Korean J Gastroenterol.
2019 Apr;73(4):219-224. 10.4166/kjg.2019.73.4.219.
Successful Treatment Using Endoluminal Vacuum Therapy after Failure of Primary Closure in Boerhaave Syndrome
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, School of Medicine, Kyungpook National University, Daegu, Korea. ldhms@naver.com
- 2Department of Thoracic and Cardiovascular Surgery, Kyungpook National University Hospital, Daegu, Korea.
- 3Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea.
- 4Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea.
- KMID: 2443635
- DOI: http://doi.org/10.4166/kjg.2019.73.4.219
Abstract
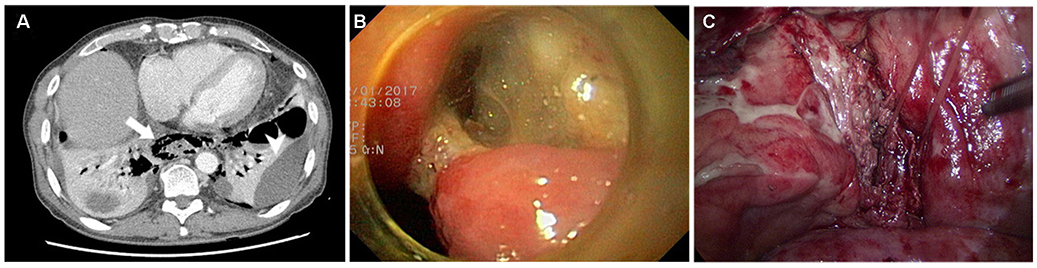
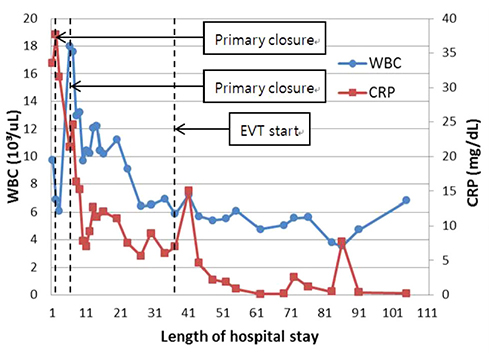
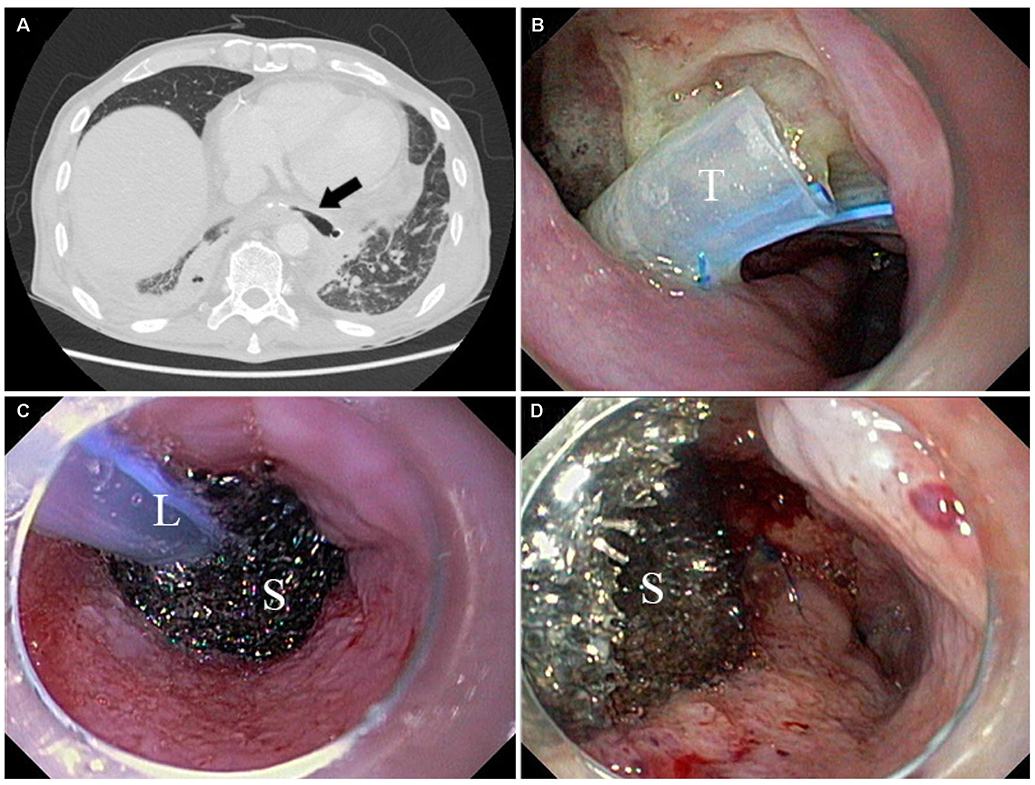
- Boerhaave syndrome is a transmural perforation of the esophagus and typically occurs after forceful emesis. Boerhaave syndrome is a destructive disease with a high mortality rate, though surgical intervention within 24 hours has a beneficial effect. On the other hand, late surgical intervention is associated with poorer prognoses. Several therapeutic strategies, ranging from medical to surgical management, are available for Boerhaave syndrome. Recently, endoscopic endoluminal vacuum therapy (EVT) was introduced as a treatment option. Here, we report the case of a 56-year-old male patient with Boerhaave syndrome who was successfully treated by EVT after primary closure failure. The patient recovered without complication.
MeSH Terms
Figure
Reference
-
1. Chirica M, Champault A, Dray X, et al. Esophageal perforations. J Visc Surg. 2010; 147:e117–e128.
Article2. Still S, Mencio M, Ontiveros E, Burdick J, Leeds SG. Primary and rescue endoluminal vacuum therapy in the management of esophageal perforations and leaks. Ann Thorac Cardiovasc Surg. 2018; 24:173–179.
Article3. Kim KD, Chung KY, Kim CS, Park HG. Delayed primary repair of esophageal rupture. Korean J Thorac Cardiovasc Surg. 1998; 31:46–51.4. Do YW, Lee CY, Lee S, Kim HE, Kim BJ, Lee JG. Successful management of delayed esophageal rupture with T-tube drainage using video-assisted thoracoscopic surgery. Korean J Thorac Cardiovasc Surg. 2016; 49:478–480.
Article5. Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997; 38:563–576.6. Loske G, Schorsch T. Endoscopic vacuum therapy for Boerhaave’s syndrome. Chirurg. 2016; 87:676–682.7. Listewnik MJ, Sielicki P, Mokrzycki K, Biskupski A, Brykczyński M. The use of vacuum-assisted closure in purulent complications and difficult-to-heal wounds in cardiac surgery. Adv Clin Exp Med. 2015; 24:643–650.
Article8. Johnsson E, Lundell L, Liedman B. Sealing of esophageal perforation or ruptures with expandable metallic stents: a prospective controlled study on treatment efficacy and limitations. Dis Esophagus. 2005; 18:262–266.
Article9. Qadeer MA, Dumot JA, Vargo JJ, Lopez AR, Rice TW. Endoscopic clips for closing esophageal perforations: case report and pooled analysis. Gastrointest Endosc. 2007; 66:605–611.
Article10. Rábago LR, Castro JL, Joya D, et al. Esophageal perforation and postoperative fistulae of the upper digestive tract treated endoscopically with the application of Tissucol. Gastroenterol Hepatol. 2000; 23:82–86.11. Brangewitz M, Voigtländer T, Helfritz FA, et al. Endoscopic closure of esophageal intrathoracic leaks: stent versus endoscopic vacuum-assisted closure, a retrospective analysis. Endoscopy. 2013; 45:433–438.
Article12. Heits N, Stapel L, Reichert B, et al. Endoscopic endoluminal vacuum therapy in esophageal perforation. Ann Thorac Surg. 2014; 97:1029–1035.
Article13. Möschler O, Nies C, Mueller MK. Endoscopic vacuum therapy for esophageal perforations and leakages. Endosc Int Open. 2015; 3:E554–E558.
Article14. Bludau M, Hölscher AH, Herbold T, et al. Management of upper intestinal leaks using an endoscopic vacuum-assisted closure system (E-VAC). Surg Endosc. 2014; 28:896–901.
Article15. Schorsch T, Müller C, Loske G. Endoscopic vacuum therapy of perforations and anastomotic insufficiency of the esophagus. Chirurg. 2014; 85:1081–1093.16. Scharl M, Stanek N, Kröger A, Bauerfeind P, Gubler C. Successful treatment of a proximal esophageal rupture with a luminal sponge. Endoscopy. 2015; 47:Suppl 1 UCTN. E293–E294.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vacuum-assisted close versus conventional treatment for postlaparotomy wound dehiscence
- Rectal perforation and perirectal abscess following stapled hemorrhoidectomy for prolapsed hemorrhoids successfully managed with Endo-SPONGE endoluminal vacuum-assisted wound closure system
- Usefulness of Endoluminal Vacuum-Assisted Closure Therapy for Pharyngocutaneous Fistula
- Endoscopic Management of Anastomotic Leakage after Esophageal Surgery: Ten Year Analysis in a Tertiary University Center
- Primary Repair of Boerhaave's Syndrome