Anesth Pain Med.
2019 Jan;14(1):63-66. 10.17085/apm.2019.14.1.63.
Sustained erroneous near-infrared cerebral oxygen saturation in alert icteric patient with vanishing bile duct syndrome during and after liver transplantation: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea. skim@schmc.ac.kr
- KMID: 2434201
- DOI: http://doi.org/10.17085/apm.2019.14.1.63
Abstract
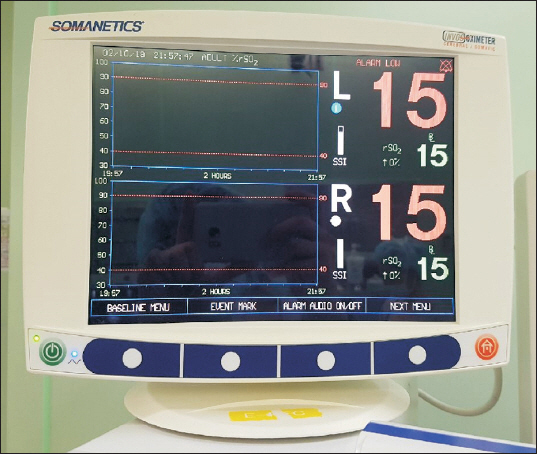
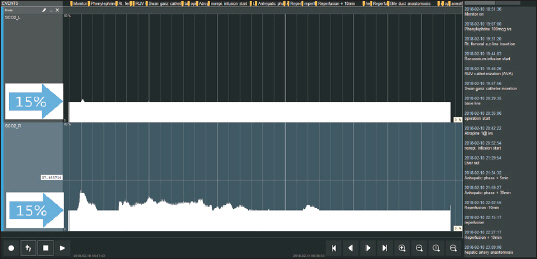
- Monitoring cerebral oxygenation using a near infrared spectroscopy (NIRS) device is useful for estimating cerebral hypoperfusion and is available during liver transplantation (LT). However, high serum bilirubin concentration can interfere with NIRS because bilirubin absorbs near infrared light. We report a patient who underwent LT with a diagnosis of vanishing bile duct syndrome, whose regional cerebral oxygen saturation (rSOâ‚‚) remained below 15% even with alert mental status and SpO2â‚‚ value of 99%. The rSOâ‚‚ values were almost fixed at the lowest measurable level throughout the intra- and postoperative period. We report a case of erroneously low rSOâ‚‚ values during the perioperative period in a liver transplant recipient which might be attributable to skin pigmentation rather than higher serum bilirubin concentration.
Keyword
MeSH Terms
Figure
Reference
-
1. Pere P, Höckerstedt K, Isoniemi H, Lindgren L. Cerebral blood flow and oxygenation in liver transplantation for acute or chronic hepatic disease without venovenous bypass. Liver Transpl. 2000; 6:471–9. DOI: 10.1053/jlts.2000.8186. PMID: 10915171.2. Song JG, Jeong SM, Shin WJ, Jun IG, Shin K, Huh IY, et al. Laboratory variables associated with low near-infrared cerebral oxygen saturation in icteric patients before liver transplantation surgery. Anesth Analg. 2011; 112:1347–52. DOI: 10.1213/ANE.0b013e318214b2b0. PMID: 21543778.3. Blei AT, Olafsson S, Webster S, Levy R. Complications of intracranial pressure monitoring in fulminant hepatic failure. Lancet. 1993; 341:157–8. DOI: 10.1016/0140-6736(93)90016-A.4. Casati A, Spreafico E, Putzu M, Fanelli G. [New technology for noninvasive brain monitoring: continuous cerebral oximetry]. Minerva Anestesiol. 2006; 72:605–25. Italian. PMID: 16865080.5. Plachky J, Hofer S, Volkmann M, Martin E, Bardenheuer HJ, Weigand MA. Regional cerebral oxygen saturation is a sensitive marker of cerebral hypoperfusion during orthotopic liver transplantation. Anesth Analg. 2004; 99:344–9. DOI: 10.1213/01.ANE.0000124032.31843.61. PMID: 15271702.6. Madsen PL, Skak C, Rasmussen A, Secher NH. Interference of cerebral near-infrared oximetry in patients with icterus. Anesth Analg. 2000; 90:489–93. DOI: 10.1213/00000539-200002000-00046. PMID: 10648345.7. Lee HC, Jung CW. Vital Recorder-a free research tool for automatic recording of high-resolution time-synchronised physiological data from multiple anaesthesia devices. Sci Rep. 2018; 8:1527. DOI: 10.1038/s41598-018-20062-4. PMID: 29367620. PMCID: PMC5784161.8. Reau NS, Jensen DM. Vanishing bile duct syndrome. Clin Liver Dis. 2008; 12:203–17. DOI: 10.1016/j.cld.2007.11.007. PMID: 18242505.9. Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth. 2009; 103(Suppl 1):i3–13. DOI: 10.1093/bja/aep299. PMID: 20007987.10. Jun IG, Shin WJ, Park YS, Song JG, Kim YK, Hwang GS. Factors affecting intraoperative changes in regional cerebral oxygen saturation in patients undergoing liver transplantation. Transplant Proc. 2013; 45:245–50. DOI: 10.1016/j.transproceed.2012.10.025. PMID: 23375309.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Vanishing Bile Duct Syndrome Associated with Ibuprofen Overuse
- A Case of Vanishing Bile Duct Syndrome after Drug-Induced Liver Injury Caused by Pelubiprofen
- A Case of Stevens-Johnson Syndrome Plus Vanishing Bile Duct Syndrome Associated with Ibuprofen Use
- A Case of Vanishing Bile Duct Syndrome Associated with Hypersensitivity to Allopurinol
- Cerebral Oxygen Saturation Monitoring during Carotid Endarterectomy: A case report