Clin Exp Otorhinolaryngol.
2018 Dec;11(4):301-308. 10.21053/ceo.2018.00178.
Body Surface Area Is Not a Reliable Predictor of Tracheal Tube Size in Children
- Affiliations
-
- 1Department of Anesthesiology and Reanimation, Hacettepe University School of Medicine, Ankara, Turkey. filizuzumcugil@hotmail.com
- 2Department of Radiology, Karabük University, Karabük, Turkey.
- KMID: 2439858
- DOI: http://doi.org/10.21053/ceo.2018.00178
Abstract
OBJECTIVES
The age-based Cole formula has been employed for the estimation of endotracheal tube (ETT) size due to its ease of use, but may not appropriately consider growth rates among children. Child growth is assessed by calculating the body surface area (BSA). The association between the outer diameter of an appropriate uncuffed-endotracheal-tube (ETT-OD) and the BSA values of patients at 24-96 months of age was our primary outcome.
METHODS
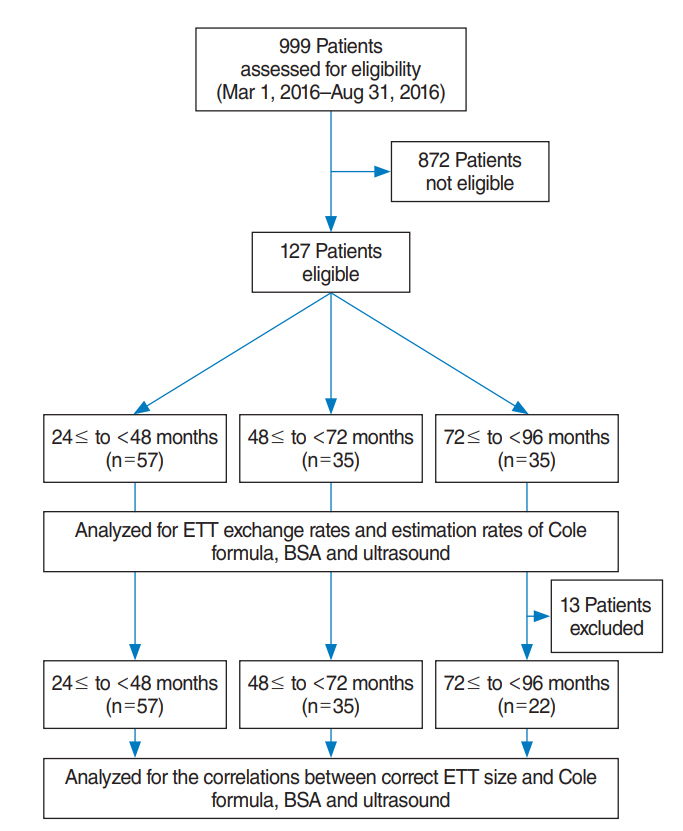
Cole formula, BSA, age, height, weight and ultrasound measurement of subglottic-transverse-diameter were evaluated for correlations with correct uncuffed ETT-OD. The Cole formula, BSA, and ultrasound measurements were analyzed for estimation rates in all patients and age subgroups. The maximum allowed error for the estimation of ETT-OD was ≤0.3 mm. Patients' tracheas were intubated with tubes chosen by Cole formula and correct ETT-OD values were determined using leak test. ETT exchange rates were recorded.
RESULTS
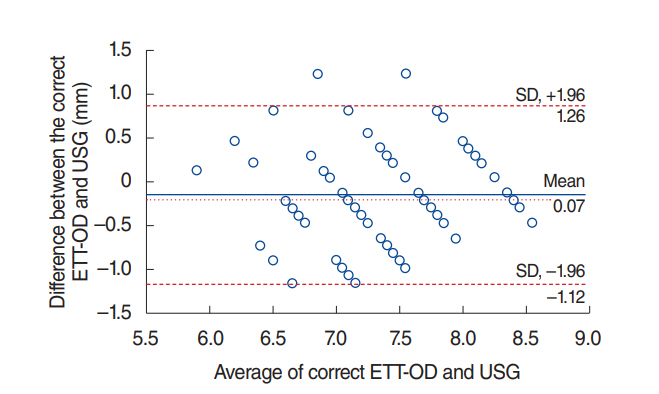
One-hundred twenty-seven patients were analyzed for the determination of estimation rates. Thirteen patients aged ≥72 months were intubated with cuffed ETT-OD of 8.4 mm and were accepted to need uncuffed ETT-OD >8.4 mm in order to be included in estimation rates, but excluded from correlations for size analysis. One-hundred fourteen patients were analyzed for correlations between correct ETT-OD (determined by the leak test) and outcome parameters. Cole formula, ultrasonography, and BSA had similar correct estimation rates. All three parameters had higher underestimation rates as age increased.
CONCLUSION
The Cole formula, BSA, and ultrasonography had similar estimation rates in patients aged ≥24 to ≤96 months. BSA had a correct estimation rate of 40.2% and may not be reliable in clinical practice to predict uncuffed-ETT-size.
Figure
Reference
-
1. Sirisopana M, Saint-Martin C, Wang NN, Manoukian J, Nguyen LH, Brown KA. Novel measurements of the length of the subglottic airway in infants and young children. Anesth Analg. 2013; Aug. 117(2):462–70.
Article2. Wani TM, Bissonnette B, Rafiq Malik M, Hayes D Jr, Ramesh AS, Al Sohaibani M, et al. Age-based analysis of pediatric upper airway dimensions using computed tomography imaging. Pediatr Pulmonol. 2016; Mar. 51(3):267–71.
Article3. Dalal PG, Murray D, Messner AH, Feng A, McAllister J, Molter D. Pediatric laryngeal dimensions: an age-based analysis. Anesth Analg. 2009; May. 108(5):1475–9.
Article4. Marciniak B. Growth and development. In : Cote CJ, Lerman J, Anderson BJ, editors. A practice of anesthesia for infants and children. 5th ed. Philadelphia (PA): Elsevier Saunders;2013. p. 7–21.5. Schramm C, Knop J, Jensen K, Plaschke K. Role of ultrasound compared to age-related formulas for uncuffed endotracheal intubation in a pediatric population. Paediatr Anaesth. 2012; Aug. 22(8):781–6.
Article6. Shibasaki M, Nakajima Y, Ishii S, Shimizu F, Shime N, Sessler DI. Prediction of pediatric endotracheal tube size by ultrasonography. Anesthesiology. 2010; Oct. 113(4):819–24.
Article7. Bae JY, Byon HJ, Han SS, Kim HS, Kim JT. Usefulness of ultrasound for selecting a correctly sized uncuffed tracheal tube for paediatric patients. Anaesthesia. 2011; Nov. 66(11):994–8.
Article8. Kim EJ, Kim SY, Kim WO, Kim H, Kil HK. Ultrasound measurement of subglottic diameter and an empirical formula for proper endotracheal tube fitting in children. Acta Anaesthesiol Scand. 2013; Oct. 57(9):1124–30.
Article9. Hofer CK, Ganter M, Tucci M, Klaghofer R, Zollinger A. How reliable is length-based determination of body weight and tracheal tube size in the paediatric age group? The Broselow tape reconsidered. Br J Anaesth. 2002; Feb. 88(2):283–5.
Article10. Daugherty RJ, Nadkarni V, Brenn BR. Endotracheal tube size estimation for children with pathological short stature. Pediatr Emerg Care. 2006; Nov. 22(11):710–7.11. Neunhoeffer F, Wahl T, Hofbeck M, Renk H, Esslinger M, Hanelt M, et al. A new method for determining the insertion depth of tracheal tubes in children: a pilot study. Br J Anaesth. 2016; Mar. 116(3):393–7.
Article12. Mosteller RD. Simplified calculation of body-surface area. N Engl J Med. 1987; Oct. 317(17):1098.
Article13. Hamill PV, Drizd TA, Johnson CL, Reed RB, Roche AF. NCHS growth curves for children birth-18 years: United States. Vital Health Stat 11. 1977; Nov. (165):i–v. 1–74.14. Prasad A, Yu E, Wong DT, Karkhanis R, Gullane P, Chan VW. Comparison of sonography and computed tomography as imaging tools for assessment of airway structures. J Ultrasound Med. 2011; Jul. 30(7):965–72.
Article15. Stafrace S, Engelhardt T, Teoh WH, Kristensen MS. Essential ultrasound techniques of the pediatric airway. Paediatr Anaesth. 2016; Feb. 26(2):122–31.
Article16. Manickavasagam J, Yapa S, Bateman ND, Thevasagayam MS. Congenital familial subglottic stenosis: a case series and review of literature. Int J Pediatr Otorhinolaryngol. 2014; Feb. 78(2):359–62.
Article17. Gnagi SH, Howard BE, Anderson C, Lott DG. Idiopathic subglottic and tracheal stenosis: a survey of the patient experience. Ann Otol Rhinol Laryngol. 2015; Sep. 124(9):734–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of the Size of the Uncuffed Tracheal Tube on Verifying Tube Position by Auscultation in Children
- Relation of Left Ventricular Mass to Body Size and Left Ventricular Wall Stress in Normal Adults
- Proper Depth of Tracheal Intubation in Korean Children
- Difficult endotracheal intubation secondary to tracheal deviation and stenosis in a patient with severe kyphoscoliosis: a case report
- Association of Oversized Tracheal Tubes and Cuff Overinsufflation With Postintubation Tracheal Ruptures