Dement Neurocogn Disord.
2016 Mar;15(1):20-23. 10.12779/dnd.2016.15.1.20.
Improvement of Frontal Lobe Dysfunctions in Neuromyelitis Optica after Treatment: A Case Report
- Affiliations
-
- 1Department of Neurology, Soonchunhyang University Gumi Hospital, Gumi, Korea.
- 2Department of Neurology, Veterans Health Service Medical Center, Seoul, Korea. astro76@naver.com
- KMID: 2442867
- DOI: http://doi.org/10.12779/dnd.2016.15.1.20
Abstract
- BACKGROUND
Neuromyelitis optica (NMO) is characterized by optic neuritis and longitudinally extensive transverse myelitis. Generally, the brain had been considered healthy in NMO patients, though recent studies have demonstrated that T2-weighted abnormalities may be observed in various brain regions. Logically, NMO brain lesions are localized at sites of high aquaporin-4 expression.
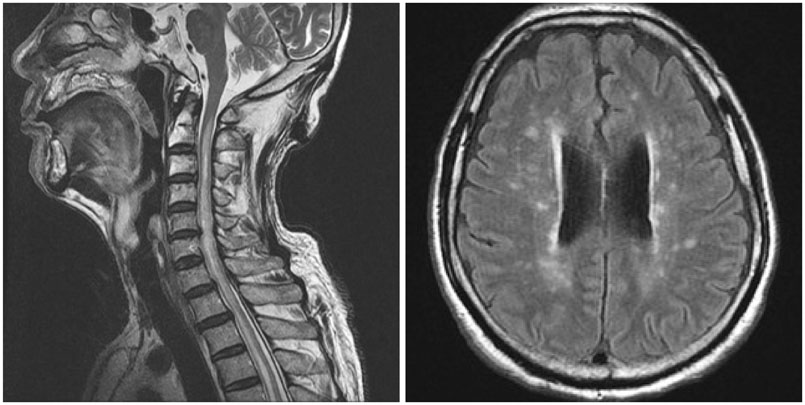
CASE REPORT
A 68-year-old right-handed man with dysuria, weakness in the bilateral upper and lower limbs, and decreased sensation of the lower extremities, was diagnosed with neuromyelitis optica. The patient was gradually speaking less, was showing reduced interest in hobbies, and had undergone changes in character and behavior. An examination was performed using the Seoul Neuropsychological Screening Battery (SNSB), which revealed that the profile of frontal lobe dysfunctions was prominent as compared with other cognitive domains. The patient was treated with prednisolone and azathioprine for about 1 year without recurrence, and showed prognostic improvement according to further SNSB testing.
CONCLUSIONS
Further studies are considered necessary in order to find the most effective medication regimen for improving cognitive functions in those accurately diagnosed with NMO, and to develop systematic treatment using even more diversified immune-related agents.
Keyword
MeSH Terms
Figure
Reference
-
1. Lee S, Kim BJ. Diagnosis and treatment of neuromyelitis optica. J Neurocrit Care. 2011; 4:Suppl 1. S38–S41.2. Lee CN, Park KW. Cognitive impairment in multiple sclerosis. J Mult Scler. 2013; 4:29–35.3. Ahn HJ, Chin J, Park A, Lee BH, Suh MK, Seo SW, et al. Seoul Neuropsychological Screening Battery-dementia version (SNSB-D): a useful tool for assessing and monitoring cognitive impairments in dementia patients. J Korean Med Sci. 2010; 25:1071–1076.
Article4. Pittock SJ, Lennon VA, Krecke K, Wingerchuk DM, Lucchinetti CF, Weinshenker BG. Brain abnormalities in neuromyelitis optica. Arch Neurol. 2006; 63:390–396.
Article5. Blanc F, Zéphir H, Lebrun C, Labauge P, Castelnovo G, Fleury M, et al. Cognitive functions in neuromyelitis optica. Arch Neurol. 2008; 65:84–88.
Article6. Saji E, Toyoshima Y, Yanagawa K, Nishizawa M, Kawachi I. Neuropsychiatric presentation of neuromyelitis optica spectrum disorders. Neurol. 2010; 74:A169.7. Blanc F, Noblet V, Jung B, Rousseau F, Renard F, Bourre B, et al. White matter atrophy and cognitive dysfunctions in neuromyelitis optica. PLoS One. 2012; 7:e33878.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postpartum Relapse of Neuromyelitis Optica Spectrum Disorder after a Long Period of Spontaneous Remission
- Neuromyelitis Optica (Devic's Disease)
- Steroid Unresponsive Neuromyelitis Optica Improved With Plasmapheresis
- Neuromyelitis Optica Spectrum Disorder Presenting with Pseudoathetosis
- A Case of Neuromyelitis Optica in Children