Intest Res.
2018 Oct;16(4):571-578. 10.5217/ir.2018.00033.
Medication non-adherence in inflammatory bowel diseases is associated with disability
- Affiliations
-
- 1Sydney Medical School, University of Sydney, Sydney, Australia. rupertleong@outlook.com
- 2Faculty of Medicine, University of New South Wales, Sydney, Australia.
- 3Gastroenterology and Liver Services, Concord Hospital, Sydney, Australia.
- KMID: 2434159
- DOI: http://doi.org/10.5217/ir.2018.00033
Abstract
- BACKGROUND/AIMS
Medication non-adherence is common in inflammatory bowel diseases (IBD). The short-term consequences of non-adherence include increased disease relapse but the long-term impact upon patients in terms of daily functional impairment are less well characterized. Identifying negative outcomes, such as disability, may encourage adherence.
METHODS
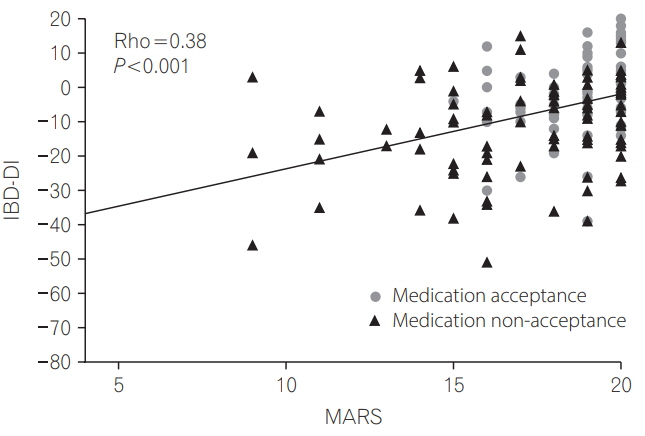
Consecutive ambulatory IBD subjects completed the Medication Adherence Rating Scale (MARS; non-adherence defined as ≤16), Inflammatory Bowel Diseases Disability Index (IBD-DI; disability: < 3.5) and Beliefs about Medicines Questionnaire (high necessity/concerns: ≥16). The primary outcome was the association between medication non-adherence and disability. Secondary outcomes were the predictors of these outcomes.
RESULTS
A total of 173 subjects on IBD maintenance medications were recruited (98 Crohn's disease, 75 ulcerative colitis: median IBD-DI, -5.0; interquartile range [IQR], -14.0 to 4.0 and median MARS, 19.0; IQR, 18 to 20) of whom 24% were non-adherent. Disability correlated significantly with medication non-adherence (r=0.38, P < 0.0001). Median IBD-DI for non-adherers was significantly lower than adherers (-16.0 vs. -2.0, P < 0.0001). Predictors of disability included female sex (P=0.002), previous hospitalization (P=0.023), management in a referral hospital clinic (P=0.008) and medication concerns (P < 0.0001). Non-adherence was independently associated with difficulty managing bowel movements (odds ratio [OR], 3.71; 95% confidence interval [CI], 1.50-9.16, P=0.005), rectal bleeding (OR, 2.69; 95% CI, 1.14-6.36; P=0.024) and arthralgia/arthritis (OR, 2.56; 95% CI, 1.11-5.92; P=0.028).
CONCLUSIONS
Medication non-adherence was associated with significantly increased disability in IBD. Female gender, higher disease severity and medication concerns were additional predictors of disability.
MeSH Terms
Figure
Reference
-
1. Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015; 12:205–217.
Article2. Ko Y, Butcher R, Leong RW. Epidemiological studies of migration and environmental risk factors in the inflammatory bowel diseases. World J Gastroenterol. 2014; 20:1238–1247.
Article3. Vatn MH. Natural history and complications of IBD. Curr Gastroenterol Rep. 2009; 11:481–487.
Article4. Ott C, Schölmerich J. Extraintestinal manifestations and complications in IBD. Nat Rev Gastroenterol Hepatol. 2013; 10:585–595.
Article5. Lix LM, Graff LA, Walker JR, et al. Longitudinal study of quality of life and psychological functioning for active, fluctuating, and inactive disease patterns in inflammatory bowel disease. Inflamm Bowel Dis. 2008; 14:1575–1584.
Article6. Peyrin-Biroulet L. What is the patient’s perspective: how important are patient-reported outcomes, quality of life and disability? Dig Dis. 2010; 28:463–471.
Article7. World Health Organization. Document A29/INFDOCI/1. Geneva: WHO;1976.8. Peyrin-Biroulet L, Cieza A, Sandborn WJ, et al. Development of the first disability index for inflammatory bowel disease based on the international classification of functioning, disability and health. Gut. 2012; 61:241–247.
Article9. Lo B, Prosberg MV, Gluud LL, et al. Systematic review and meta-analysis: assessment of factors affecting disability in inflammatory bowel disease and the reliability of the inflammatory bowel disease disability index. Aliment Pharmacol Ther. 2018; 47:6–15.
Article10. Leong RW, Huang T, Ko Y, et al. Prospective validation study of the International Classification of Functioning, Disability and Health score in Crohn’s disease and ulcerative colitis. J Crohns Colitis. 2014; 8:1237–1245.
Article11. Lee Y, McCombie A, Gearry R, et al. Disability in restorative proctocolectomy recipients measured using the Inflammatory Bowel Disease Disability Index. J Crohns Colitis. 2016; 10:1378–1384.
Article12. Selinger CP, Robinson A, Leong RW. Clinical impact and drivers of non-adherence to maintenance medication for inflammatory bowel disease. Expert Opin Drug Saf. 2011; 10:863–870.
Article13. Jackson CA, Clatworthy J, Robinson A, Horne R. Factors associated with non-adherence to oral medication for inflammatory bowel disease: a systematic review. Am J Gastroenterol. 2010; 105:525–539.
Article14. Ediger JP, Walker JR, Graff L, et al. Predictors of medication adherence in inflammatory bowel disease. Am J Gastroenterol. 2007; 102:1417–1426.
Article15. van der Have M, Oldenburg B, Kaptein AA, et al. Non-adherence to anti-TNF therapy is associated with illness perceptions and clinical outcomes in outpatients with inflammatory bowel disease: results from a prospective multicentre study. J Crohns Colitis. 2016; 10:549–555.
Article16. Trindade AJ, Ehrlich A, Kornbluth A, Ullman TA. Are your patients taking their medicine? Validation of a new adherence scale in patients with inflammatory bowel disease and comparison with physician perception of adherence. Inflamm Bowel Dis. 2011; 17:599–604.
Article17. Higgins PD, Rubin DT, Kaulback K, Schoenfield PS, Kane SV. Systematic review: impact of non-adherence to 5-aminosalicylic acid products on the frequency and cost of ulcerative colitis flares. Aliment Pharmacol Ther. 2009; 29:247–257.
Article18. Chan W, Chen A, Tiao D, Selinger C, Leong R. Medication adherence in inflammatory bowel disease. Intest Res. 2017; 15:434–445.
Article19. Selinger CP, Andrews JM, Titman A, et al. Long-term follow-up reveals low incidence of colorectal cancer, but frequent need for resection, among Australian patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2014; 12:644–650.
Article20. Horne R, Parham R, Driscoll R, Robinson A. Patients’ attitudes to medicines and adherence to maintenance treatment in inflammatory bowel disease. Inflamm Bowel Dis. 2009; 15:837–844.
Article21. Selinger CP, Eaden J, Jones DB, et al. Modifiable factors associated with nonadherence to maintenance medication for inflammatory bowel disease. Inflamm Bowel Dis. 2013; 19:2199–2206.
Article22. Fialko L, Garety PA, Kuipers E, et al. A large-scale validation study of the Medication Adherence Rating Scale (MARS). Schizophr Res. 2008; 100:53–59.
Article23. Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psych Health. 1999; 14:1–24.
Article24. Kane S, Shaya F. Medication non-adherence is associated with increased medical health care costs. Dig Dis Sci. 2008; 53:1020–1024.
Article25. Sellin J. Disability in IBD: the devil is in the details. Inflamm Bowel Dis. 2010; 16:23–26.
Article26. Berry SK, Melmed GY. Quality indicators in inflammatory bowel disease. Intest Res. 2018; 16:43–47.
Article27. Brakenhoff LK, van der Heijde DM, Hommes DW. IBD and arthropathies: a practical approach to its diagnosis and management. Gut. 2011; 60:1426–1435.
Article28. Stange EF, Travis SP, Vermeire S, et al. European evidence-based consensus on the diagnosis and management of ulcerative colitis: definitions and diagnosis. J Crohns Colitis. 2008; 2:1–23.
Article29. Stange EF, Travis SP, Vermeire S, et al. European evidence based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. Gut. 2006; 55 Suppl 1:i1–i15.
Article30. Norton C, Dibley LB, Bassett P. Faecal incontinence in inflammatory bowel disease: associations and effect on quality of life. J Crohns Colitis. 2013; 7:e302–e311. doi: 10.1016/j.crohns.2012.11.004.
Article31. Gower-Rousseau C, Sarter H, Savoye G, et al. Validation of the Inflammatory Bowel Disease Disability Index in a population-based cohort. Gut. 2017; 66:588–596.
Article32. Chan W, Shim HH, Lim MS, et al. Symptoms of anxiety and depression are independently associated with inflammatory bowel disease-related disability. Dig Liver Dis. 2017; 49:1314–1319.
Article33. Tiao DK, Chan W, Jeganathan J, et al. Inflammatory bowel disease pharmacist adherence counseling improves medication adherence in Crohn’s disease and ulcerative colitis. Inflamm Bowel Dis. 2017; 23:1257–1261.
Article34. Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich). 2008; 10:348–354.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Medication adherence in inflammatory bowel disease
- Medication-Related Knowledge and Medication Adherence in Pediatric and Adolescent Patients with Inflammatory Bowel Disease
- Medication Adherence in Korean Patients with Inflammatory Bowel Disease and Its Associated Factors
- Evaluation and improvement of adherence to medication
- Antihypertensive Drug Medication Adherence of People with Disabilities and its Affecting Factors in Korea