Clin Orthop Surg.
2019 Jun;11(2):226-232. 10.4055/cios.2019.11.2.226.
Surgical Results of Limb Lengthening at the Femur, Tibia, and Humerus in Patients with Achondroplasia
- Affiliations
-
- 1Department of Orthopedic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jss3505@skku.edu
- KMID: 2445059
- DOI: http://doi.org/10.4055/cios.2019.11.2.226
Abstract
- BACKGROUND
Results of limb lengthening in patients with achondroplasia were previously reported in many studies. However, the reports of comparison among the three long bones (femur, tibia, and humerus) are rare, especially for the results of crossed lengthening (lengthening of one femur and contralateral tibia followed by that of the opposite side) for the lower limbs. The purpose of this study was to report the surgical results of a series of limb lengthening in achondroplastic or hypochondroplasia patients at our institution.
METHODS
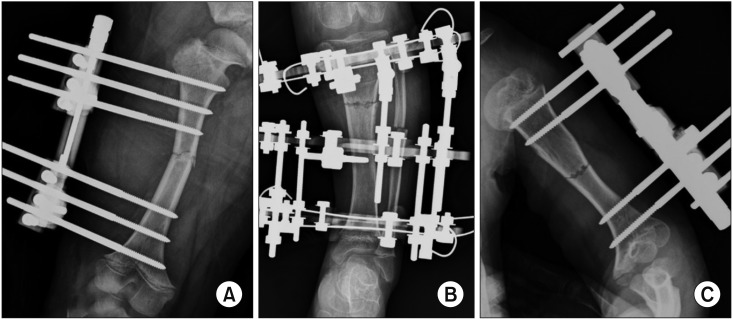
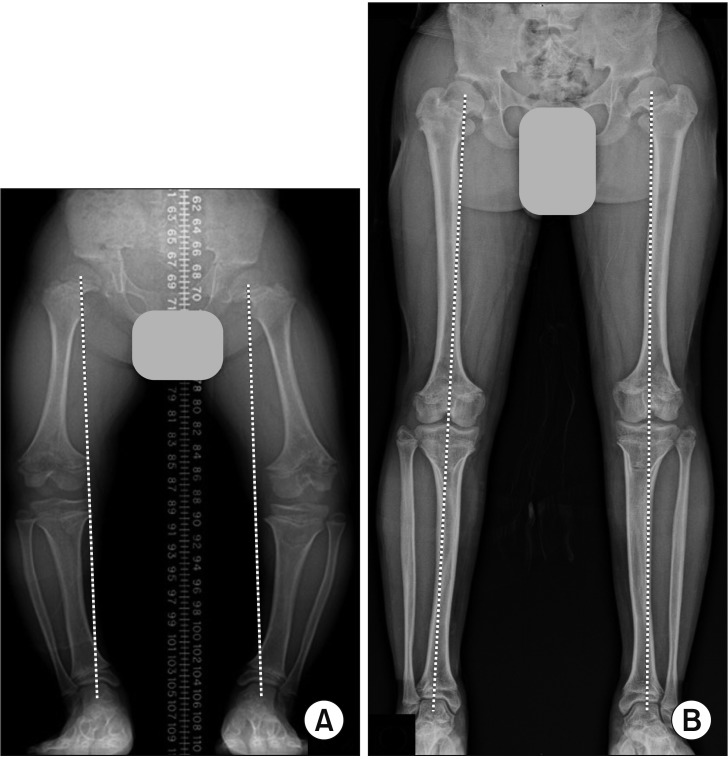
Fifteen patients (14 with achondroplasia and 1 with hypochondroplasia) underwent lower limb lengthening of the femur (n = 32) and tibia (n = 28), and 12 of them underwent crossed lengthening. Humeral lengthening was performed in 14 patients (n = 28). The mean age at the first operation was 11.7 years, and the mean follow-up duration was 66.7 months. The healing index, consolidation period index (duration of consolidation period/gained length), and other radiographic indices were analyzed. Limb length discrepancy and hip-knee-ankle alignment in lower limbs, and the occurrence of difficulties were assessed.
RESULTS
The average gain in length for the femur, tibia, and humerus was 8.3 cm, 8.5 cm, and 7.4 cm, respectively. The mean healing index was 29.6 days/cm for the femur, 29.0 days/cm for the tibia, and 27.2 days/cm for the humerus. The mean consolidation period index was 14.7 days/cm for the humerus, which was significantly lower than that in the lower limb (17.3 days/cm for the femur and 17.8 days/cm for the tibia). Of the 12 who underwent crossed lengthening, five showed limb length discrepancy ≥ 1.0 cm. Among their 24 lower limbs, three showed valgus alignment ≥ 5° and one showed varus alignment ≥ 5°. Thirty-two pin site infections and three fractures were conservatively managed. Three femoral fractures, eight equinus deformities, and four cases with premature consolidation of the fibula were surgically treated. Obstacle and true complication related to humeral lengthening were not observed.
CONCLUSIONS
Humeral lengthening was relatively effective and safe. Careful attention will be needed to avoid the occurrence of limb length discrepancy or malalignment in crossed lengthening.
Keyword
Figure
Reference
-
1. Balci HI, Kocaoglu M, Sen C, Eralp L, Batibay SG, Bilsel K. Bilateral humeral lengthening in achondroplasia with unilateral external fixators: is it safe and does it improve daily life? Bone Joint J. 2015; 97(11):1577–1581. PMID: 26530664.2. Kim SJ, Balce GC, Agashe MV, Song SH, Song HR. Is bilateral lower limb lengthening appropriate for achondroplasia? Midterm analysis of the complications and quality of life. Clin Orthop Relat Res. 2012; 470(2):616–621. PMID: 21785895.
Article3. Kim SJ, Pierce W, Sabharwal S. The etiology of short stature affects the clinical outcome of lower limb lengthening using external fixation: a systematic review of 18 trials involving 547 patients. Acta Orthop. 2014; 85(2):181–186. PMID: 24650027.4. Donaldson J, Aftab S, Bradish C. Achondroplasia and limb lengthening: results in a UK cohort and review of the literature. J Orthop. 2015; 12(1):31–34. PMID: 25829758.
Article5. Park KW, Garcia RA, Rejuso CA, Choi JW, Song HR. Limb lengthening in patients with achondroplasia. Yonsei Med J. 2015; 56(6):1656–1662. PMID: 26446651.
Article6. Kitoh H, Mishima K, Matsushita M, Nishida Y, Ishiguro N. Early and late fracture following extensive limb lengthening in patients with achondroplasia and hypochondroplasia. Bone Joint J. 2014; 96(9):1269–1273. PMID: 25183602.
Article7. Song SH, Agashe MV, Huh YJ, Hwang SY, Song HR. Physeal growth arrest after tibial lengthening in achondroplasia: 23 children followed to skeletal maturity. Acta Orthop. 2012; 83(3):282–287. PMID: 22489887.8. Akman SD, Karakas P, Bozkir MG. The morphometric measurements of humerus segments. Turk J Med Sci. 2006; 36(2):81–85.9. Venkatesh KP, Modi HN, Devmurari K, Yoon JY, Anupama BR, Song HR. Femoral lengthening in achondroplasia: magnitude of lengthening in relation to patterns of callus, stiffness of adjacent joints and fracture. J Bone Joint Surg Br. 2009; 91(12):1612–1617. PMID: 19949126.10. Li R, Saleh M, Yang L, Coulton L. Radiographic classification of osteogenesis during bone distraction. J Orthop Res. 2006; 24(3):339–347. PMID: 16479566.
Article11. Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990; (250):81–104.
Article12. Chilbule SK, Dutt V, Madhuri V. Limb lengthening in achondroplasia. Indian J Orthop. 2016; 50(4):397–405. PMID: 27512222.
Article13. Gross RH. Leg length discrepancy: how much is too much? Orthopedics. 1978; 1(4):307–310. PMID: 733195.
Article14. McCarthy JJ, MacEwen GD. Management of leg length inequality. J South Orthop Assoc. 2001; 10(2):73–85. PMID: 12132831.15. Vaidya SV, Song HR, Lee SH, Suh SW, Keny SM, Telang SS. Bifocal tibial corrective osteotomy with lengthening in achondroplasia: an analysis of results and complications. J Pediatr Orthop. 2006; 26(6):788–793. PMID: 17065948.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Limb Lengthening in Patients with Achondroplasia
- Classification and Evaluation of the Callus in Limb Lengthening
- Lower Limb Lengthening in Turner Dwarfism
- Endoprosthetic Reconstruction in the Limb Salvage Surgery for Treatment of Malignant Bone Tumors
- Lymphangiomatosis of Bone and Visceral Parenchyma : Report of Two Cases