Ann Rehabil Med.
2018 Apr;42(2):358-362. 10.5535/arm.2018.42.2.358.
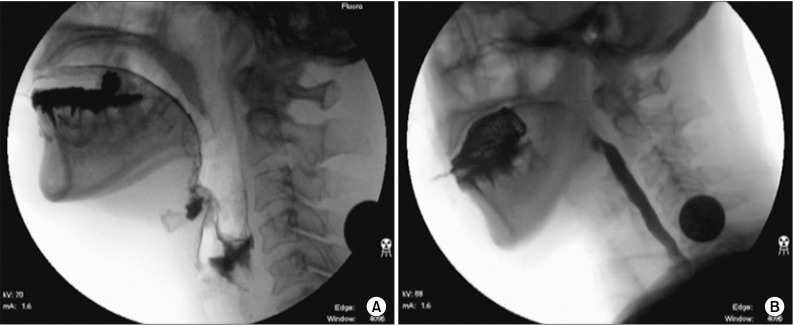
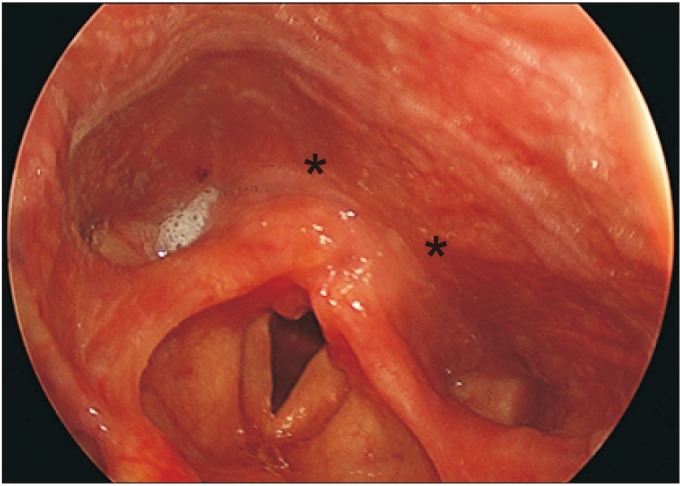
Botulinum Toxin Injection in the Treatment of Postextubation Dysphagia: A Case Report
- Affiliations
-
- 1Department of Rehabilitation Medicine, Dankook University College of Medicine, Cheonan, Korea. magnarbor@dankook.ac.kr
- 2Department of Nanobiomedical Science & WCU Research Center, Dankook University, Cheonan, Korea.
- 3Institute of Tissue Regeneration Engineering (ITREN), Dankook University, Cheonan, Korea.
- KMID: 2432208
- DOI: http://doi.org/10.5535/arm.2018.42.2.358
Abstract
- Prolonged intubation is known to bring on postextubation dysphagia (PED) in some patients. We have noted that there were some studies to investigate specific type and pattern of PED, which showed large variety of different swallowing abnormalities as mechanisms of PED that are multifactorial. There are several options of treatment in accordance with the management of these abnormalities. A botulinum toxin (BoT) injection into the upper esophageal sphincter (UES) can improve swallowing functions for patients with this disorder, by working to help the muscle relax. In this case, the conventional treatment was not effective in patients with PED, whereas the BoT injection made a great improvement for these patients. This study suggests that the UES pathology could be the main cause of PED.
MeSH Terms
Figure
Reference
-
1. Rassameehiran S, Klomjit S, Mankongpaisarnrung C, Rakvit A. Postextubation dysphagia. Proc (Bayl Univ Med Cent). 2015; 28:18–20. PMID: 25552788.
Article2. Bishop MJ, Weymuller EA, Fink BR. Laryngeal effects of prolonged intubation. Anesth Analg. 1984; 63:335–342. PMID: 6367543.
Article3. Barker J, Martino R, Reichardt B, Hickey EJ, Ralph-Edwards A. Incidence and impact of dysphagia in patients receiving prolonged endotracheal intubation after cardiac surgery. Can J Surg. 2009; 52:119–124. PMID: 19399206.4. Partik B, Pokieser P, Schima W, Schober E, Stadler A, Eisenhuber E, et al. Videofluoroscopy of swallowing in symptomatic patients who have undergone long-term intubation. AJR Am J Roentgenol. 2000; 174:1409–1412. PMID: 10789804.
Article5. Alfonsi E, Merlo IM, Ponzio M, Montomoli C, Tassorelli C, Biancardi C, et al. An electrophysiological approach to the diagnosis of neurogenic dysphagia: implications for botulinum toxin treatment. J Neurol Neurosurg Psychiatry. 2010; 81:54–60. PMID: 19762326.
Article6. Woisard-Bassols V, Alshehri S, Simonetta-Moreau M. The effects of botulinum toxin injections into the cricopharyngeus muscle of patients with cricopharyngeus dysfunction associated with pharyngo-laryngeal weakness. Eur Arch Otorhinolaryngol. 2013; 270:805–815. PMID: 22865104.
Article7. Goldsmith T. Evaluation and treatment of swallowing disorders following endotracheal intubation and tracheostomy. Int Anesthesiol Clin. 2000; 38:219–242. PMID: 10984854.
Article8. O'Leary MA, Grillone GA. Injection laryngoplasty. Otolaryngol Clin North Am. 2006; 39:43–54. PMID: 16469654.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Botulinum Toxin Injection for the Treatment of Dysphagia Caused by Cricopharyngeal Hypertonicity : A case report
- Endoscopic botulinum toxin injection in cricopharyngeal dysphagia
- Botulinum Toxin Injection Therapy for Lingual Dystonia: A Case Report
- Botulinum Toxin for Upper Esophageal Sphincter and Larynx
- Improvement of Lingual Dystonia Following Cerebellar Infarction through Botulinum Toxin Injection: a Case Report