Ann Rehabil Med.
2018 Apr;42(2):229-238. 10.5535/arm.2018.42.2.229.
Effects of Repetitive Peripheral Magnetic Stimulation on Patients With Acute Low Back Pain: A Pilot Study
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
- 2Department of Rehabilitation Medicine, Hallym University Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea. pmnrh@naver.com
- 3Department of Physical Medicine and Rehabilitation, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- KMID: 2432193
- DOI: http://doi.org/10.5535/arm.2018.42.2.229
Abstract
OBJECTIVE
To investigate the effects of real repetitive peripheral magnetic stimulation (rPMS) treatment compared to sham rPMS treatment on pain reduction and functional recovery of patients with acute low back pain.
METHODS
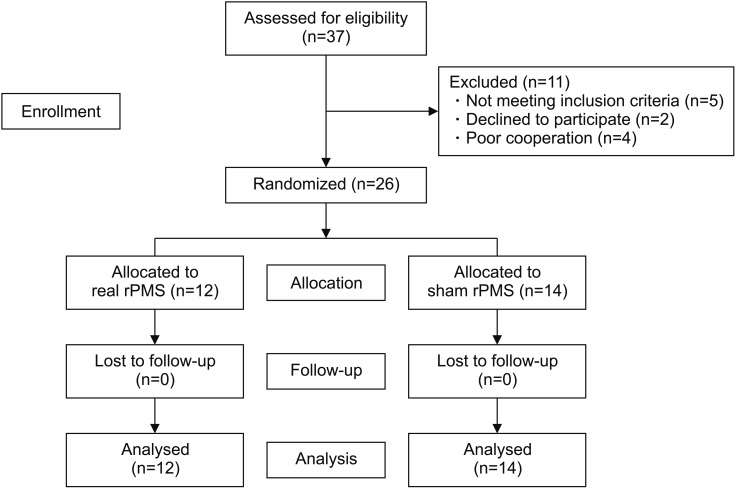
A total of 26 patients with acute low back pain were randomly allocated to the real rPMS group and the sham rPMS group. Subjects were then administered a total of 10 treatment sessions. Visual analogue scale (VAS) was assessed before and after each session. Oswestry Disability Index (ODI) and Roland-Morris Disability Questionnaire (RMDQ) were employed to assess functional recovery at baseline and after sessions 5 and 10.
RESULTS
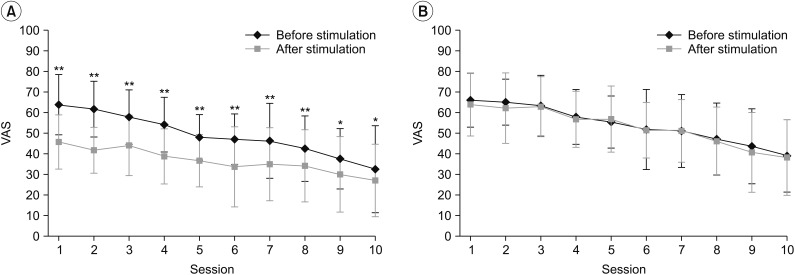
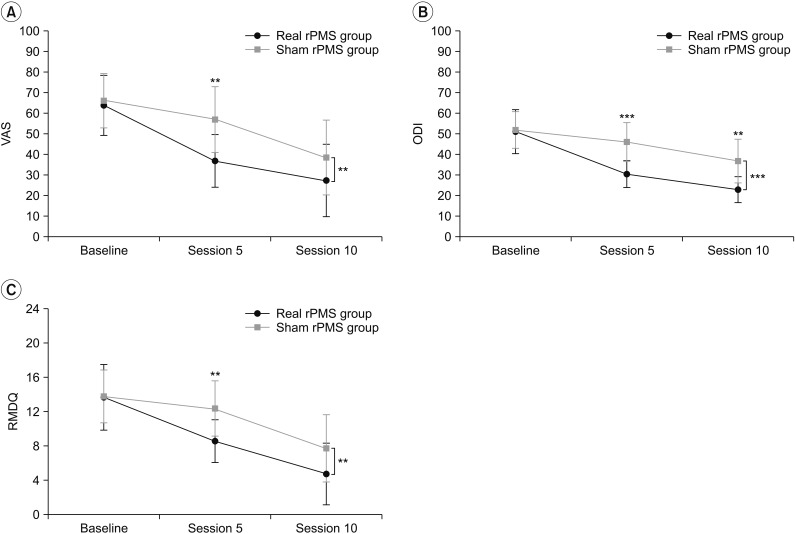
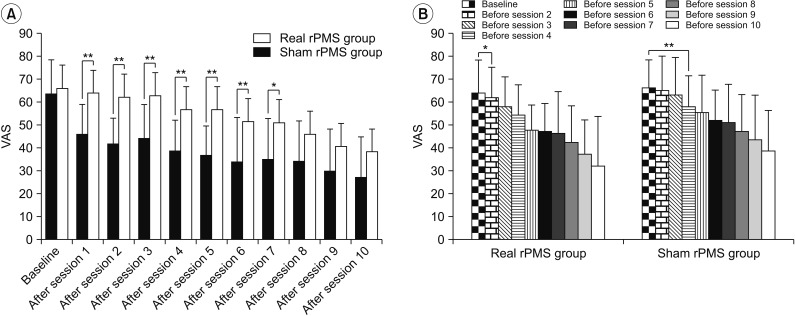
Real rPMS treatment showed significant pain reduction immediately after each session. Sustained and significant pain relief was observed after administering only one session in the real rPMS group. Significant functional improvement was observed in the real rPMS group compared to that in the sham rPMS group after sessions 5 and 10 based on ODI and after session 5 based on RMDQ.
CONCLUSION
Real rPMS treatment has immediate effect on pain reduction and sustained effect on pain relief for patients with acute low back pain compared to sham rPMS.
Keyword
MeSH Terms
Figure
Reference
-
1. Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380:2197–2223. PMID: 23245608.2. van Tulder M, Becker A, Bekkering T, Breen A, del Real MT, Hutchinson A, et al. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006; 15(Suppl 2):S169–S191. PMID: 16550447.
Article3. Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, et al. Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ. 2008; 337:a171. PMID: 18614473.
Article4. Downie AS, Hancock MJ, Rzewuska M, Williams CM, Lin CW, Maher CG. Trajectories of acute low back pain: a latent class growth analysis. Pain. 2016; 157:225–234. PMID: 26397929.5. Dahm KT, Brurberg KG, Jamtvedt G, Hagen KB. Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica. Cochrane Database Syst Rev. 2010; (6):CD007612. PMID: 20556780.
Article6. Saragiotto BT, Machado GC, Ferreira ML, Pinheiro MB, Abdel Shaheed C, Maher CG. Paracetamol for low back pain. Cochrane Database Syst Rev. 2016; (6):CD012230. PMID: 27271789.
Article7. Harirforoosh S, Asghar W, Jamali F. Adverse effects of nonsteroidal antiinflammatory drugs: an update of gastrointestinal, cardiovascular and renal complications. J Pharm Pharm Sci. 2013; 16:821–847. PMID: 24393558.
Article8. Kinkade S. Evaluation and treatment of acute low back pain. Am Fam Physician. 2007; 75:1181–1188. PMID: 17477101.9. Acute Low. Acute low back problems in adults: assessment and treatment. Am Fam Physician. 1995; 51:469–484. PMID: 7840043.10. Furlan AD, Giraldo M, Baskwill A, Irvin E, Imamura M. Massage for low-back pain. Cochrane Database Syst Rev. 2015; (9):CD001929. PMID: 26329399.
Article11. Beaulieu LD, Schneider C. Repetitive peripheral magnetic stimulation to reduce pain or improve sensorimotor impairments: a literature review on parameters of application and afferents recruitment. Neurophysiol Clin. 2015; 45:223–237. PMID: 26363684.
Article12. Kim J, Yoon SH, Rah UW, Cho KH, Hong JY. Effect of repetitive magnetic stimulation and transcutaneous electrical nerve stimulation in chronic low back pain: a pilot study. J Korean Acad Rehabil Med. 2010; 34:725–729.13. Lo YL, Fook-Chong S, Huerto AP, George JM. A randomized, placebo-controlled trial of repetitive spinal magnetic stimulation in lumbosacral spondylotic pain. Pain Med. 2011; 12:1041–1045. PMID: 21668750.
Article14. Masse-Alarie H, Flamand VH, Moffet H, Schneider C. Peripheral neurostimulation and specific motor training of deep abdominal muscles improve posturomotor control in chronic low back pain. Clin J Pain. 2013; 29:814–823. PMID: 23370067.15. Masse-Alarie H, Beaulieu LD, Preuss R, Schneider C. Repetitive peripheral magnetic neurostimulation of multifidus muscles combined with motor training influences spine motor control and chronic low back pain. Clin Neurophysiol. 2017; 128:442–453. PMID: 28160750.16. Maccabee PJ, Amassian VE, Cracco RQ, Cadwell JA. An analysis of peripheral motor nerve stimulation in humans using the magnetic coil. Electroencephalogr Clin Neurophysiol. 1988; 70:524–533. PMID: 2461286.
Article17. Smania N, Corato E, Fiaschi A, Pietropoli P, Aglioti SM, Tinazzi M. Therapeutic effects of peripheral repetitive magnetic stimulation on myofascial pain syndrome. Clin Neurophysiol. 2003; 114:350–358. PMID: 12559244.
Article18. Smania N, Corato E, Fiaschi A, Pietropoli P, Aglioti SM, Tinazzi M. Repetitive magnetic stimulation: a novel therapeutic approach for myofascial pain syndrome. J Neurol. 2005; 252:307–314. PMID: 15726272.
Article19. Saltychev M, Mattie R, McCormick Z, Barlund E, Laimi K. Psychometric properties of the Oswestry Disability Index. Int J Rehabil Res. 2017; 40:202–208. PMID: 28368870.
Article20. Stevens ML, Lin CC, Maher CG. The Roland Morris Disability Questionnaire. J Physiother. 2016; 62:116. PMID: 26687949.
Article21. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965; 150:971–979. PMID: 5320816.
Article22. Massion J. Movement, posture and equilibrium: interaction and coordination. Prog Neurobiol. 1992; 38:35–56. PMID: 1736324.
Article23. Tsao H, Danneels LA, Hodges PW. ISSLS prize winner: smudging the motor brain in young adults with recurrent low back pain. Spine (Phila Pa 1976). 2011; 36:1721–1727. PMID: 21508892.24. Tsao H, Danneels L, Hodges PW. Individual fascicles of the paraspinal muscles are activated by discrete cortical networks in humans. Clin Neurophysiol. 2011; 122:1580–1587. PMID: 21377923.
Article25. Masse-Alarie H, Schneider C. Revisiting the corticomotor plasticity in low back pain: challenges and perspectives. Healthcare (Basel). 2016; 4:67.26. Masse-Alarie H, Beaulieu LD, Preuss R, Schneider C. The side of chronic low back pain matters: evidence from the primary motor cortex excitability and the postural adjustments of multifidi muscles. Exp Brain Res. 2017; 235:647–659. PMID: 27847987.
Article27. Strutton PH, Theodorou S, Catley M, McGregor AH, Davey NJ. Corticospinal excitability in patients with chronic low back pain. J Spinal Disord Tech. 2005; 18:420–424. PMID: 16189454.
Article28. Flor H, Braun C, Elbert T, Birbaumer N. Extensive reorganization of primary somatosensory cortex in chronic back pain patients. Neurosci Lett. 1997; 224:5–8. PMID: 9132689.
Article29. Struppler A, Angerer B, Gundisch C, Havel P. Modulatory effect of repetitive peripheral magnetic stimulation on skeletal muscle tone in healthy subjects: stabilization of the elbow joint. Exp Brain Res. 2004; 157:59–66. PMID: 15309359.
Article30. Struppler A, Binkofski F, Angerer B, Bernhardt M, Spiegel S, Drzezga A, et al. a fronto-parietal network is mediating improvement of motor function related to repetitive peripheral magnetic stimulation: a PET-H2O15 study. Neuroimage. 2007; 36(Suppl 2):T174–T186. PMID: 17499165.
Article31. Gallasch E, Christova M, Kunz A, Rafolt D, Golaszewski S. Modulation of sensorimotor cortex by repetitive peripheral magnetic stimulation. Front Hum Neurosci. 2015; 9:407. PMID: 26236220.
Article32. Krause P, Straube A. Peripheral repetitive magnetic stimulation induces intracortical inhibition in healthy subjects. Neurol Res. 2008; 30:690–694. PMID: 18498680.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Repetitive Magnetic Stimulation and Transcutaneous Electrical Nerve Stimulation in Chronic Low Back Pain: A Pilot Study
- Short-Term Pain Relief by Repetitive Peripheral Magnetic Stimulation in Patients with Musculoskeletal Pain: A Pilot Study
- Repetitive Transcranial Magnetic Stimulation to Treat Depression and Insomnia with Chronic Low Back Pain
- Repetitive transcranial magnetic stimulation: a potential therapeutic modality for chronic low back pain
- Comparison between the Electric and Magnetic Stimulations for a Repetitive Nerve Stimulation Test