J Korean Neurosurg Soc.
2019 Jan;62(1):46-52. 10.3340/jkns.2017.0304.
A Nationwide Study of Surgery in a Newly Diagnosed Spine Metastasis Population
- Affiliations
-
- 1Department of Neurosurgery, CHA Bundang Medical Center, CHA University College of Medicine, Seongnam, Korea.
- 2Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea. chungc@snu.ac.kr
- 3Neuroscience Research Institute, Seoul National University Medical Research Center, Seoul, Korea.
- 4Clinical Research Institute, Seoul National University Hospital, Seoul, Korea.
- 5Department of Brain and Cognitive Sciences, Seoul National University College of Natural Sciences, Seoul, Korea.
- 6Department of Biostatistics, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 7Department of Nursing, Chosun University College of Medicine, Gwangju, Korea.
- 8Department of Neurosurgery, Korea Cancer Center Hospital, Korea Institute of Radiological and Medical Science, Seoul, Korea.
- 9Department of Neurosurgery, Neuroscience & Radiosurgery Hybrid Research Center, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Ilsan, Korea.
- 10Department of Radiation Oncology, St. Vincent’s Hospital, The Catholic University of Korea School of Medicine, Seoul, Korea.
- KMID: 2434345
- DOI: http://doi.org/10.3340/jkns.2017.0304
Abstract
OBJECTIVE
The aim of this nationwide study was to analyze the current state of patients with newly diagnosed metastatic spine tumors according to surgical methods.
METHODS
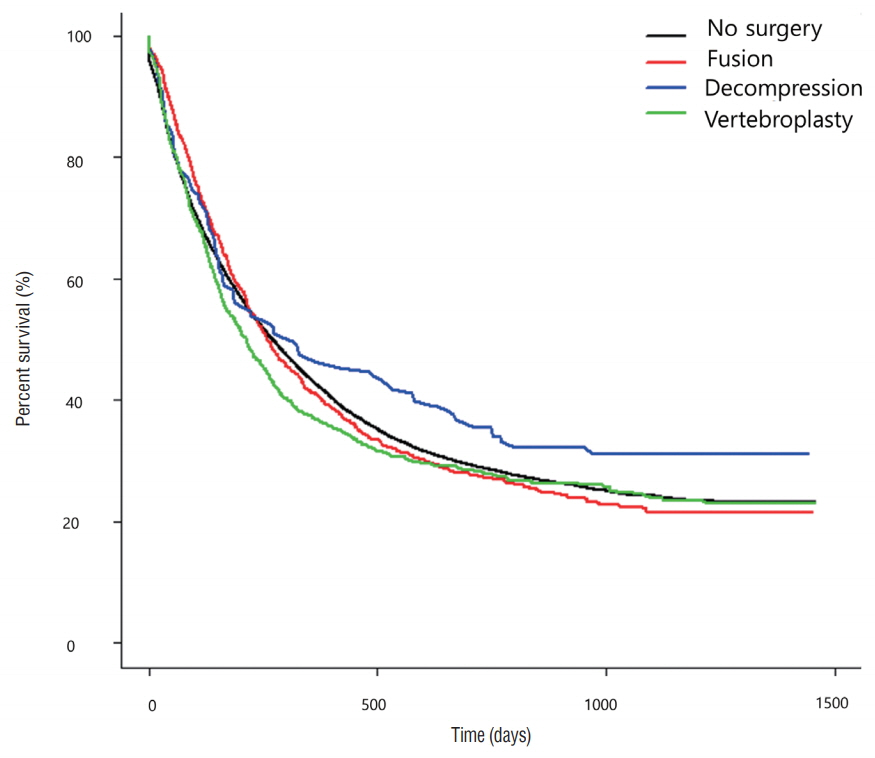
Data was extracted from the Korean Health Insurance Review and Assessment Service database. Surgery was categorized into three methods : fusion, decompression, and vertebroplasty. Data included patient age, sex, health insurance type, and co-morbidities. Survival rates of metastatic spine tumor patients according to each surgical method were evaluated.
RESULTS
Among 1677 patients who had an operation, 823 patients were treated by fusion, 141 patients underwent decompression, and 713 patients were treated by vertebroplasty. The three most prevalent primary tumor sites were the lung, breast, and liver & biliary. On the other hand, the three most prevalent primary tumor sites of patients who underwent surgery were the lung, liver & biliary, and the prostate. The median survival periods for each surgical method in the metastatic spine tumor patients were 228 days for those who underwent surgery, 249 days for decompression, and 154 days for vertebroplasty. Age, sex, and comorbidities significantly affected survival rate.
CONCLUSION
For every primary tumor site, decompression was the least common surgical method during the study period. Although the three surgical methods did not significantly affect the survival period, patients with a poor prognosis tended to undergo vertebroplasty.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Change of Pyogenic and Tuberculous Spondylitis between 2007 and 2016 Year : A Nationwide Study
Yeon Jee Kim, Je Beom Hong, Yeo Song Kim, Jeeeun Yi, Jung Min Choi, Seil Sohn
J Korean Neurosurg Soc. 2020;63(6):784-793. doi: 10.3340/jkns.2020.0013.
Reference
-
References
1. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 40:373–383. 1987.
Article2. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 36:8–27. 1998.
Article3. Kim CH, Chung CK, Park CS, Choi B, Kim MJ, Park BJ. Reoperation rate after surgery for lumbar herniated intervertebral disc disease: nationwide cohort study. Spine (Phila Pa 1976). 38:581–590. 2013.
Article4. Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine (Phila Pa 1976). 32:382–387. 2007.
Article5. Sohn S, Kim J, Chung CK, Lee NR, Chang UK, Sohn MJ. A nationwide study of stereotactic radiosurgery in a newly diagnosed spine metastasis population. Stereotact Funct Neurosurg. 95:189–196. 2017.
Article6. Sohn S, Kim J, Chung CK, Lee NR, Park E, Chang UK, et al. A nationwide epidemiological study of newly diagnosed spine metastasis in the adult Korean population. Spine J. 16:937–945. 2016.
Article7. Sohn S, Kim J, Chung CK, Lee NR, Sohn MJ, Kim SH. A nation-wide epidemiological study of newly diagnosed primary spine tumor in the adult Korean population, 2009-2011. J Korean Neurosurg Soc. 60:195–204. 2017.
Article8. Sohn S, Kim JH, Chung CK, Lee NR, Park EJ, Chang UK, et al. Nationwide epidemiology and healthcare utilization of spine tumor patients in the adult Korean population, 2009-2012. Neuro-Oncology Practice. 2:93–100. 2015.
Article9. Yoon SJ, Bae SC, Lee SI, Chang H, Jo HS, Sung JH, et al. Measuring the burden of disease in Korea. J Korean Med Sci. 22:518–523. 2007.
Article10. Zaikova O, Giercksky KE, Fosså SD, Kvaløy S, Johannesen TB, Skjelda S. A population-based study of spinal metastatic disease in South-East Norway. Clin Oncol (R Coll Radiol). 21:753–759. 2009.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Utility of the National Lung Screening Trial Criteria for Estimation of Lung Cancer in the Korean Population
- Outcomes after Surgery for Spinal Metastasis of Colorectal Origin: Case Series
- Incidence and Treatment Pattern of Extremity Soft Tissue Sarcoma in Korea, 2009-2011: A Nationwide Study Based on the Health Insurance Review and Assessment Service Database
- Intramedullary Spinal Cord Metastasis: Case Report
- Drop Metastasis of Adrenocorticotropic Hormone-Producing Pituitary Carcinoma to the Cauda Equina