J Rhinol.
2019 May;26(1):8-15. 10.18787/jr.2019.26.1.8.
Effect of Endonasal Dilator on Nasal Airflow and Sleep Test Index on Sleep Apnea Patients
- Affiliations
-
- 1Department of Otorhinolaryngology, Inha University College of Medicine, Incheon, Korea. inhaorl@inha.ac.kr
- KMID: 2449022
- DOI: http://doi.org/10.18787/jr.2019.26.1.8
Abstract
- BACKGROUND AND OBJECTIVES
We aimed to evaluate effects of endonasal dilators (END) on sleep quality in patients with obstructive sleep apnea (OSA) by improving nasal airflow.
MATERIALS AND METHODS
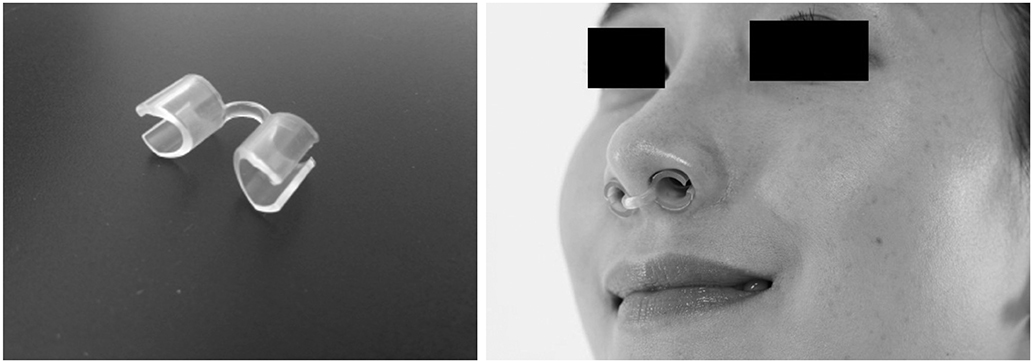
In 13 patients with OSA, changes of total nasal volume (TNV) and minimal cross-sectional area (MCA) before and after END use were evaluated. The change in peak nasal inspiratory flow (PNIF) was also measured. Subjects completed Epworth Sleepiness Scale questionnaire before and 2 weeks after END use. Finally, changes in apnea-hypopnea index (AHI), respiratory distress index (RDI), oxygen desaturation index (ODI), sleep time, sleep position and loudness of snoring (in decibels) were obtained by repetitive portable polysomnography.
RESULTS
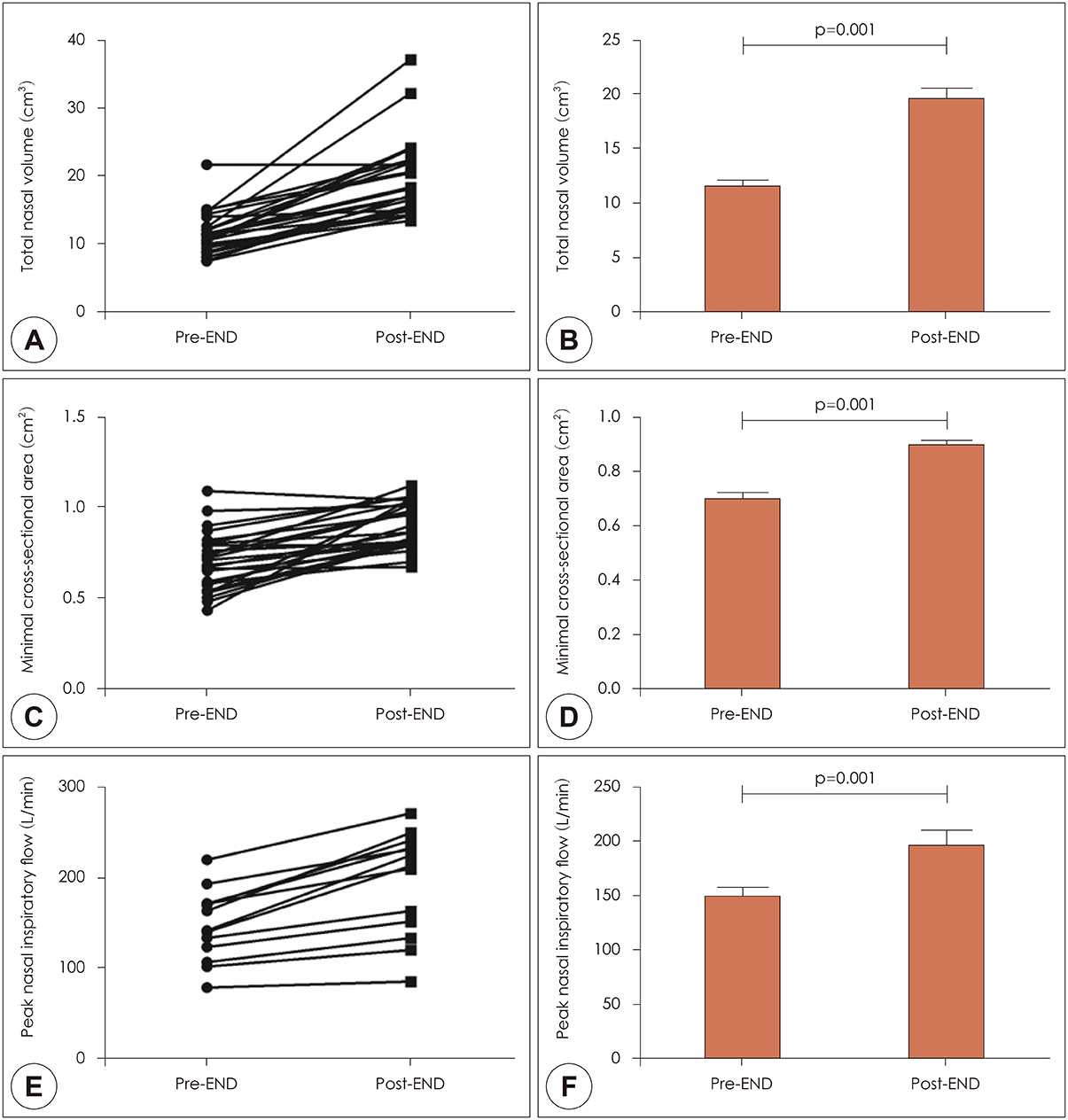
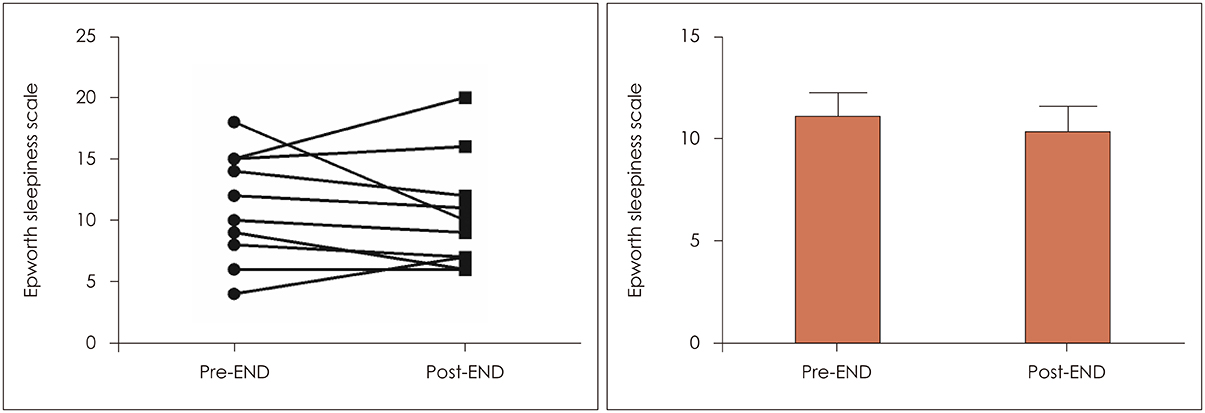
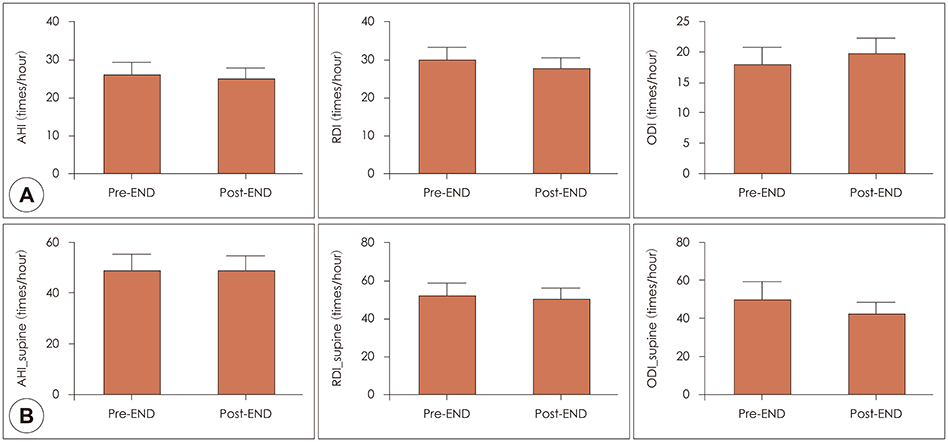
After END use, TNV (11.4±3.1 cm3 to 19.4±5.7 cm3) and MCA (0.7±0.2 cm2 to 0.9±0.1 cm2) increased significantly (p=0.001). PNIF also increased significantly after END (147.3±39.5 to 194.6±57.6 liter/min, p=0.001). Among 11 patients undergoing 2-week follow-up, 7 reported improvement in daytime sleepiness. Although AHI, RDI and ODI showed no statistically significant change before and after END (p>0.05), the proportion of subjects sleeping in the supine position increased from 38.0 to 44.5%.
CONCLUSION
END may be an effective adjunctive tool for patients with OSA with the potential to improve nasal airflow and daytime sleepiness.
MeSH Terms
Figure
Reference
-
1. Neruntarat C. Uvulopalatal flap for obstructive sleep apnea: shortterm and long-term results. The Laryngoscope. 2011; 121:683–687.
Article2. Lin T, Huang J-F, Lin Q-C, Chen G-P, Wang B-Y, Zhao J-M, et al. The effect of CPAP treatment on venous lactate and arterial blood gas among obstructive sleep apnea syndrome patients. Sleep Breath. 2017; 21:303–309.
Article3. Can M, Uygur F, Tanrıverdi H, Acıkgoz B, Alper B, Guven B. Effect of continuous positive airway pressure (CPAP) therapy on IL-23 in patients with obstructive sleep apnea. Immunol Res. 2016; 64:1179–1184.
Article4. Riachy M, Najem S, Iskandar M, Choucair J, Ibrahim I, Juvelikian G. Factors predicting CPAP adherence in obstructive sleep apnea syndrome. Sleep Breath. 2017; 21:295–302.
Article5. Hevener B, Hevener W. Continuous Positive Airway Pressure Therapy for Obstructive Sleep Apnea: Maximizing Adherence Including Using Novel Information Technology-based Systems. Sleep Med Clin. 2016; 11:323–329.
Article6. Baker AB, Xiao CC, O’Connell BP, Cline JM, Gillespie MB. Uvulopalatopharyngoplasty: Does Multilevel Surgery Increase Risk? Otolaryngol Head Neck Surg. 2016; 155:1053–1058.7. Choi JH, Cho SH, Kim S-N, Suh JD, Cho JH. Predicting Outcomes after Uvulopalatopharyngoplasty for Adult Obstructive Sleep Apnea: A Meta-analysis. Otolaryngol Head Neck Surg. 2016; 155:904–913.
Article8. Ulfberg J, Fenton G. Effect of Breathe Right nasal strip on snoring. Rhinology. 1997; 35:50–52.9. Petruson B. The importance of improved nasal breathing: a review of the Nozovent nostril dilator. Acta Otolaryngol. 2007; 127:418–423.
Article10. Ellegård E. Mechanical nasal alar dilators. Rhinology. 2006; 44:239–248.11. Jang TY, Kim YH. Nasal provocation test is useful for discriminating allergic, nonallergic, and local allergic rhinitis. Am J Rhinol Allergy. 2015; 29:e100–e104.
Article12. Kim YH, Jang TY. Proposed diagnostic standard using visual analogue scale and acoustic rhinometry in nasal provocation test in allergic patients. Auris Nasus Larynx. 2011; 38:340–346.
Article13. Djupesland PG, Skatvedt O, Borgersen AK. Dichotomous physiological effects of nocturnal external nasal dilation in heavy snorers: the answer to a rhinologic controversy? Am J Rhinol. 2001; 15:95–103.
Article14. Peltonen LI, Vento SI, Simola M, Malmberg H. Effects of the nasal strip and dilator on nasal breathing--a study with healthy subjects. Rhinology. 2004; 42:122–125.15. Latte J, Taverner D. Opening the nasal valve with external dilators reduces congestive symptoms in normal subjects. Am J Rhinol. 2005; 19:215–219.
Article16. Roithmann R, Chapnik J, Cole P, Szalai J, Zamel N. Role of the external nasal dilator in the management of nasal obstruction. The Laryngoscope. 1998; 108:712–715.
Article17. Metes A, Cole P, Hoffstein V, Miljeteig H. Nasal airway dilation and obstructed breathing in sleep. The Laryngoscope. 1992; 102:1053–1055.
Article18. Dinardi RR, de Andrade CR, Ibiapina C. Evaluation of the effectiveness of the external nasal dilator strip in adolescent athletes: a randomized trial. Int J Pediatr Otorhinolaryngol. 2013; 77:1500–1505.
Article19. Dinardi RR, de Andrade CR, Martins-Costa HC, Ibiapina C. Does the Airmax® internal nasal dilator increase peak nasal inspiratory flow (PNIF) in adolescent athletes. Int J Pediatr Otorhinolaryngol. 2016; 84:37–42.
Article20. Barnes ML, Lipworth BJ. Removing nasal valve obstruction in peak nasal inspiratory flow measurement. Ann Allergy Asthma Immunol. 2007; 99:59–60.
Article21. Raudenbush B. Stenting the nasal airway for maximizing inspiratory airflow: internal Max-Air Nose Cones versus external Breathe Right strip. Am J Rhinol Allergy. 2011; 25:249–251.
Article22. Shinkawa A, Sakai M. A clinical study of the nasal dilator Nozovent in Japanese subjects. Tokai J Exp Clin Med. 1998; 23:13–17.23. Scharf MB, Brannen DE, McDannold M. A subjective evaluation of a nasal dilator on sleep & snoring. Ear Nose Throat J. 1994; 73:395–401.
Article24. Petruson B, Theman K. Clinical evaluation of the nasal dilator Nozovent. The effect on snoring and dryness of the mouth. Rhinology. 1992; 30:283–287.25. Pevernagie D, Hamans E, Van Cauwenberge P, Pauwels R. External nasal dilation reduces snoring in chronic rhinitis patients: a randomized controlled trial. Eur Respir J. 2000; 15:996–1000.
Article26. Schönhofer B, Kerl J, Suchi S, Köhler D, Franklin KA. Effect of nasal valve dilation on effective CPAP level in obstructive sleep apnea. Respir Med. 2003; 97:1001–1005.
Article27. Hoffstein V, Mateika S, Metes A. Effect of nasal dilation on snoring and apneas during different stages of sleep. Sleep. 1993; 16:360–365.
Article28. Schönhofer B, Franklin KA, Brünig H, Wehde H, Köhler D. Effect of nasal-valve dilation on obstructive sleep apnea. Chest. 2000; 118:587–590.
Article29. Löth S, Petruson B. Improved nasal breathing reduces snoring and morning tiredness. A 6-month follow-up study. Arch Otolaryngol Head Neck Surg. 1996; 122:1337–1340.
Article30. Petruson B, Löth S. Five-year compliance with a nostril dilator. Arch Otolaryngol Head Neck Surg. 2000; 126:1168–1169.31. Adams CM, Peiffer JJ. Neither internal nor external nasal dilation improves cycling 20-km time trial performance. J Sci Med Sport. 2017; 20:415–419.
Article32. Kim YH, Jang TY. Proposed diagnostic standard using visual analogue scale and acoustic rhinometry in nasal provocation test in allergic patients. Auris Nasus Larynx. 2011; 38:340–346.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sleep Disordered Breathing and Nasal Obstruction
- Pathogenesis of Obstructive Sleep Apnea
- The Effect of Nasal Obstruction on Sleep Apnea
- Allergic Rhinitis and Sleep-disordered Breathing
- The Nasal Airflow Pressure Monitoring and the Measurement of Airway Pressure Changes in Obstructive Sleep Apnea Syndrome and Upper Airway Resistance Syndrome