Korean J Pain.
2019 Jan;32(1):39-46. 10.3344/kjp.2019.32.1.39.
Effect of needle type on intravascular injection in transforaminal epidural injection: a meta-analysis
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konkuk University School of Medicine, Seoul, Korea. painfree@kuh.ac.kr
- 2Department of Obstetrics and Gynecology, Konkuk University School of Medicine, Seoul, Korea.
- KMID: 2430762
- DOI: http://doi.org/10.3344/kjp.2019.32.1.39
Abstract
- BACKGROUND
Lumbosacral transforaminal epidural injection (TFEI) is an effective treatment for spinal disease. However, TFEI may have several types of complications, some of which can be attributed to intravascular injection. We reviewed studies to compare the intravascular injection rate among different needle types.
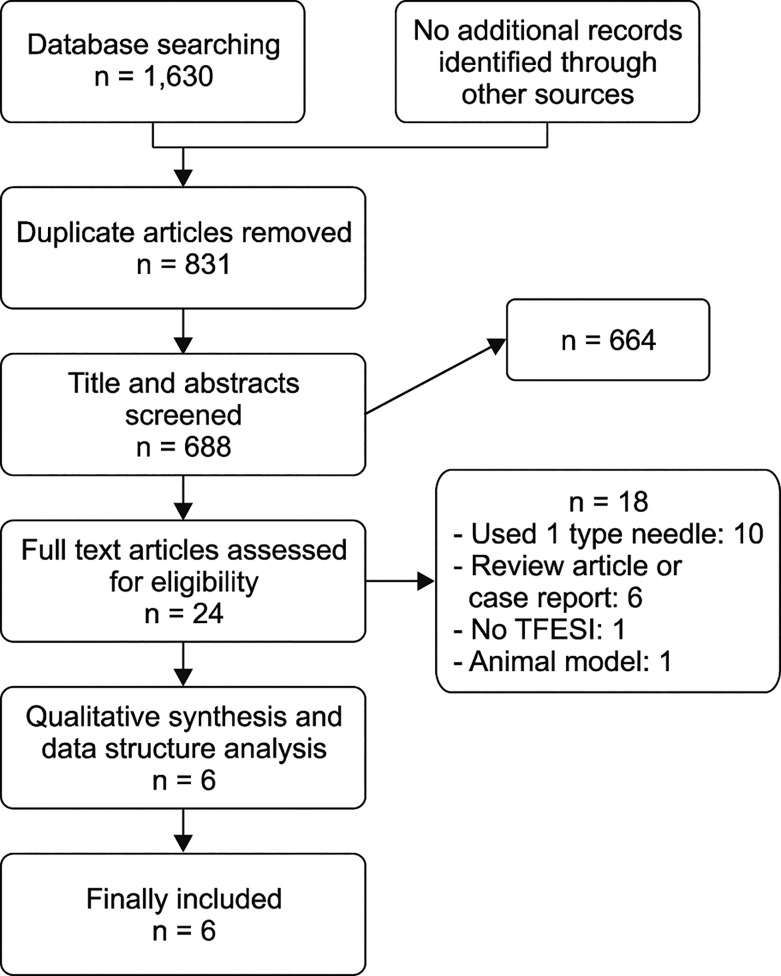
METHODS
We searched the literature for articles on the intravascular injection rate among different needle types used in TFEI. The search was performed using PubMed, MEDLINE, the Cochrane Library, EMBASE, and Web of Science.
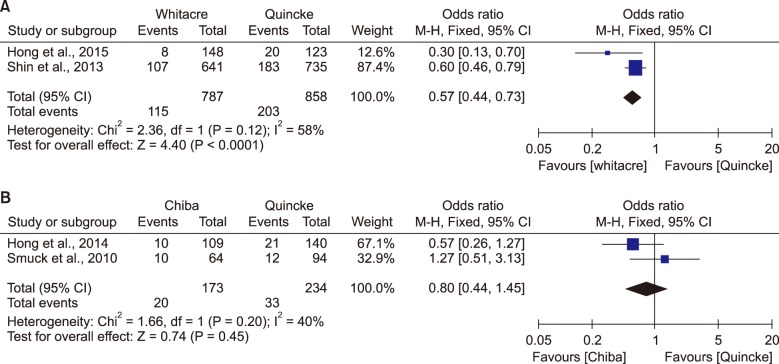
RESULTS
A total of six studies comprising 2359 patients were identified. Compared with the Quincke needle, the Whitacre needle reduced the intravascular injection rate (OR = 0.57, 95% CI = [0.44-0.73], P < 0.001). However, compared with the Quincke needle, the Chiba needle did not reduce the intravascular injection rate (OR = 0.80, 95% CI = [0.44-1.45], P = 0.46). In one study, the intravascular injection rate using a blunt-tip needle was lower than that using a sharp needle. In another study, the Whitacre and the blunt-tip needle have similar intravascular injection rates, while, the catheter-extension needle showed a reduced intravascular injection rate.
CONCLUSIONS
This meta-analysis showed that the Whitacre needle reduced the intravascular injection rate as compared with the Quincke needle, but failed to establish that the Chiba needle can decrease the intravascular injection rate in TFEI. Moreover, the blunt-tip needle can reduce the intravascular injection rate compared with the Quincke needle, and the catheter-extension needle can reduce the intravascular injection rate compared with the Whitacre and the blunt-tip needle.
Keyword
Figure
Reference
-
1. Marshall LL, Trethewie ER, Curtain CC. Chemical radiculitis. A clinical, physiological and immunological study. Clin Orthop Relat Res. 1977; 61–67. PMID: 608297.2. Boswell MV, Trescot AM, Datta S, Schultz DM, Hansen HC, Abdi S, et al. Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007; 10:7–111. PMID: 17256025.3. Buenaventura RM, Datta S, Abdi S, Smith HS. Systematic review of therapeutic lumbar transforaminal epidural steroid injections. Pain Physician. 2009; 12:233–251. PMID: 19165306.4. Davis N, Hourigan P, Clarke A. Transforaminal epidural steroid injection in lumbar spinal stenosis: an observational study with two-year follow-up. Br J Neurosurg. 2017; 31:205–208. PMID: 27548310.
Article5. Hong JH, Park EK, Park KB, Park JH, Jung SW. Comparison of clinical efficacy in epidural steroid injections through transforaminal or parasagittal approaches. Korean J Pain. 2017; 30:220–228. PMID: 28757923.
Article6. Manchikanti L, Singh V, Pampati V, Falco FJ, Hirsch JA. Comparison of the efficacy of caudal, interlaminar, and transforaminal epidural injections in managing lumbar disc herniation: is one method superior to the other? Korean J Pain. 2015; 28:11–21. PMID: 25589942.
Article7. Gupta R, Singh S, Kaur S, Singh K, Aujla K. Correlation between epidurographic contrast flow patterns and clinical effectiveness in chronic lumbar discogenic radicular pain treated with epidural steroid injections via different approaches. Korean J Pain. 2014; 27:353–359. PMID: 25317285.
Article8. Eckel TS, Bartynski WS. Epidural steroid injections and selective nerve root blocks. Tech Vasc Interv Radiol. 2009; 12:11–21. PMID: 19769903.
Article9. Cohen SP, Bicket MC, Jamison D, Wilkinson I, Rathmell JP. Epidural steroids: a comprehensive, evidence-based review. Reg Anesth Pain Med. 2013; 38:175–200. PMID: 23598728.10. Quraishi NA. Transforaminal injection of corticosteroids for lumbar radiculopathy: systematic review and meta-analysis. Eur Spine J. 2012; 21:214–219. PMID: 21892774.
Article11. Lee JH, Shin KH, Park SJ, Lee GJ, Lee CH, Kim DH, et al. Comparison of clinical efficacy between transforaminal and interlaminar epidural injections in lumbosacral disc herniation: a systematic review and meta-analysis. Pain Physician. 2018; 21:433–448. PMID: 30282389.12. Alleyne CH Jr, Cawley CM, Shengelaia GG, Barrow DL. Microsurgical anatomy of the artery of Adamkiewicz and its segmental artery. J Neurosurg. 1998; 89:791–795. PMID: 9817417.
Article13. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Freeman TL, Slaten WK. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil. 2000; 81:1045–1050. PMID: 10943753.
Article14. Kennedy DJ, Dreyfuss P, Aprill CN, Bogduk N. Paraplegia following image-guided transforaminal lumbar spine epidural steroid injection: two case reports. Pain Med. 2009; 10:1389–1394. PMID: 19863744.
Article15. Bogduk N, Dreyfuss P, Baker R, Yin W, Landers M, Hammer M, et al. Complications of spinal diagnostic and treatment procedures. Pain Med. 2008; 9:S11–S34.
Article16. McLain RF, Fry M, Hecht ST. Transient paralysis associated with epidural steroid injection. J Spinal Disord. 1997; 10:441–444. PMID: 9355063.
Article17. Reitman CA, Watters W 3rd. Subdural hematoma after cervical epidural steroid injection. Spine (Phila Pa 1976). 2002; 27:E174–E176. PMID: 11884923.
Article18. Scanlon GC, Moeller-Bertram T, Romanowsky SM, Wallace MS. Cervical transforaminal epidural steroid injections: more dangerous than we think? Spine (Phila Pa 1976). 2007; 32:1249–1256. PMID: 17495784.19. Murthy NS, Maus TP, Behrns CL. Intraforaminal location of the great anterior radiculomedullary artery (artery of Adamkiewicz): a retrospective review. Pain Med. 2010; 11:1756–1764. PMID: 21134118.
Article20. Özcan U, Şahin Ş, Gurbet A, Türker G, Özgür M, Çelebi S. Comparison of blunt and sharp needles for transforaminal epidural steroid injections. Agri. 2012; 24:85–89. PMID: 22865493.
Article21. Hong JH, Lee YH. Comparison of incidence of intravascular injections during transforaminal epidural steroid injection using different needle types. Korean J Anesthesiol. 2014; 67:193–197. PMID: 25302096.
Article22. Shin J, Kim YC, Lee SC, Kim JH. A comparison of Quincke and Whitacre needles with respect to risk of intravascular uptake in S1 transforaminal epidural steroid injections: a randomized trial of 1376 cases. Anesth Analg. 2013; 117:1241–1247. PMID: 24047591.
Article23. Smuck M, Paulus S, Patel A, Demirjian R, Ith MA, Kennedy DJ. Differential rates of inadvertent intravascular injection during lumbar transforaminal epidural injections using blunt-tip, pencil-point, and catheter-extension needles. Pain Med. 2015; 16:2084–2089. PMID: 26442619.
Article24. Smuck M, Yu AJ, Tang CT, Zemper E. Influence of needle type on the incidence of intravascular injection during transforaminal epidural injections: a comparison of short-bevel and long-bevel needles. Spine J. 2010; 10:367–371. PMID: 20171936.
Article25. Hong J, Jung S, Chang H. Whitacre needle reduces the incidence of intravascular uptake in lumbar transforaminal epidural steroid injections. Pain Physician. 2015; 18:325–331. PMID: 26218935.26. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996; 17:1–12. PMID: 8721797.
Article27. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009; 151:W65–W94. PMID: 19622512.
Article28. Selander D, Dhunér KG, Lundborg G. Peripheral nerve injury due to injection needles used for regional anesthesia. An experimental study of the acute effects of needle point trauma. Acta Anaesthesiol Scand. 1977; 21:182–188. PMID: 878831.
Article29. Lavi R, Yarnitsky D, Rowe JM, Weissman A, Segal D, Avivi I. Standard vs atraumatic Whitacre needle for diagnostic lumbar puncture: a randomized trial. Neurology. 2006; 67:1492–1494. PMID: 17060584.
Article30. Peterman SB. Postmyelography headache rates with Whitacre versus Quincke 22-gauge spinal needles. Radiology. 1996; 200:771–778. PMID: 8756930.
Article31. Akins EW, Hawkins IF Jr, Mladinich C, Tupler R, Siragusa RJ, Pry R. The blunt needle: a new percutaneous access device. AJR Am J Roentgenol. 1989; 152:181–182. PMID: 2783274.
Article32. Heavner JE, Racz GB, Jenigiri B, Lehman T, Day MR. Sharp versus blunt needle: a comparative study of penetration of internal structures and bleeding in dogs. Pain Pract. 2003; 3:226–231. PMID: 17147672.
Article33. Kloth DS, Calodney AK, Derby R, Lagattuta FP, O'Neill C, Yurth E, et al. Improving the safety of transforaminal epidural steroid injections in the treatment of cervical radiculopathy. Pain Physician. 2011; 14:285–293. PMID: 21587332.34. Kim DW, Han KR, Kim C, Chae YJ. Intravascular flow patterns in transforaminal epidural injections: a comparative study of the cervical and lumbar vertebral segments. Anesth Analg. 2009; 109:233–239. PMID: 19535715.
Article35. Furman MB, O'Brien EM, Zgleszewski TM. Incidence of intravascular penetration in transforaminal lumbosacral epidural steroid injections. Spine (Phila Pa 1976). 2000; 25:2628–2632. PMID: 11034648.
Article36. Furman MB, Giovanniello MT, O'Brien EM. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine (Phila Pa 1976). 2003; 28:21–25. PMID: 12544950.
Article37. El Abd OH, Amadera JE, Pimentel DC, Pimentel TS. Intravascular flow detection during transforaminal epidural injections: a prospective assessment. Pain Physician. 2014; 17:21–27. PMID: 24452642.38. Wolter T, Knoeller S, Berlis A, Hader C. CT-guided cervical selective nerve root block with a dorsal approach. AJNR Am J Neuroradiol. 2010; 31:1831–1836. PMID: 20801765.
Article39. Desai MJ, Shah B, Sayal PK. Epidural contrast flow patterns of transforaminal epidural steroid injections stratified by commonly used final needle-tip position. Pain Med. 2011; 12:864–870. PMID: 21539705.
Article40. Lee MH, Yang KS, Kim YH, Jung HD, Lim SJ, Moon DE. Accuracy of live fluoroscopy to detect intravascular injection during lumbar transforaminal epidural injections. Korean J Pain. 2010; 23:18–23. PMID: 20552068.
Article41. Jeon YH, Kim SY. Detection rate of intravascular injections during cervical medial branch blocks: a comparison of digital subtraction angiography and static images from conventional fluoroscopy. Korean J Pain. 2015; 28:105–108. PMID: 25852831.
Article42. Visnjevac O, Kim P, Farid-Davari S, Johnson P, Nader ND. Digital subtraction angiography versus real-time fluoroscopy for detection of intravascular penetration prior to epidural steroid injections: meta-analysis of prospective studies. Pain Physician. 2015; 18:29–36. PMID: 25675057.43. Chang Chien GC, Candido KD, Knezevic NN. Digital subtraction angiography does not reliably prevent paraplegia associated with lumbar transforaminal epidural steroid injection. Pain Physician. 2012; 15:515–523. PMID: 23159970.
Article44. Jasper JF. Role of digital subtraction fluoroscopic imaging in detecting intravascular injections. Pain Physician. 2003; 6:369–372. PMID: 16880884.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of incidence of intravascular injections during transforaminal epidural steroid injection using different needle types
- Evaluation of Contrast Flow Patterns with Fluoroscopic Guided Lumbar Transforaminal Epidural Injections
- Incidence of Intravascular Penetration during Transforaminal Lumbosacral Epidural Steroid Injection
- Accuracy of Live Fluoroscopy to Detect Intravascular Injection During Lumbar Transforaminal Epidural Injections
- Comparison of Transforaminal Epidural Steroid Injection and Lumbar/Caudal Epidural Steroid Injection for the Treatment of Lumbosacral Radiculopathy