Kosin Med J.
2018 Dec;33(2):200-207. 10.7180/kmj.2018.33.2.200.
Pulmonary tuberculosis occurred in patient with Tracheobronchopathia Osteochondroplastica
- Affiliations
-
- 1Department of Internal Medicine, Gachon University Gil Medical Center, Incheon, Korea. sangminlee77@naver.com
- 2Departement of Radiology, Gachon University Gil Medical Center, Incheon, Korea.
- 3Departement of Pathology, Gachon University Gil Medical Center, Incheon, Korea.
- KMID: 2430735
- DOI: http://doi.org/10.7180/kmj.2018.33.2.200
Abstract
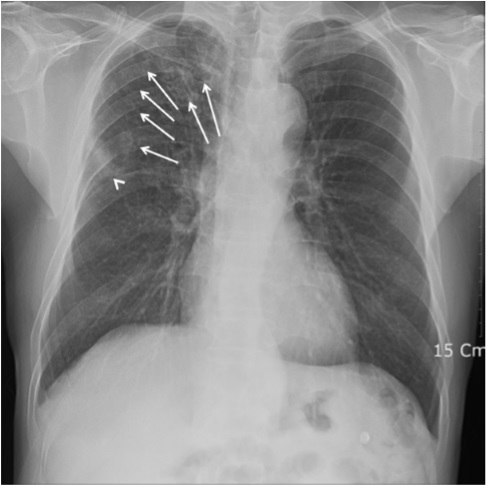
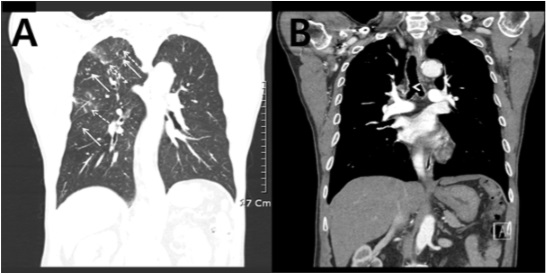
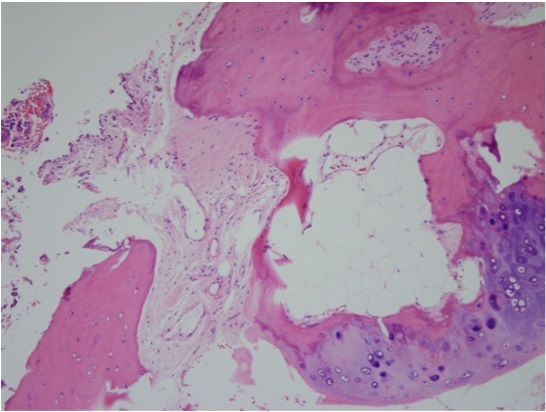
- Tracheobronchopathia osteoplastica (TO) is a rare benign disease in which the anterior inner wall of the tracheobronchus changes because of abnormal chondrogenesis or ossification, while the posterior wall of the trachea is spared. The etiology is not clearly understood, but may relate with chronic infection, inflammation, and trauma. In some case studies, it has also been reported to be accompanied by other chronic diseases such as atrophic rhinitis and amyloidosis. However, Coexistence of TO and tuberculosis has rarely been reported, and has never been reported in Korea. Here, we report a case of a 70-year-old male patient who complained of hemoptysis and whose case was diagnosed as TO and pulmonary tuberculosis through bronchoscopy with bronchial washing and biopsy.
MeSH Terms
Figure
Reference
-
1. Wilks S. Ossific deposits on larynx, trachea, and bronchi. Rans Pathol Soc London. 1857; 8:88.2. Zhu Y, Wu N, Huang HD, Dong YC, Sun QY, Zhang W, et al. A clinical study of tracheobronchopathia osteochondroplastica: findings from a large Chinese cohort. PLoS One. 2014; 9:e102068.
Article3. Hussain K, Gilbert S. Tracheopathia osteochondro plastica. Clin Med Res. 2003; 1:239–242.4. Prakash UB. Tracheobronchopathia osteochondro plastica. Semin Respir Crit Care Med. 2002; 23:167–175.5. Chroneou A, Zias N, Gonzalez AV, Beamis JF Jr. Tracheobronchopathia osteochondroplastica. An underrecognized entity? Monaldi Arch Chest Dis. 2008; 69:65–69.
Article6. Magro P, Garand G, Cattier B, Renjard L, Marquette CH, Diot P. Association of tracheobronchopathia osteochondroplastica and ozène. Rev Mal Respir. 2007; 24:883–887.7. Leske V, Lazor R, Coetmeur D, Crestani B, Chatté G, Cordier JF. Groupe d'Etudes et de Recherche sur les Maladies “Orphelines” Pulmonaires (GERM“O”P).Tracheobronchopathia osteochondroplastica: a study of 41 patients. Medicine (Baltimore). 2001; 80:378–390.8. Virchow R. Die krankhaften Geschwülste. 1st ed. Berlin Hirschwald 1863;442p.9. Aschoff-Freiburg L. Ueber Tracheopathia Osteoplastica. Verh Dtsch Gesch Pathol. 1910; 14:125–127.10. Clee MD, Anderson JM, Johnston RN. Clinical aspects of tracheobronchopathia osteochondroplastica. Br J Dis Chest. 1983; 77:308–314.
Article11. Nienhuis DM, Prakash UB, Edell ES. Tracheobronchopathia osteochondroplastica. Ann Otol Rhinol Laryngol. 1990; 99:689–694.
Article12. White BD, Kong A, Khoo E, Southcott AM. Computed tomography diagnosis of tracheobronchopathia osteochondroplastica. Australas Radiol. 2005; 49:319–321.
Article13. Manning JE, Goldin JG, Shpiner RB, Aberle DR. Case report: tracheobronchopathia osteochon droplastica. Clin Radiol. 1998; 53:302–309.14. Magnusson P, Rotemark G. Tracheobronchopathia osteochondroplastica. Three case reports. J Laryngol Otol. 1974; 88:159–164.15. Tukiainen H, Torkko M, Terho EO. Lung function in patients with tracheobronchopathia osteochondroplastica. Eur Respir J. 1988; 1:632–635.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tracheobronchopathia Osteochondroplastica detected during Difficult EndotrachealIntubation : A case report
- A Case of Tracheobronchopathia Osteochondroplastica with Upper Airway Obstruction
- A Case of Tracheobronchopathia Osteochondroplastica Associated with Atrophic Rhinitis
- Two Cases of Tracheobronchopathia Osteochondroplastica
- A Case of Tracheobronchopathia Osteochondroplastica Diagnosed by Endobronchial Ultrasonography