Large B Cell Lymphoma): the First Case Report
- Affiliations
-
- 1Department of Pathology, Soonchunhyang University Seoul Hospital, Seoul, Korea. s78170@schmc.ac.kr
- 2Department of Internal Medicine, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- KMID: 2449067
- DOI: http://doi.org/10.11106/ijt.2019.12.1.58
Abstract
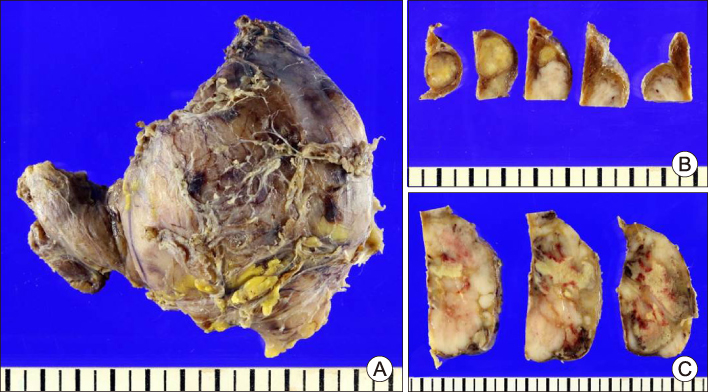
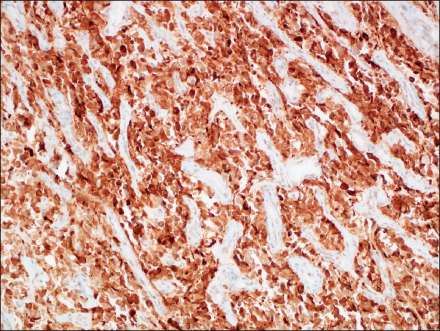
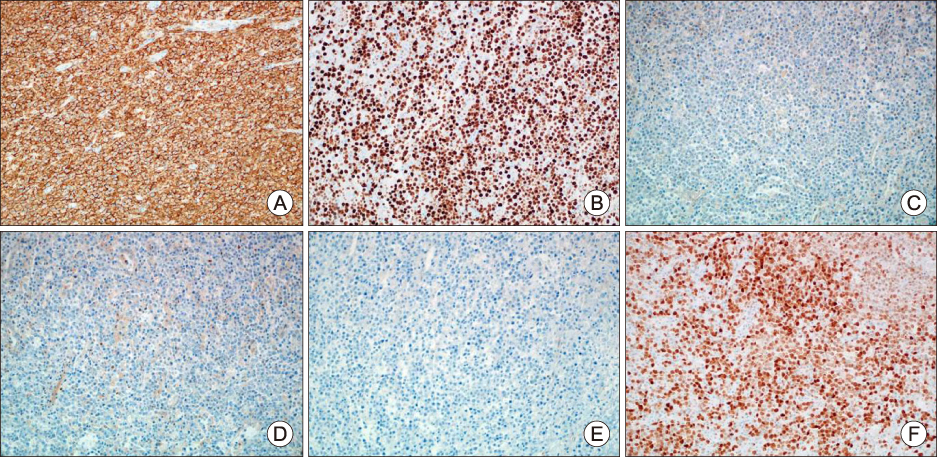
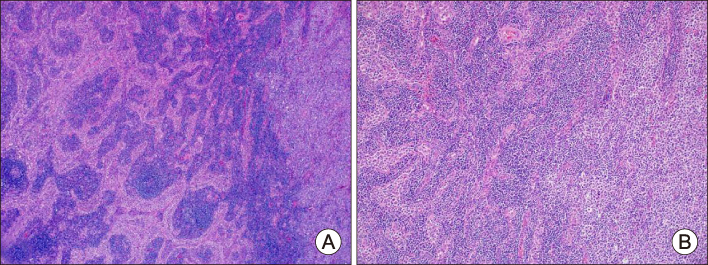
- Cases of simultaneously occurring medullary thyroid carcinoma (MTC) and lymphoma are extremely rare. An 84-year-old woman visited the hospital due to dyspnea, resulting from rapidly aggravated enlarged neck mass. Ultrasonography revealed two lesions in the thyroid and they were diagnosed as concurrent medullary thyroid carcinoma and diffuse large B cell lymphoma after total thyroidectomy. A few cases simultaneously diagnosed with MTC and systemic lymphoma have been reported. However, the coexistence of MTC and primary thyroid lymphoma is extremely rare.
MeSH Terms
Figure
Reference
-
1. Lloyd RV, Osamura RY, Kloppel G, Rosai J. WHO classification of tumours of endocrine organs. WHO classification of tumors. 4th ed. International Agency for Research on Cancer (IARC);2017.2. Ahmed M, Al-Saihati B, Greer W, Al-Nuaim A, Bakheet S, Abdulkareem AM, et al. A study of 875 cases of thyroid cancer observed over a fifteen-year period (1975-1989) at the King Faisal Specialist Hospital and Research Centre. Ann Saudi Med. 1995; 15(6):579–584.
Article3. Papajik T, Myslivecek M, Sedova Z, Buriankova E, Prochazka V, Raida L, et al. Synchronous second primary neoplasms detected by initial staging F-18 FDG PET/CT examination in patients with non-Hodgkin lymphoma. Clin Nucl Med. 2011; 36(7):509–512.
Article4. Catana R, Boila A, Borda A. Thyroid cancer profile in Mures County (Romania): a 20 years study. Rom J Morphol Embryol. 2012; 53(4):1007–1012.5. Lan XB, Cao J, Zhu XH, Han Z, Huang YQ, Ge MH, et al. Concomitant papillary thyroid carcinoma and mucosa-associated lymphoid tissue thyroid lymphoma in the setting of Hashimoto thyroiditis. Int J Clin Exp Pathol. 2018; 11(6):3076–3083.6. Cheng V, Brainard J, Nasr C. Co-occurrence of papillary thyroid carcinoma and primary lymphoma of the thyroid in a patient with long-standing Hashimoto’s thyroiditis. Thyroid. 2012; 22(6):647–650.
Article7. Shen G, Ji T, Hu S, Liu B, Kuang A. Coexistence of papillary thyroid carcinoma with thyroid MALT lymphoma in a patient with Hashimoto's thyroiditis: A clinical case report. Medicine (Baltimore). 2015; 94(52):e2403.8. Mathai C, Ruby E. Case Report: Coexistence of papillary thyroid cancer and thyroid lymhoma. The Medicine Forum. 2018; 19:15–16.
Article9. Paschali A, Moonim M, Hubbard J, Mohan H. 18F-FDG PET detection of a medullary thyroid carcinoma in a patient with SMZL. Clin Nucl Med. 2016; 41(10):e447–e448.
Article10. Acosta-Ortega J, Montalban-Romero S, Garcia-Solano J, Sanchez-Sanchez C, Perez-Guillermo M. Simultaneous medullary carcinoma of the thyroid gland and Hodgkin's lymphoma in bilateral lymph nodes of the neck: a potential pitfall in fine-needle aspiration cytology. Diagn Cytopathol. 2004; 31(4):255–258.
Article11. Bocian A, Kopczynski J, Rieske P, Piaskowski S, Sluszniak J, Kupnicka D, et al. Simultaneous occurrence of medullary and papillary carcinomas of the thyroid gland with metastases of papillary carcinoma to the cervical lymph nodes and the coinciding small B-cell lymphocytic lymphoma of the lymph nodes--a case report. Pol J Pathol. 2004; 55(3):23–30.12. Willard EM. Medullary carcinoma of the thyroid in a patient treated for Hodgkin's disease. Am J Med. 1990; 89(5):690.
Article13. Machaczka M. Mantle cell lymphoma successfully treated in a patient with multiple endocrine neoplasia type 2: a rare combination of two malignancies. Med Oncol. 2012; 29(3):2174–2175.
Article14. Resende de, Gronhoj C, Feldt-Rasmussen U, von Buchwald C. Association between Hashimoto's thyroiditis and thyroid cancer in 64,628 patients. Front Oncol. 2017; 7:53.
Article15. Dasgupta S, Chakrabarti S, Mandal PK, Das S. Hashimoto's thyroiditis and medullary carcinoma of thyroid. JNMA J Nepal Med Assoc. 2014; 52(194):831–833.
Article16. Gaskin D, Parai SK, Parai MR. Hashimoto's thyroiditis with medullary carcinoma. Can J Surg. 1992; 35(5):528–530.17. Patel BK, Roy A, Badhe BA, Siddaraju N. Cytologic aspects of an interesting case of medullary thyroid carcinoma coexisting with Hashimoto’s thyroiditis. J Cytol. 2016; 33(2):100–102.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Thyroid Lymphoma Associated with Hashimoto's Thyroiditis
- A Case of Epstein-Barr Virus-Positive Diffuse Large B-Cell Lymphoma Occurring in Thyroid Gland
- Concurrent Medullary Carcinoma and Hashimoto’s Thyroiditis: A Case Report with an Emphasis on US Features
- Concurrent Medullay and Papillary Carcinoma of the Thyroid
- Three Cases of Primary Thyroid Lymphoma at a Single Institution