Dement Neurocogn Disord.
2014 Dec;13(4):89-93. 10.12779/dnd.2014.13.4.89.
Comparison of Behavioral and Psychological Symptoms between Early and Late Onset Alzheimer's Disease According to the Progression of Dementia
- Affiliations
-
- 1Department of Psychiatry, Inje university paik-hospital, Busan, Korea.
- 2Department of Neurology, Pusan National University Hospital, Pusan National University School of Medicine and Medical Research Institute, Busan, Korea.
- 3Department of Psychology, Pusan National University, Busan, Korea. hch2144@yahoo.co.kr
- KMID: 2443071
- DOI: http://doi.org/10.12779/dnd.2014.13.4.89
Abstract
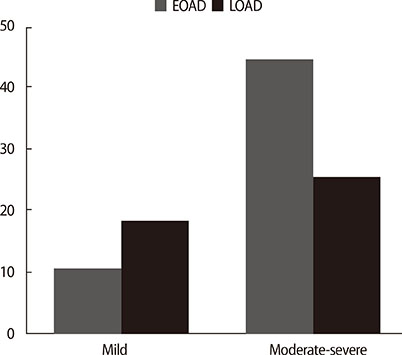
- The aim of this study was to investigate behavioral and psychological symptoms of dementia (BPSD) measured by caregiver-administered neuropsychiatric inventory (CGA-NPI) as a function of dementia severity in early onset (EOAD) versus late onset Alzheimer's disease (LOAD). A total of 113 patients with AD consisting of 49 patients with EOAD and 64 patients with LOAD were enrolled consecutively. General cognitive function and severity of dementia were assessed by the Korean version of mini-mental status examination and clinical dementia rating (CDR), respectively. In the mild stage (CDR 0.5-1), LOAD patients had a significantly higher total CGA-NPI score than EOAD patients. Subgroup analysis demonstrated that disinhibition and night-time behavior were more common and severe in the LOAD group than the EOAD group. However, in the moderate to severe stage (CDR 2-3), EOAD patients had a significantly higher total CGA-NPI score with higher subscores in hallucination, agitation/aggression, irritability/lability, aberrant motor behavior, and appetite/eating change. This study suggested that the heterogeneity of BPSD in AD might be accounted for by dementia severity as well as age at symptoms onset.
Keyword
Figure
Reference
-
1. Luscombe G, Brodaty H, Freeth S. Younger people with dementia: diagnostic issues, effects on carers and use of services. Int J Geriatr Psychiatry. 1998; 13:323–330.
Article2. Sampson EL, Warren JD, Rossor MN. Young onset dementia. Postgrad Med J. 2004; 80:125–139.
Article3. Amaducci LA, Rocca WA, Schoenberg BS. Origin of the distinction between Alzheimer's disease and senile dementia: how history can clarify nosology. Neurology. 1986; 36:1497–1499.
Article4. Heyman A, Wilkinson WE, Hurwitz BJ, Helms MJ, Haynes CS, Utley CM, et al. Early-onset Alzheimer's disease: clinical predictors of institutionalization and death. Neurology. 1987; 37:980–984.
Article5. Jacobs D, Sano M, Marder K, Bell K, Bylsma F, Lafleche G, et al. Age at onset of Alzheimer's disease: relation to pattern of cognitive dysfunction and rate of decline. Neurology. 1994; 44:1215–1220.6. Koedam EL, Lauffer V, van der Vlies AE, van der Flier WM, Scheltens P, Pijnenburg YA. Early-versus late-onset Alzheimer's disease: more than age alone. J Alzheimers Dis. 2010; 19:1401–1408.
Article7. Koss E, Edland S, Fillenbaum G, Mohs R, Clark C, Galasko D, et al. Clinical and neuropsychological differences between patients with earlier and later onset of Alzheimer's disease: A CERAD analysis, Part XII. Neurology. 1996; 46:136–141.
Article8. Bigio EH, Hynan LS, Sontag E, Satumtira S, White CL. Synapse loss is greater in presenile than senile onset Alzheimer disease: implications for the cognitive reserve hypothesis. Neuropathol Appl Neurobiol. 2002; 28:218–227.
Article9. Kim EJ, Cho SS, Jeong Y, Park KC, Kang SJ, Kang E, et al. Glucose metabolism in early onset versus late onset Alzheimer's disease: an SPM analysis of 120 patients. Brain. 2005; 128(Pt 8):1790–1801.
Article10. Mielke R, Herholz K, Grond M, Kessler J, Heiss WD. Differences of regional cerebral glucose metabolism between presenile and senile dementia of Alzheimer type. Neurobiol Aging. 1992; 13:93–98.
Article11. Finkel S. Introduction to behavioural and psychological symptoms of dementia (BPSD). Int J Geriatr Psychiatry. 2000; 15:Suppl 1. S2–S4.
Article12. Matsumoto T, Adachi H, Hirono N, Tanabe H. Caregiver burden associated with behavioral and psychological symptoms of dementia in elderly people in the local community. Dement Geriatr Cogn Disord. 2007; 23:219–224.
Article13. Hori K, Oda T, Asaoka T, Yoshida M, Watanabe S, Oyamada R, et al. First episodes of behavioral symptoms in Alzheimer's disease patients at age 90 and over, and early-onset Alzheimer's disease: comparison with senile dementia of Alzheimer's type. Psychiatry Clin Neurosci. 2005; 59:730–735.
Article14. Toyota Y, Ikeda M, Shinagawa S, Matsumoto T, Matsumoto N, Hokoishi K, et al. Comparison of behavioral and psychological symptoms in early-onset and late-onset Alzheimer's disease. Int J Geriatr Psychiatry. 2007; 22:896–901.
Article15. Hachinski VC, Iliff LD, Zilhka E, Du Boulay GH, McAllister VL, Marshall J, et al. Symon L. Cerebral blood flow in dementia. Arch Neurol. 1975; 32:632–637.16. Kang SJ, Choi SH, Lee BH, Jeong Y, Hahm DS, Han IW, et al. Caregiver-Administered Neuropsychiatric Inventory (CGA-NPI). J Geriatr Psychiatry Neurol. 2004; 17:32–35.
Article17. Kang Y, Na DL, Hahn S. A validitiy study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997; 15:300–308.18. Choi SH, Lee BH, Hahm DS, Jeong JH, Yoon SJ. Estimating the validity of the Korean version of Expanded Clinical Dementia Rating (CDR) scale. J Korean Neurol Assoc. 2001; 19:585–591.19. Lange RT, Hopp GA, Kang N. Psychometric properties and factor structure of the Neuropsychiatric Inventory Nursing Home version in an elderly neuropsychiatric population. Int J Geriatr Psychiatry. 2004; 19:440–448.
Article20. Cohen-Mansfield J, Marx MS, Rosenthal AS. A description of agitation in a nursing home. J Gerontol. 1989; 44(3):M77–M84.
Article21. Bruen PD, McGeown WJ, Shanks MF, Venneri A. Neuroanatomical correlates of neuropsychiatric symptoms in Alzheimer's disease. Brain. 2008; 131(Pt 9):2455–2463.
Article22. Tekin S, Mega MS, Masterman DM, Chow T, Garakian J, Vinters HV, et al. Orbitofrontal and anterior cingulate cortex neurofibrillary tangle burden is associated with agitation in Alzheimer disease. Ann Neurol. 2001; 49:355–361.
Article23. Trzepacz PT, Yu P, Bhamidipati PK, Willis B, Forrester T, Tabas L, et al. Frontolimbic atrophy is associated with agitation and aggression in mild cognitive impairment and Alzheimer's disease. Alzheimers Dement. 2013; 9:S95–S104.
Article24. Cho H, Seo SW, Kim JH, Kim C, Ye BS, Kim GH, et al. Changes in subcortical structures in early-versus late-onset Alzheimer's disease. Neurobiol Aging. 2013; 34:1740–1747.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Behavioral and Psychological Symptoms in Dementia(BPSD):Psychotic Symptoms
- Pharmacological Treatments of Behavioral Symptoms in Dementia
- The Functional Changes of Cognitive and Non-Cognitive Domains in the Progression of Alzheimers Disease
- Brain MRI Findings for the Patient with the Late Onset Schizophrenia: Comparison among Patients with the Early Onset Schizophrenia, Progressive Schizophrenia, Senile Dementia and Controls
- Atypical Antipsychotics for Behavioral and Psychological Symptoms in Alzheimer's Dementia