Anat Biol Anthropol.
2019 Mar;32(1):31-42. 10.11637/aba.2019.32.1.31.
Incidence Rate of Lumbosacral Transitional Vertebrae and Measurement of their Cross-sectional Areas of Vertebral Canal and Dural Sac Using Magnetic Resonance Imaging
- Affiliations
-
- 1Department of Anatomy, College of Medicine, Pusan National University, Korea. sikyoon@pusan.ac.kr
- 2Daegu Wooridul Spine Hospital, Korea.
- KMID: 2442782
- DOI: http://doi.org/10.11637/aba.2019.32.1.31
Abstract
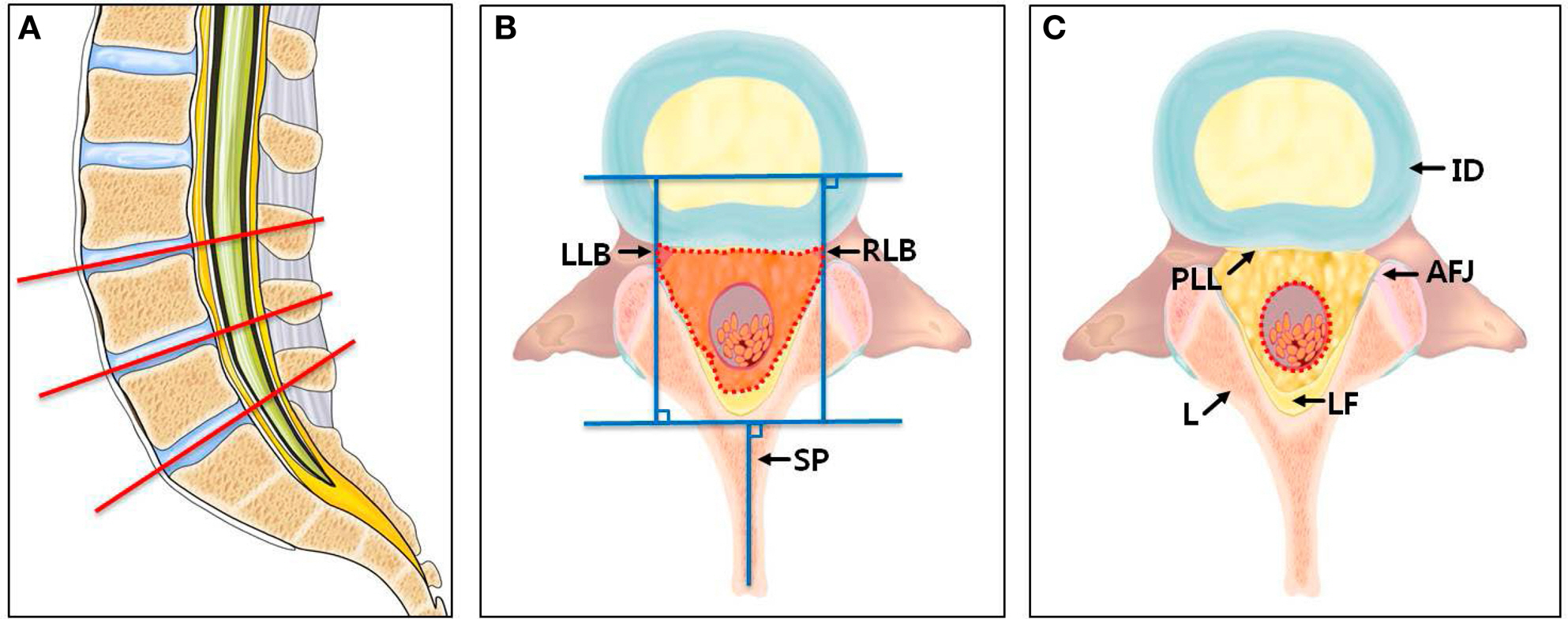
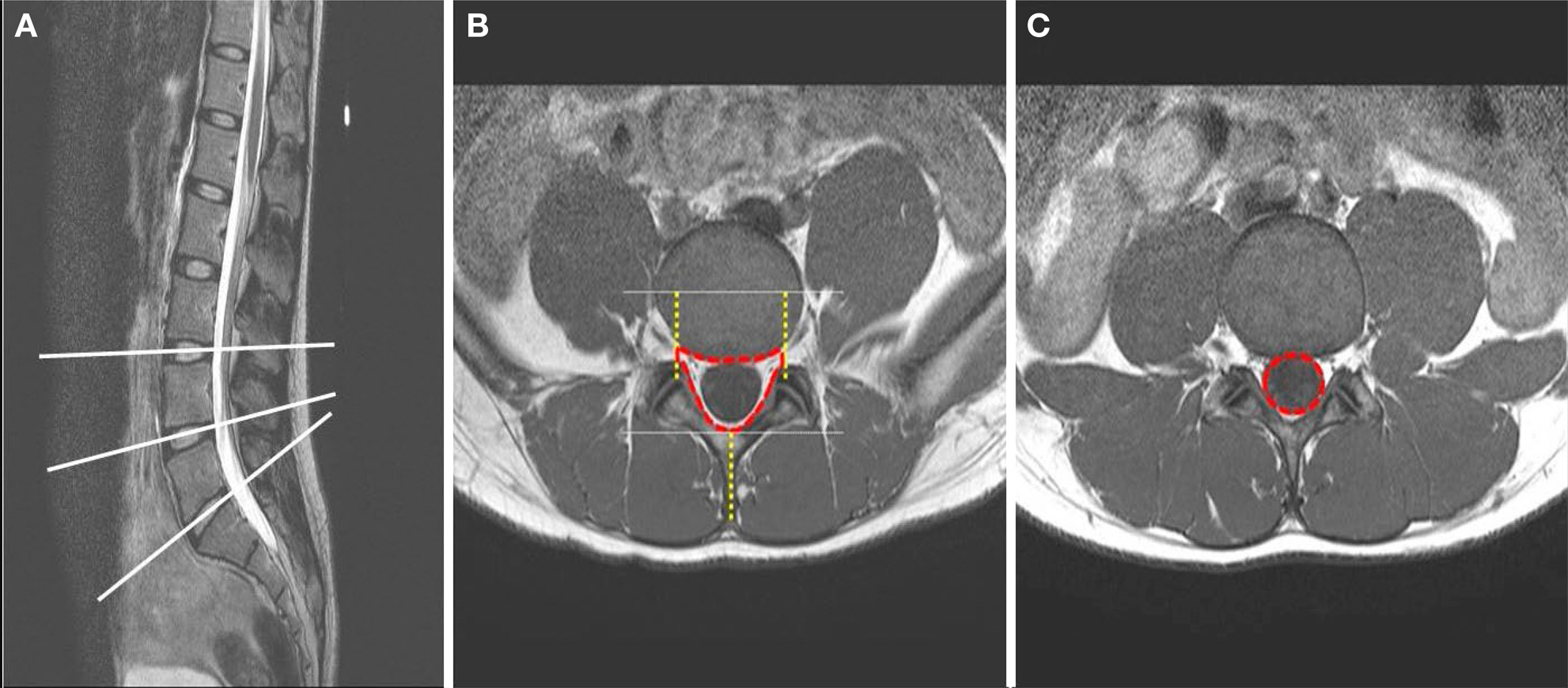
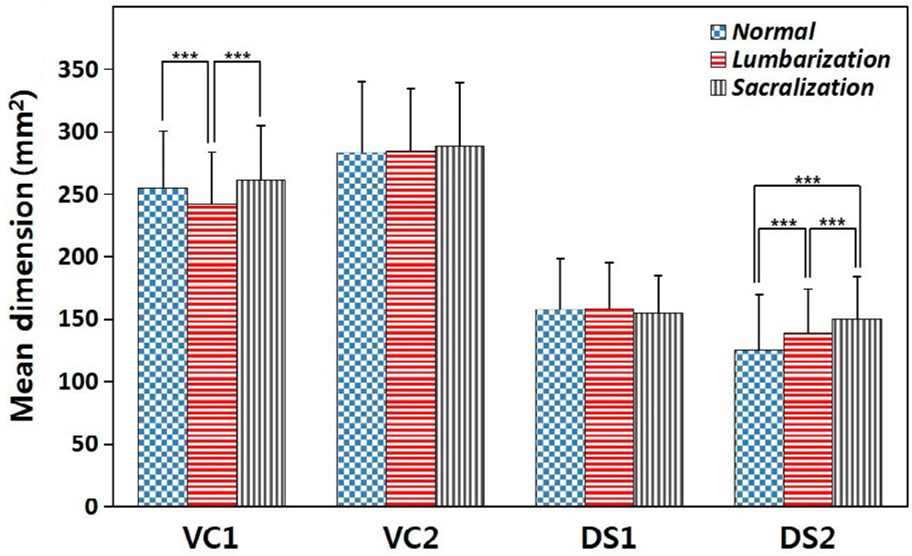
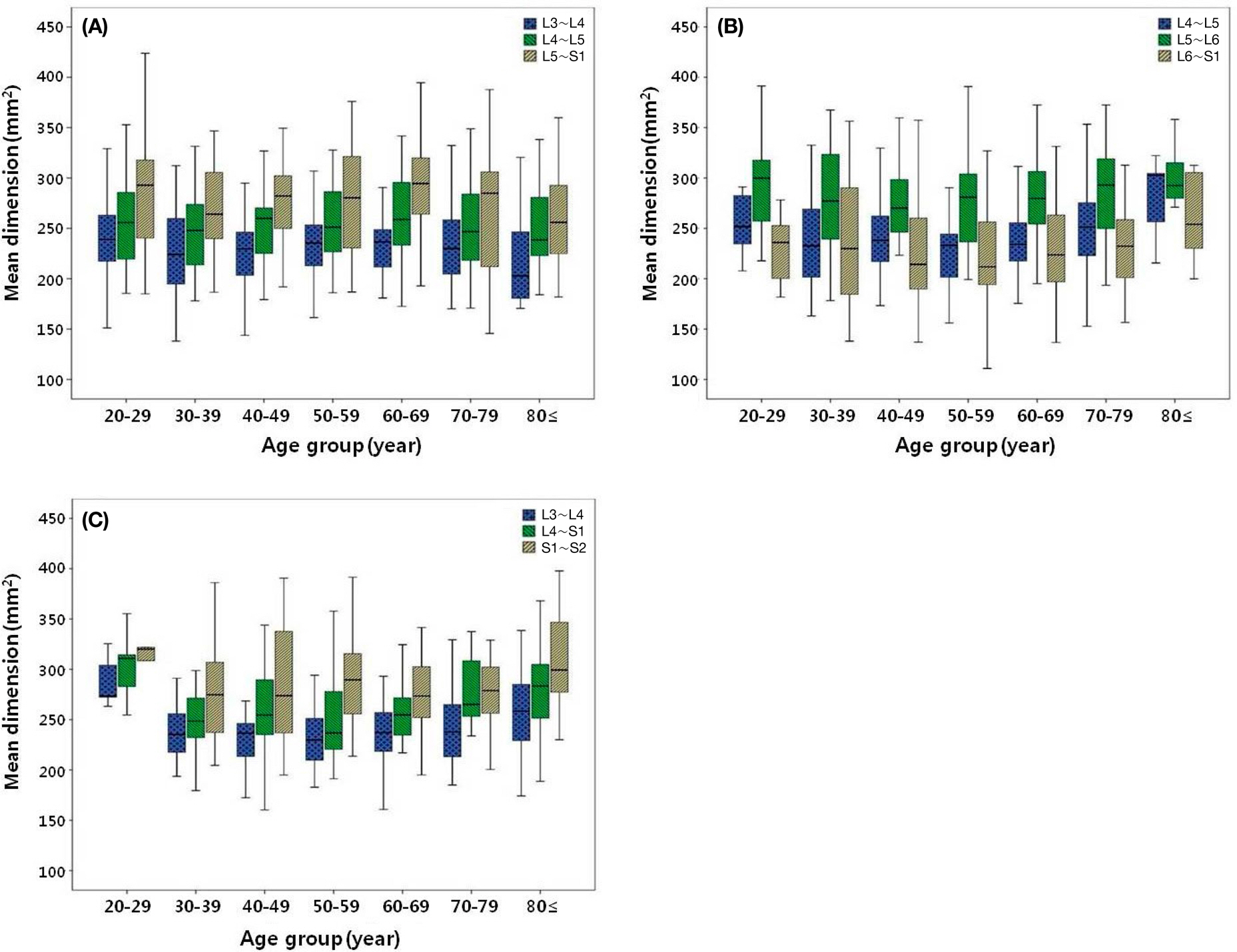
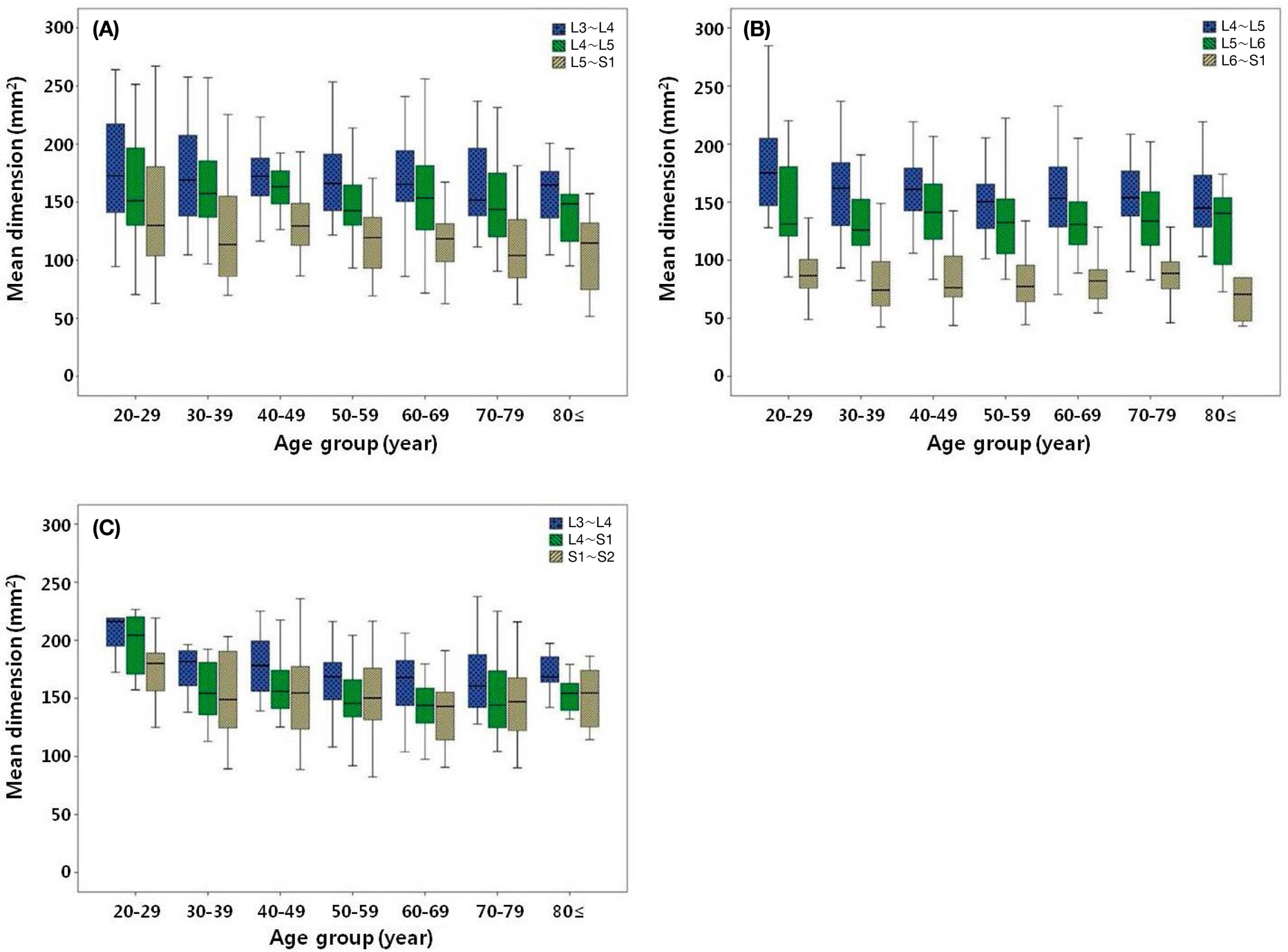
- Human lumbar spines usually consist of five vertebrae; however, some individuals have vertebral anomalies with four or six lumbar vertebrae because of the lumbarized first sacral vertebra (lumbarization) or the sacralized fifth lumbar vertebra (sacralization), respectively. These vertebral anomalies are called lumbosacral transitional vertebrae (LSTV). This study was performed to determine the prevalence of LSTV and to measure their cross-sectional areas of vertebral canal and dural sac in Koreans using magnetic resonance imaging. We evaluated 9709 patients, comprising of 5570 male and 4139 female subjects. The prevalence of LSTV in our study population was 3.77%, with a higher incidence of lumbarization than sacralization (p<0.05). The prevalence of lumbarization was 2.27%, with a higher rate in men (60.2%), while the incidence of sacralization was 1.50%, with a higher rate in women (62.7%). Differences between the groups were compared separately for the L4~L5 level which represents the level of lumbarization, and the L5~S1 level which represents the level of sacralization. When the vertebral canal cross-sectional areas (VCCSA) were compared between the normal and LSTV groups, the size of the vertebral canal was found to be smaller in the lumbarization group than in the normal group at the L4~L5 level (p<0.001), while there was no significant difference in VCCSA between the normal and LSTV groups at the L5~S1 level. However, when the dural sac cross-sectional areas were compared between the normal and LSTV groups, the size of the dural sac was larger in the LSTV group than in the normal group at the L5~S1 level (p<0.001). These results could be clinically used as one of the parameters for evaluating lumbar vertebral canal stenosis with LSTV in Koreans.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Quinlan JF, Duke D, Eustace S. Bertolotti's syndrome. A cause of back pain in young people. J Bone Joint Surg Br. 2006; 88:1183–6.2. Abe E, Sato K, Shimada Y, Okada K, Yan K, Mizutani Y. Anterior decompression of foraminal stenosis below a lumbosacral transitional vertebra. A case report. Spine (Phila Pa 1976). 1997; 22:823–6.3. Ichihara K, Taguchi T, Hashida T, Ochi Y, Murakami T, Kawai S. The treatment of far-out foraminal stenosis below a lumbosacral transitional vertebra: A report of two cases. J Spinal Disord Tech. 2004; 17:154–7.4. Delport EG, Cucuzzella TR, Kim N, Marley J, Pruitt C, Delport AG. Lumbosacral transitional vertebrae: incidence in a consecutive patient series. Pain Physician. 2006; 9:53–6.5. Tang M, Yang XF, Yang SW, Han P, Ma YM, Yu H, et al. Lumbosacral transitional vertebra in a population-based study of 5860 individuals: Prevalence and relationship to low back pain. Eur J Radiol. 2014; 83:1679–82.
Article6. Konin GP, Walz DM. Lumbosacral transitional vertebrae: Classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol. 2010; 31:1778–86.
Article7. Nardo L, Alizai H, Virayavanich W, Liu F, Hernandez A, Lynch JA, et al. Lumbosacral transitional vertebrae: association with low back pain. Radiology. 2012; 265:497–503.
Article8. Djurasovic M, Glassman SD, Carreon LY, Dimar JR 2nd. Contemporary management of symptomatic lumbar spinal stenosis. Orthop Clin North Am. 2010; 41:183–91.9. Frymoyer JW. Back pain and sciatica. N Engl J Med. 1988; 318:291–300.
Article10. Young S, Veerapen R, O'Laoire SA. Relief of lumbar canal stenosisusing multilevel subarticular fenestrations as an alternative to wide laminectomy: preliminary report. Neurosurgery. 1988; 23:628–33.11. Katz JN, Lipson SJ, Larson MG, Mclnnes JM, Fossel AH, Liang MH. The outcome of decompressive laminectomy for degenerative lumbar stenosis. J Bone Joint Surg. 1991; 73:809–16.
Article12. Masaryk TJ, Ross JS, Modie MT, Boumphrey F, Bohlman H, Wilber G. High-resolution MR imaging of sequestered lumbar intervertebral disks. AJR Am J Roentgenol. 1988; 150:115562.
Article13. Farshad-Amacker NA, Farshad M, Winklehner A, Andreisek G. MR imaging of degenerative disc disease. Eur J Radiol. 2015; 84:176876.
Article14. Becker SH, Arenson RL. Cost benefits of picture archiving and communication system. J Am Med Inform Assoc. 1994; 1:361–71.15. Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976). 1984; 9:493–5.
Article16. Seyfert S. Dermatome variations in patients with transitional vertebrae. J Neurol Neurosurg Psychiatry. 1997; 63:801–3.
Article17. Hahn PY, Strobel JJ, Hahn FJ. Verification of lumbosacral segments on MR images: Identification of transitional vertebrae. Radiology. 1992; 182:580–1.
Article18. Nakagawa T, Hashimoto K, Tsubakino T, Hoshikawa T, Inawashiro T, Tanaka Y. Lumbosacral transitional vertebrae cause spinal level misconception in surgeries for degenerative lumbar spine disorders. Tohoku J Exp Med. 2017; 242:223–8.
Article19. Bron JL, van Royen BJ, Wuisman PI. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg. 2007; 73:678–95.20. Hsieh CY, Vanderford JD, Moreau SR, Prong T. Lumbosa-cral transitional segments: classification, prevalence, and effect on disk height. J Manipulative Physiol Ther. 2000; 23:483–9.
Article21. Hughes RJ, Saifuddin A. Numbering of lumbosacral transitional vertebrae on MRI: role of the iliolumbar ligaments. AJR Am J Roentgenol. 2006; 187:W59–65.
Article22. Chithriki M, Jaibaji M, Steele RD. The anatomical relationship of the aortic bifurcation to the lumbar vertebrae: a MRI study. Surg Radiol Anat. 2002; 24:308–12.23. Kim JT, Bahk JH, Sung J. Influence of age and sex on the position of the conus medullaris and Tuffier's line in adults. Anesthesiology. 2003; 99:1359–63.
Article24. Tins BJ, Balain B. Incidence of numerical variants and transitional lumbosacral vertebrae on whole-spine MRI. Insights Imaging. 2016; 7:199–203.
Article25. Mahato NK. Relationship of sacral articular surfaces and gender with occurrence of lumbosacral transitional vertebrae. Spine J. 2011; 11:961–5.
Article26. Singh K, Samartzis D, Vaccaro AR, Nassr A, Andersson GB, Yoon ST, et al. Congenital lumbar spinal stenosis: a prospective, control-matched, cohort radiographic analysis. Spine J. 2005; 5:615–22.
Article27. Thomas SA. Spinal stenosis: history and physical examination. Phys Med Rehabil Clin N Am. 2003; 14:29–39.
Article28. Lipetz JS. Pathophysiology of inflammatory, degenerative, and compressive radiculopathies. Phys Med Rehabil Clin N Am. 2002; 13:439–49.
Article29. Aihara T, Takahashi K, Ogasawara A, Itadera E, Ono Y, Moriya H. Intervertebral disc degeneration associated with lumbosacral transitional vertebrae: a clinical and anatomical study. J Bone Joint Surg Br. 2005; 87:687–91.30. Vergauwen S, Parizel PM, van Breusegem L, Van Goethem JW, Nackaerts Y, Van den Hauwe L, et al. Distribution and incidence of degenerative spine changes in patients with a lumbosacral transitional vertebra. Eur Spine J. 1997; 6:168–72.
Article31. Oğuz H, Akkuş S, Tarhan S, Açikgözoğlu S, Kerman M. Measurement of spinal canal diameters in young subjects with lumbosacral transitional vertebra. Eur Spine J. 2002; 11:115–8.
Article32. Porter RW, Wicks M, Ottewell D. Measurement of the spinal canal by diagnostic ultrasound. J Bone Joint Surg Br. 1978; 60-B:481–4.
Article33. Dora C, Wȁlchli B, Elfering A, Gal I, Weishaupt D, Boos N. The significance of spinal canal dimensions in discriminating symptomatic from asymptomatic disc herniations. Eur Spine J. 2002; 11:575–81.
Article34. Korse NS, Kruit MC, Peul WC, Vleggeert-Lankamp CLA. Lumbar spinal canal MRI diameter is smaller in herniated disc cauda equina syndrome patients. PLoS One. 2017; 12:e0186148.
Article35. Sigmundsson FG, Kang XP, Jőnsson B, Strőmqvist B. Correlation between disability and MRI findings in lumbar spinal stenosis: a prospective study of 109 patients operated on by decompression. Acta Orthop. 2011; 82:204–10.36. Malmivaara A, Slȁtis P, Heliővaara M, Sainio P, Kinnunen H, Kankare J, et al. Surgical or nonoperative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine. 2007; 32:1–8.37. Luoma K, Vehmas T, Raininko R, Luukkonen R, Riihimȁki H. Lumbosacral transitional vertebra relation to disc degeneration and low back pain. Spine (Phila Pa 1976). 2004; 29:200–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Morphological Analysis of the Cervical Spinal Cord, Dural Tube, and Spinal Canal by Magnetic Resonance Imaging in Normal Korean Adults
- Prevalence of Lumbosacral Transitional Vertebra in Individuals with Low Back Pain: Evaluation Using Plain Radiography and Magnetic Resonance Imaging
- Variations of End Level of the Dural Sac
- Inadvertent Dural Puncture during Caudal Approach by the Introducer Needle for Epidural Adhesiolysis Caused by Anatomical Variation
- Marfan syndrome and symptomatic dural ectasia: A case report and literature review