Investig Clin Urol.
2019 Jan;60(1):40-45. 10.4111/icu.2019.60.1.40.
Transvaginal ultrasound guided trigone and bladder injection: A cadaveric feasibility study for a novel route of intradetrusor chemodenervation
- Affiliations
-
- 1Department of Urology, Stanford University School of Medicine, Stanford, CA, USA. rsyan@stanford.edu
- 2Department of Surgery, Stanford University School of Medicine, Stanford, CA, USA.
- KMID: 2434624
- DOI: http://doi.org/10.4111/icu.2019.60.1.40
Abstract
- PURPOSE
OnabotulinumtoxinA (BTX) detrusor chemodenervation is an efficacious third-line treatment for overactive bladder. Despite high clinical efficacy rates for BTX injection, many patients refuse initial or repeat treatment due to the invasiveness of the cystoscopic route of delivery. We assess the feasibility of injecting the trigone and posterior bladder wall via a transvaginal route under ultrasound guidance using a human cadaveric model.
MATERIALS AND METHODS
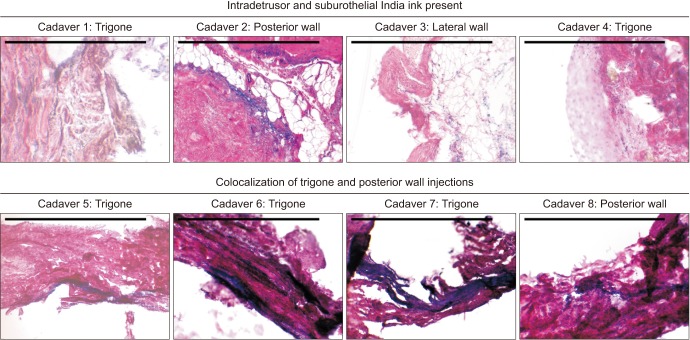
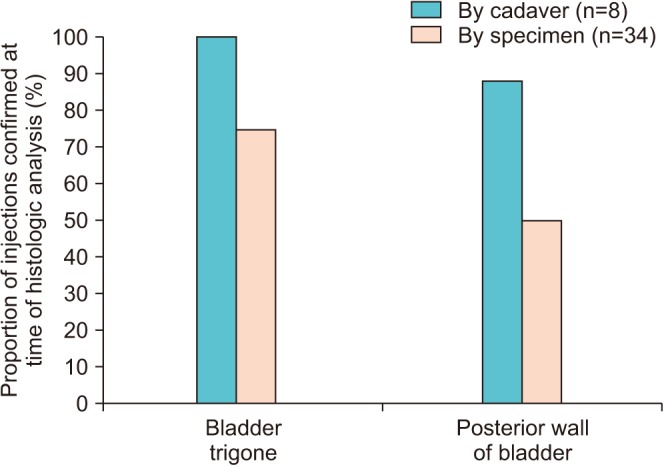
Eight de-identified anonymous fresh female deceased donor cadaver pelvises were placed in supine split leg position. A transvaginal ultrasound probe guided injections of India ink into the trigone in 3 sites and the posterior wall in 2 sites. Full thickness bladder biopsies were then obtained and histologic analysis was performed to confirm presence of India ink in the detrusor layer.
RESULTS
The mean time from day of death was 11.0 days (range, 4.0-23.0 days). Three to five bladder biopsies were obtained per cadaver, for a total of 34 specimens (20 trigone, 14 posterior wall). Histologic analysis revealed presence of India ink within the detrusor layer in 8/8 (100.0%) of cadavers. The surgeon's perception of appropriate targeting under ultrasound guidance was confirmed in 8/8 cadavers (100.0%) involving the bladder trigone, and 7/8 (87.5%) involving the posterior wall. Of injections that were believed to have appropriately targeted the detrusor layer, 22/34 specimens (64.7%) demonstrated the presence of India ink under histologic analysis.
CONCLUSIONS
Intradetrusor injection of the bladder trigone and posterior wall under transvaginal ultrasound guidance is feasible and has acceptable accuracy.
Keyword
MeSH Terms
Figure
Reference
-
1. Sun Y, Luo D, Tang C, Yang L, Shen H. The safety and efficiency of onabotulinumtoxinA for the treatment of overactive bladder: a systematic review and meta-analysis. Int Urol Nephrol. 2015; 47:1779–1788. PMID: 26433883.
Article2. Gormley EA, Lightner DJ, Burgio KL, Chai TC, Clemens JQ, Culkin DJ, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline. J Urol. 2012; 188(6 Suppl):2455–2463. PMID: 23098785.
Article3. Nitti VW, Dmochowski R, Herschorn S, Sand P, Thompson C, Nardo C, et al. OnabotulinumtoxinA for the treatment of patients with overactive bladder and urinary incontinence: results of a phase 3, randomized, placebo controlled trial. J Urol. 2013; 189:2186–2193. PMID: 23246476.
Article4. Abdel-Meguid TA. Botulinum toxin-A injections into neurogenic overactive bladder--to include or exclude the trigone? A prospective, randomized, controlled trial. J Urol. 2010; 184:2423–2428. PMID: 20952003.
Article5. Kuo HC. Bladder base/trigone injection is safe and as effective as bladder body injection of onabotulinumtoxinA for idiopathic detrusor overactivity refractory to antimuscarinics. Neurourol Urodyn. 2011; 30:1242–1248. PMID: 21560152.
Article6. Lucioni A, Rapp DE, Gong EM, Fedunok P, Bales GT. Intravesical botulinum type A toxin injection in patients with overactive bladder: trigone versus trigone-sparing injection. Can J Urol. 2006; 13:3291–3295. PMID: 17076955.7. Manecksha RP, Cullen IM, Ahmad S, McNeill G, Flynn R, McDermott TE, et al. Prospective randomised controlled trial comparing trigone-sparing versus trigone-including intradetrusor injection of abobotulinumtoxinA for refractory idiopathic detrusor overactivity. Eur Urol. 2012; 61:928–935. PMID: 22078337.
Article8. Dobberfuhl AD, Chen B, Han X, Diaz E, Comiter CV. Ambulatory and cystometric response following single versus multiple onabotulinumtoxina detrusor injections in a rat model of overactive bladder induced by intravesical acetic acid [abstract]. Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction 2017 winter meeting program book. 2017. p. 147.9. Dobberfuhl AD, Chen B, Han X, Diaz EC, Comiter C. No Adverse change in ambulatory voiding function after trigone onabotulinumtoxinA detrusor injection in the rat [abstract]. In : International Continence Society 2017 scientific programme; 2017. Abstract No. 775.10. Pinto R, Costa D, Morgado A, Pereira P, Silva J, Cruz F. Results from a randomized, double blind, placebo-controlled trial to evaluate efficacy and safety of intra-trigonal injection of onabotulinum toxin A in patients with bladder pain syndrome/interstitial cystitis [abstract]. J Urol. 2017; 197(Suppl 4):e46. Abstract No. PD01-01.
Article11. Stav K, Leibovici D, Goren E, Livshitz A, Siegel YI, Lindner A, et al. Adverse effects of cystoscopy and its impact on patients’ quality of life and sexual performance. Isr Med Assoc J. 2004; 6:474–478. PMID: 15326827.12. Rahnama'i MS, Marcelissen TAT, Brierley B, Schurch B, de Vries P. Long-term compliance and results of intravesical botulinum toxin A injections in male patients. Neurourol Urodyn. 2017; 36:1855–1859. PMID: 28084637.13. Bartley J, Han E, Gupta P, Gaines N, Killinger KA, Boura JA, et al. Transvaginal trigger point injections improve pain scores in women with pelvic floor hypertonicity and pelvic pain conditions. Female Pelvic Med Reconstr Surg. 2018; 4. 04. [Epub]. DOI: 10.1097/SPV.0000000000000581.
Article14. Spradling K, Khoyilar C, Abedi G, Okhunov Z, Wikenheiser J, Yoon R, et al. Redefining the autonomic nerve distribution of the bladder using 3-dimensional image reconstruction. J Urol. 2015; 194:1661–1667. PMID: 26003207.
Article15. Yang JM, Huang WC. Bladder wall thickness on ultrasonographic cystourethrography: affecting factors and their implications. J Ultrasound Med. 2003; 22:777–782. PMID: 12901404.16. Kuhn A, Bank S, Robinson D, Klimek M, Kuhn P, Raio L. How should bladder wall thickness be measured? A comparison of vaginal, perineal and abdominal ultrasound. Neurourol Urodyn. 2010; 29:1393–1396. PMID: 20976813.
Article17. Blatt AH, Titus J, Chan L. Ultrasound measurement of bladder wall thickness in the assessment of voiding dysfunction. J Urol. 2008; 179:2275–2278. discussion 2278-9. PMID: 18423703.
Article18. Oelke M, Höfner K, Jonas U, Ubbink D, de la Rosette J, Wijkstra H. Ultrasound measurement of detrusor wall thickness in healthy adults. Neurourol Urodyn. 2006; 25:308–317. discussion 318. PMID: 16652381.
Article19. Khullar V, Salvatore S, Cardozo L, Bourne TH, Abbott D, Kelleher C. A novel technique for measuring bladder wall thickness in women using transvaginal ultrasound. Ultrasound Obstet Gynecol. 1994; 4:220–223. PMID: 12797185.
Article20. Kuo HC. Measurement of detrusor wall thickness in women with overactive bladder by transvaginal and transabdominal sonography. Int Urogynecol J Pelvic Floor Dysfunct. 2009; 20:1293–1299. PMID: 19557300.
Article21. Alsinnawi M, Torreggiani W, Sheikh M, Thomas A, Donnellan J, Flynn R, et al. Delayed contrast-enhanced MRI to localize Botox after cystoscopic intravesical injection. Int Urol Nephrol. 2015; 47:893–898. PMID: 25894961.
Article22. Mehnert U, Boy S, Schmid M, Reitz A, von Hessling A, Hodler J, et al. A morphological evaluation of botulinum neurotoxin A injections into the detrusor muscle using magnetic resonance imaging. World J Urol. 2009; 27:397–403. PMID: 19145439.
Article23. Sermeus LA, Sala-Blanch X, McDonnell G, Lobo CA, Nicholls BJ, van Geffen GJ, et al. Ultrasound-guided approach to nerves (direct vs. tangential) and the incidence of intraneural injection: a cadaveric study. Anaesthesia. 2017; 72:461–469. PMID: 28185262.
Article24. Choquet O, Morau D, Biboulet P, Capdevila X. Where should the tip of the needle be located in ultrasound-guided peripheral nerve blocks? Curr Opin Anaesthesiol. 2012; 25:596–602. PMID: 22821146.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of transvaginal ultrasound-guided aspiration in benign pelvic cyst
- Feasibility of Ultrasound Guided Atlanto-occipital Joint Injection
- Feasibility of Ultrasound-Guided Intraarticular Contrast Injection for MR Arthrography
- Accuracy of Ultrasound-Guided and Non-guided Botulinum Toxin Injection Into Neck Muscles Involved in Cervical Dystonia: A Cadaveric Study
- Usefulness of Ultrasound for Carpal Tunnel Syndrome Proven in Meta-Analysis Studies