Anesth Pain Med.
2018 Oct;13(4):463-467. 10.17085/apm.2018.13.4.463.
Pharyngeal reperforation following incentive spirometry: A case report
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, Pusan National University Hospital, Busan, Korea. ccarrot@pusan.ac.kr
- KMID: 2436009
- DOI: http://doi.org/10.17085/apm.2018.13.4.463
Abstract
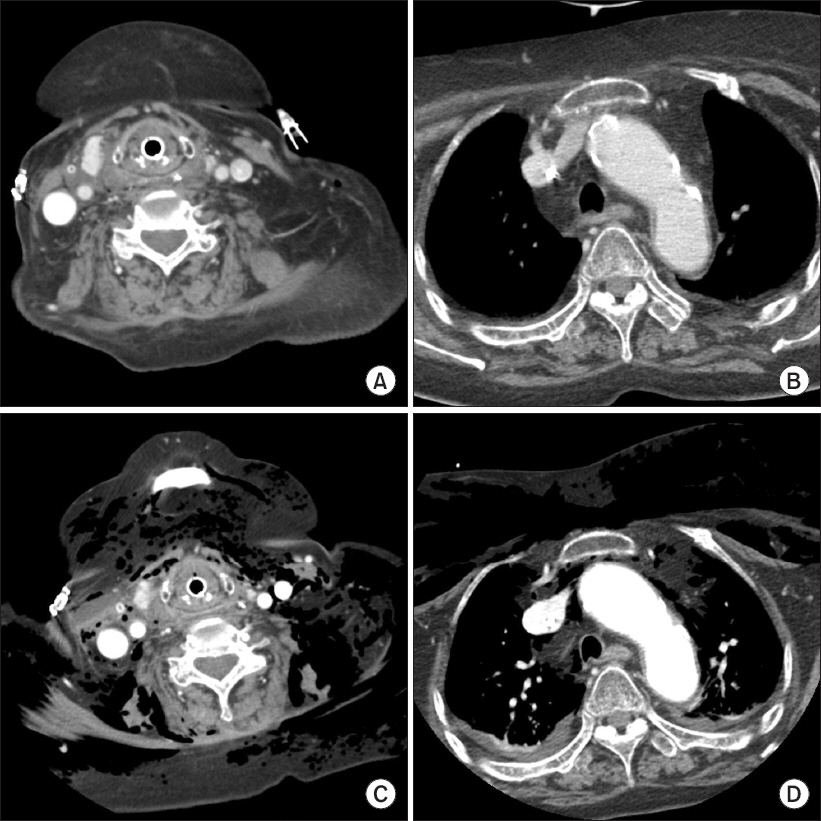
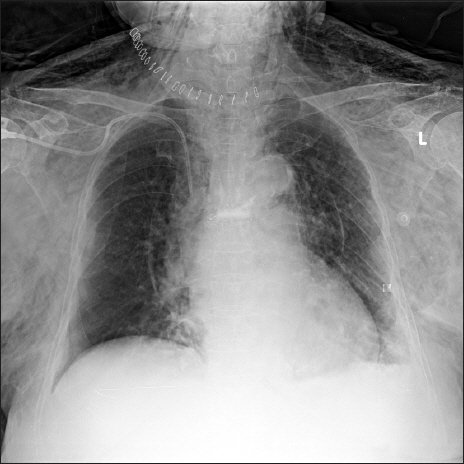
- Despite its widespread use, complication of incentive spirometry has been rarely reported. We report a case of pharyngeal reperforation following incentive spirometry. A 75-year-old female, had a history of long-term steroid use, entered the intensive care unit for maintenance of mechanical ventilation following surgical repair of a pharyngeal perforation. After ventilator weaning, incentive spirometry was implemented on postoperative day 4. Immediately after incentive spirometry use, patient's neck began to swell, and subcutaneous emphysema was palpated. Pharyngeal reperforation was suspected on neck computed tomography, and emergency surgery was performed. Surgery revealed a 3-cm long rupture from the hypopharynx to the esophagus. The causes were thought to be delayed wound healing due to long-term steroid use and a sudden increase in pharyngeal pressure due to incentive spirometry. In conclusion, particular attention should be paid when using incentive spirometry after head and neck surgery in patients with a history of long-term steroid use.
Keyword
MeSH Terms
Figure
Reference
-
REFERENCE
1. Restrepo RD, Wettstein R, Wittnebel L, Tracy M. Incentive spirometry:2011. Respir Care. 2011; 56:1600–4. DOI: 10.4187/respcare.01471. PMID: 22008401.2. Sawant AA, Shinde N. Effects of diaphragmatic weight training versus incentive spirometry in patients weaned from mechanical ventilation.- A pilot study. Indian J Basic Appl Med Res. 2014; 3:24–30.3. Reid WD, Chung F. Clinical management notes and case histories in cardiopulmonary physical therapy. Thorofare, Slack Incorporated. 2004; 79–84.4. Seikaly H, Kuzon WM Jr, Gullane PJ, Herman SJ. Pulmonary atelectasis after reconstruction with pectoralis major flaps. Arch Otolaryngol Head Neck Surg. 1990; 116:575–7. DOI: 10.1001/archotol.1990.01870050075010. PMID: 2328115.5. Schuller DE, Daniels RL, King M, Houser S. Analysis of frequency of pulmonary atelectasis in patients undergoing pectoralis major musculocutaneous flap reconstruction. Head Neck. 1994; 16:25–9. DOI: 10.1002/hed.2880160107. PMID: 8125785.6. Tan AK. Incentive spirometry for tracheostomy and laryngectomy patients. J Otolaryngol. 1995; 24:292–4. PMID: 8537988.7. Schepens T, Verbrugghe W, Dams K, Corthouts B, Parizel PM, Jorens PG. The course of diaphragm atrophy in ventilated patients assessed with ultrasound:a longitudinal cohort study. Crit Care. 2015; 19:422. DOI: 10.1186/s13054-015-1141-0. PMID: 26639081. PMCID: PMC4671211.8. do Nascimento P Junior, Módolo NS, Andrade S, Guimarães MM, Braz LG, El Dib R. Incentive spirometry for prevention of postoperative pulmonary complications in upper abdominal surgery. Cochrane Database Syst Rev. 2014; (2):CD006058. DOI: 10.1002/14651858.CD006058.pub3.9. Cassidy MR, Rosenkranz P, McCabe K, Rosen JE, McAneny D. I COUGH:reducing postoperative pulmonary complications with a multidisciplinary patient care program. JAMA Surg. 2013; 148:740–5. DOI: 10.1001/jamasurg.2013.358. PMID: 23740240.10. Kim SW, Kang HH, Kang JY, Kim SK, Lee BY, Lee SH, et al. A case of pneumomediastinum and parapneumonic effusions following pharyngeal perforation caused by shouting. Yonsei Med J. 2014; 55:270–2. DOI: 10.3349/ymj.2014.55.1.270. PMID: 24339317. PMCID: PMC3874924.11. Roh JL, Park CI. Spontaneous pharyngeal perforation after forceful vomiting:the difference from classic Boerhaave's syndrome. Clin Exp Otorhinolaryngol. 2008; 1:174–6. DOI: 10.3342/ceo.2008.1.3.174. PMID: 19434253. PMCID: PMC2671744.12. Wake M, Stansbie M, Thompson H. Spontaneous perforation of the pharynx/esophagus. Ear Nose Throat J. 1991; 70:318–20. PMID: 1914957.13. Wang AS, Armstrong EJ, Armstrong AW. Corticosteroids and wound healing:clinical considerations in the perioperative period. Am J Surg. 2013; 206:410–7. DOI: 10.1016/j.amjsurg.2012.11.018. PMID: 23759697.14. Ismael H, Horst M, Farooq M, Jordon J, Patton JH, Rubinfeld IS. Adverse effects of preoperative steroid use on surgical outcomes. Am J Surg. 2011; 201:305–8. discussion 308-9. DOI: 10.1016/j.amjsurg.2010.09.018. PMID: 21367368.15. Gorosh LR, Ingaramo O, Nelson D, Vohra M, Ciccolo ML. Spontaneous tracheal rupture:a case report. J Emerg Med. 2014; 46:31–3. DOI: 10.1016/j.jemermed.2013.05.062. PMID: 24054884.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of preoperative incentive spirometry on fentanyl-induced cough: a prospective, randomized, controlled study
- Effects of Incentive Spirometry on Respiratory Motion in Healthy Subjects Using Cine Breathing Magnetic Resonance Imaging
- The Effect of Deep Breathing Exercise and Incentive Spirometry to Prevent Postoperative Pulmonary Complications after Abdominal Surgery in Geriatric Patients
- The Effects of Deep Breathing Methods on Pulmonary Ventilatory Function of Pneumothorax Patients undergoing a Thoracotomy
- Use of Office Spirometry in Primary-Care Clinics