Pediatr Infect Vaccine.
2018 Apr;25(1):45-49. 10.14776/piv.2018.25.1.45.
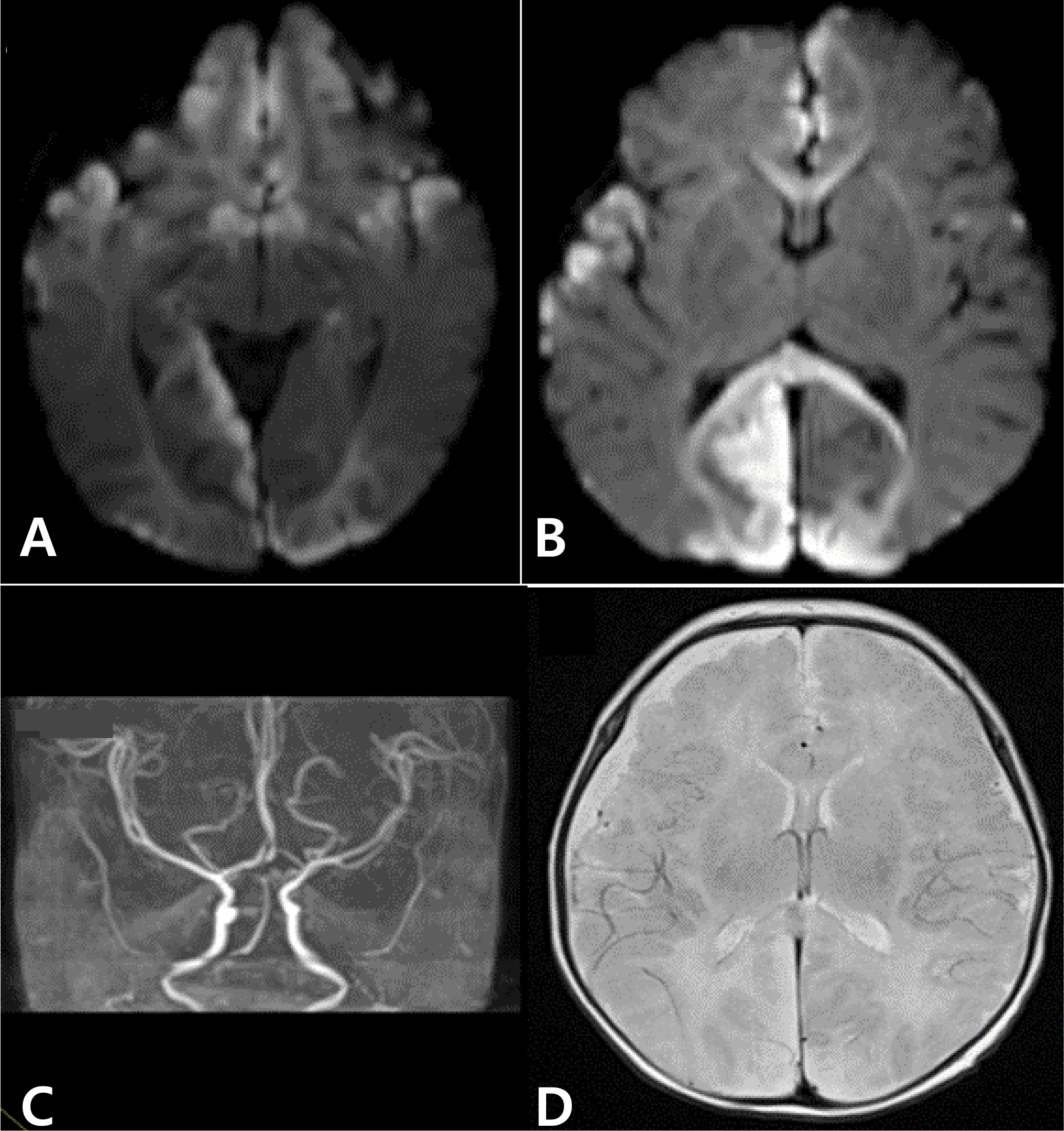
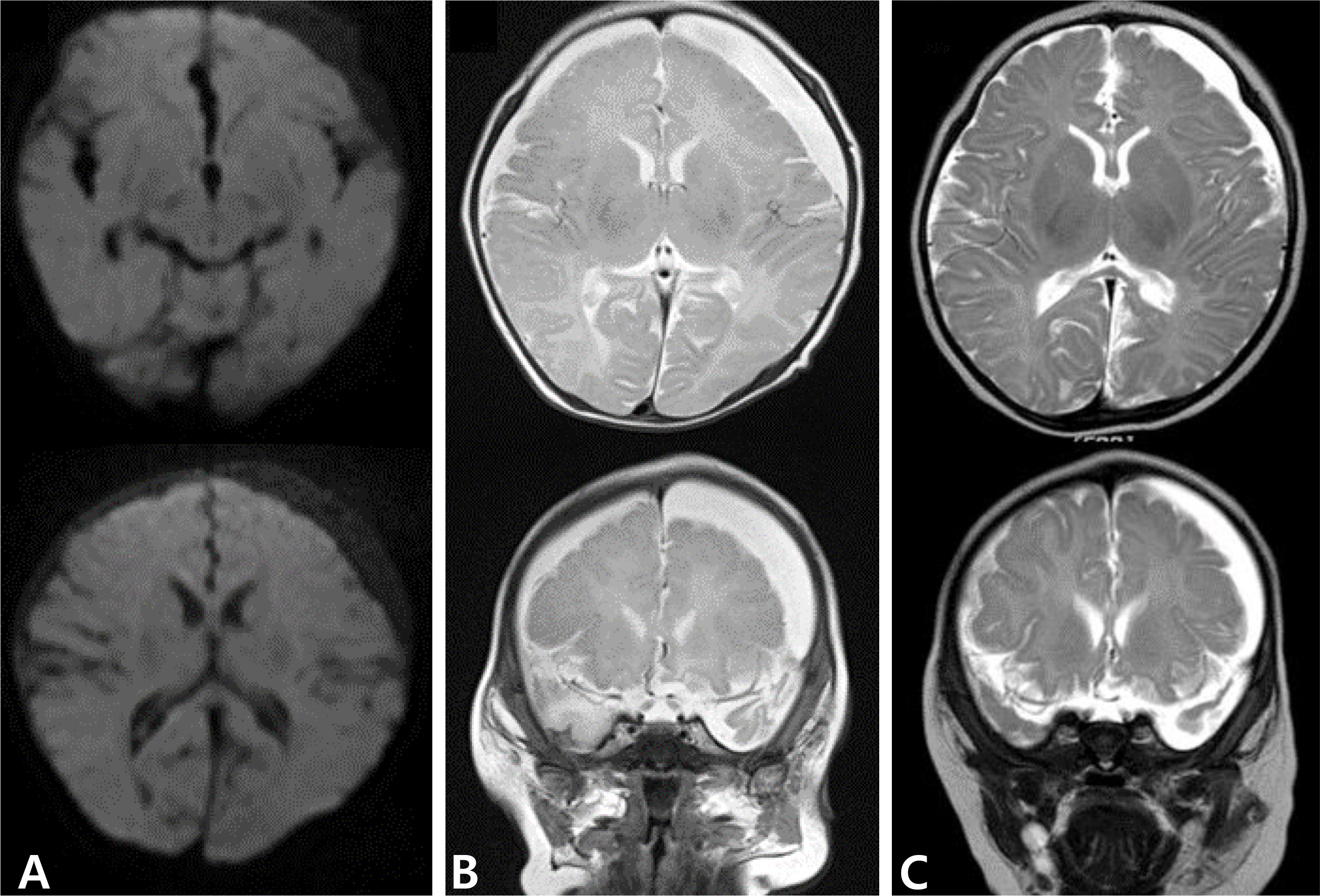
Late-Onset Group B Streptococcal Meningitis Complicated with Extensive Cerebral Infarction
- Affiliations
-
- 1Department of Pediatrics, Hallym University Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, the Republic of Korea. soohanchoi@hallym.or.kr
- 2Department of Pediatrics, Gil Medical Center, Gachon University College of Medicine, Incheon, the Republic of Korea.
- KMID: 2438753
- DOI: http://doi.org/10.14776/piv.2018.25.1.45
Abstract
- Group B streptococcus (GBS) is the leading cause of neonatal morbidity and mortality. Late-onset GBS disease commonly manifests as occult bacteremia or meningitis. Approximately 50% of survivors of late-onset meningitis have long-term neurologic sequelae. Cerebrovascular complications are often associated with unfavorable clinical outcomes of GBS meningitis. There have been a few reports of cerebral infarction accompanied by GBS meningitis. We report a 29-day-old girl with severe, widespread cerebral infarction due to late-onset GBS meningitis. Isolated GBS strain from this patient was serotype III, ST-19. Currently, she has cortical blindness and significant developmental delay.
MeSH Terms
Figure
Reference
-
References
1. Pannaraj PS, Baker CJ. Group B streptococcal infections. Cherry JD, Demmler-Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ, editors. editors.Feigin and Cherry's Textbook of pediatric infectious diseases. 7th Ed.Philadelphia: Saunders Elsevier;2014. p. 1153–69.
Article2. Lachenauer CS, Wessels MR. Group B streptococcus. Kliegman RM, Nelson WE, editors. editors.Nelson textbook of pediatrics. 20th Ed.Philadelphia: Elsevier;2016. p. 1337–41.
Article3. Hernandez MI, Sandoval CC, Tapia JL, Mesa T, Escobar R, Huete I, et al. Stroke patterns in neonatal group B streptococcal meningitis. Pediatr Neurol. 2011; 44:282–8.4. deVeber GA, Kirton A, Booth FA, Yager JY, Wirrell EC, Wood E, et al. Epidemiology and outcomes of arterial ischemic stroke in children: the Canadian Pediatric Ischemic Stroke Registry. Pediatr Neurol. 2017; 69:58–70.
Article5. Pryde K, Walker WT, Hollingsworth C, Haywood P, Baird J, Hussey M, et al. Stroke in paediatric pneumococcal meningitis: a cross-sectional population-based study. Arch Dis Child. 2013; 98:647–9.
Article6. Lehman LL, Rivkin MJ. Perinatal arterial ischemic stroke: presentation, risk factors, evaluation, and outcome. Pediatr Neurol. 2014; 51:760–8.
Article7. Cho HK, Nam HN, Cho HJ, Son DW, Cho YK, Seo YH, et al. Serotype distribution of invasive group B streptococcal diseases in infants at two university hospitals in Korea. Pediatr Infect Vaccine. 2017; 24:79–86.
Article8. Jones N, Bohnsack JF, Takahashi S, Oliver KA, Chan MS, Kunst F, et al. Multilocus sequence typing system for group B streptococcus. J Clin Microbiol. 2003; 41:2530–6.
Article9. Pintye J, Saltzman B, Wolf E, Crowell CS. Risk factors for late-onset group B streptococcal disease before and after implementation of universal screening and intrapartum antibiotic prophylaxis. J Pediatric Infect Dis Soc. 2016; 5:431–8.
Article10. Cho HK, Lee H, Kang JH, Kim KN, Kim DS, Kim YK, et al. The causative organisms of bacterial meningitis in Korean children in 1996–2005. J Korean Med Sci. 2010; 25:895–9.
Article11. Chong Y, Lee K, Kwon OH, Nahm CH, Murai T, Inazumi Y. Trend of isolation and serotypes of group B streptococci in Korea. Yonsei Med J. 1993; 34:78–83.
Article12. Uh Y, Jang IH, Yoon KJ, Lee CH, Kwon JY, Kim MC. Colonization rates and serotypes of group B streptococci isolated from pregnant women in a Korean tertiary hospital. Eur J Clin Microbiol Infect Dis. 1997; 16:753–6.
Article13. Hong JS, Choi CW, Park KU, Kim SN, Lee HJ, Lee HR, et al. Genital group B Streptococcus carrier rate and serotype distribution in Korean pregnant women: implications for group B streptococcal disease in Korean neonates. J Perinat Med. 2010; 38:373–7.
Article14. Lee BK, Song YR, Kim MY, Yang JH, Shin JH, Seo YS, et al. Epidemiology of group B streptococcus in Korean pregnant women. Epidemiol Infect. 2010; 138:292–8.
Article15. Park KH, Kim KH, Kang JH, Kim KN, Kim DS, Kim YK, et al. Current status and clinical presentations of invasive neonatal Group B streptococcal infections in Korea. Pediatr Int. 2011; 53:236–9.
Article16. Tibussek D, Sinclair A, Yau I, Teatero S, Fittipaldi N, Richardson SE, et al. Late-onset group B streptococcal meningitis has cerebrovascular complications. J Pediatr. 2015; 166:1187–92.e1.
Article17. Chang CJ, Chang WN, Huang LT, Chang YC, Huang SC, Hung PL, et al. Cerebral infarction in perinatal and childhood bacterial meningitis. QJM. 2003; 96:755–62.
Article18. Tazi A, Disson O, Bellais S, Bouaboud A, Dmytruk N, Dramsi S, et al. The surface protein HvgA mediates group B streptococcus hypervirulence and meningeal tropism in neonates. J Exp Med. 2010; 207:2313–22.
Article19. Kang HM, Lee HJ, Lee H, Jo DS, Lee HS, Kim TS, et al. Genotype characterization of group B streptococcus isolated from infants with invasive diseases in South Korea. Pediatr Infect Dis J. 2017; 36:e242–7.
Article20. Boelman C, Shroff M, Yau I, Bjornson B, Richrdson S, deVeber G, et al. Antithrombotic therapy for secondary stroke prevention in bacterial meningitis in children. J Pediatr. 2014; 165:799–806.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Late Onset Group B Streptococcal Sepsis with the Complication of Subclavian Vein Catheterization
- A Case of Cryptococcal Meningitis Presenting as Multiple Cerebral Infarctions
- Clinical study on 12 cases of neonatal group B ?hemolytic streptococcal meningitis
- A Case of Bacterial Meningitis Associated with Cerebral Infarction and Arterial Stenosis-Transcranial Doppler Findings
- A Case of Cerebral Infarction and Subdural Hemorrhage after Aseptic Meningitis