J Korean Orthop Assoc.
2018 Dec;53(6):513-521. 10.4055/jkoa.2018.53.6.513.
Ultrasound-Guided Axillary Brachial Plexus Block, Performed by Orthopedic Surgeons
- Affiliations
-
- 1Department of Orthopedic Surgery, Daejeon Sun Hospital, Daejeon, Korea. mediiron@naver.com
- KMID: 2430058
- DOI: http://doi.org/10.4055/jkoa.2018.53.6.513
Abstract
- PURPOSE
The purpose of this study was to assess the effectiveness and complications of an ultrasound-guided axillary brachial plexus block performed by orthopedic surgeons.
MATERIALS AND METHODS
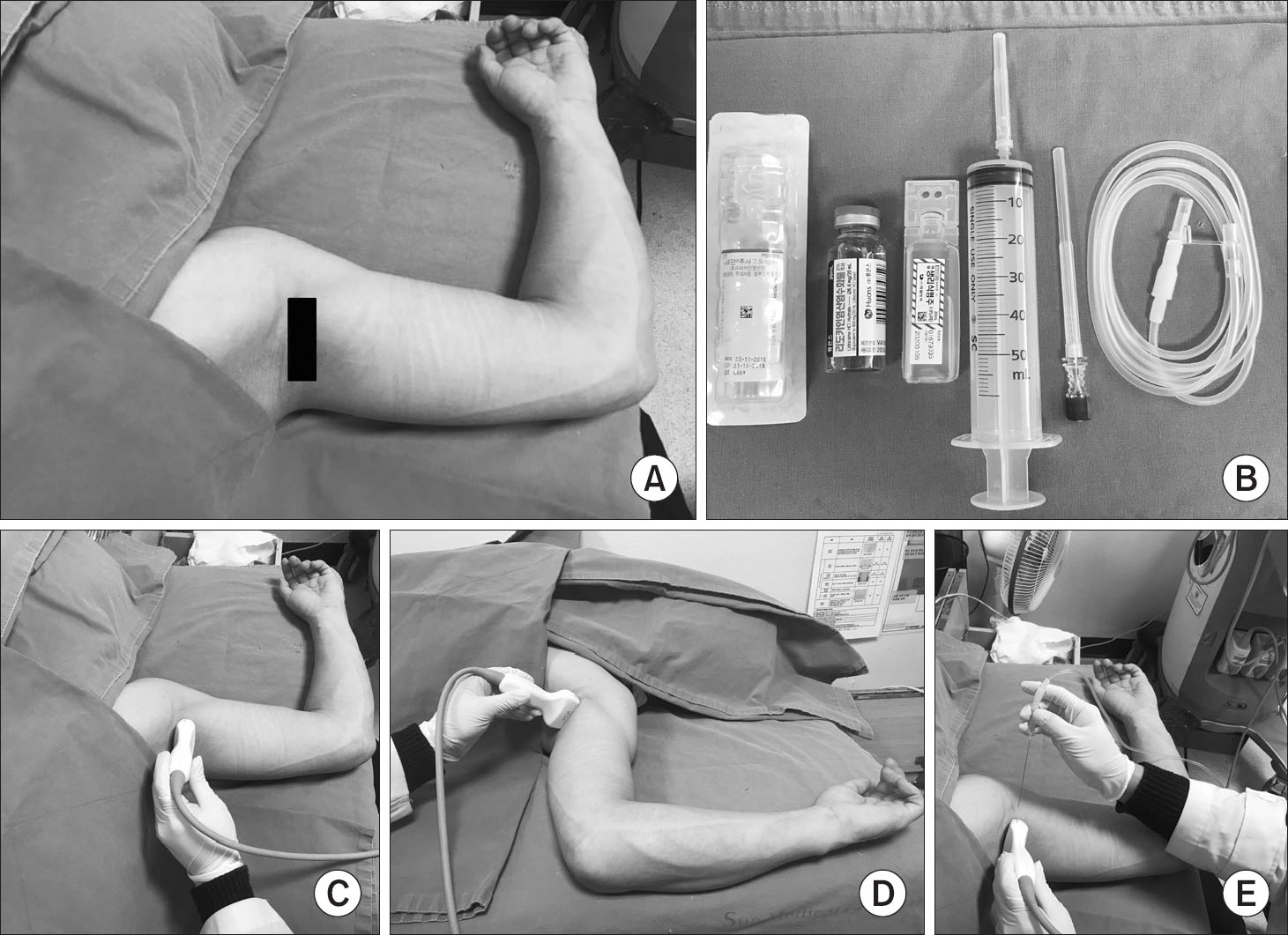
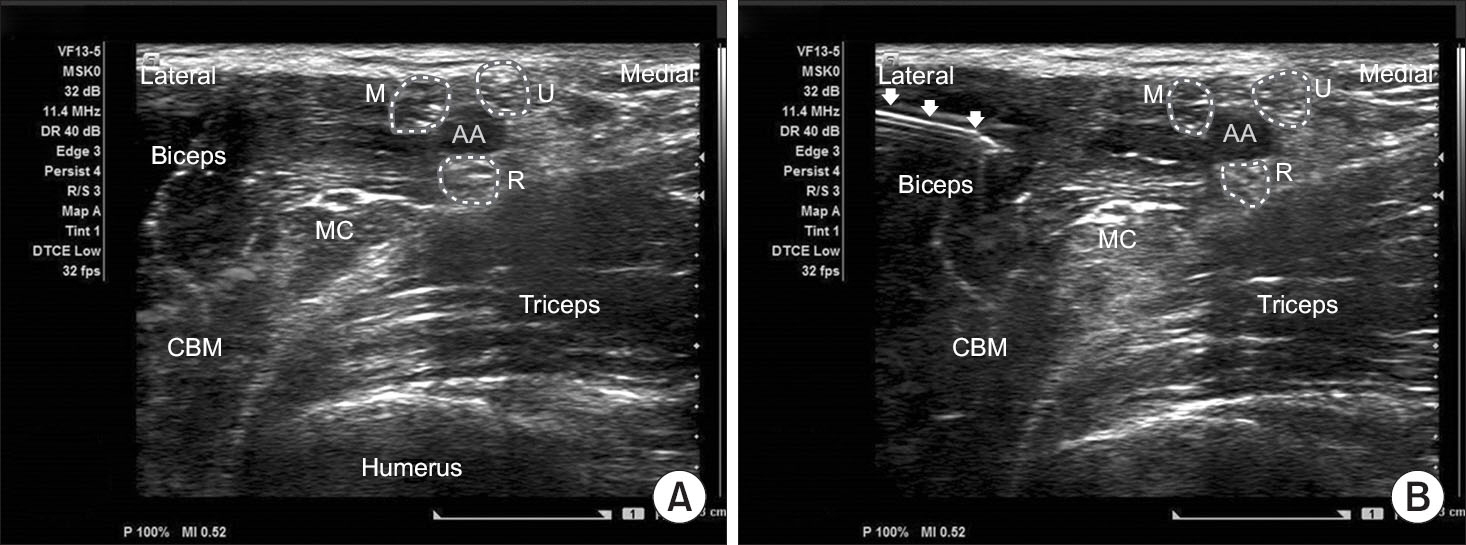
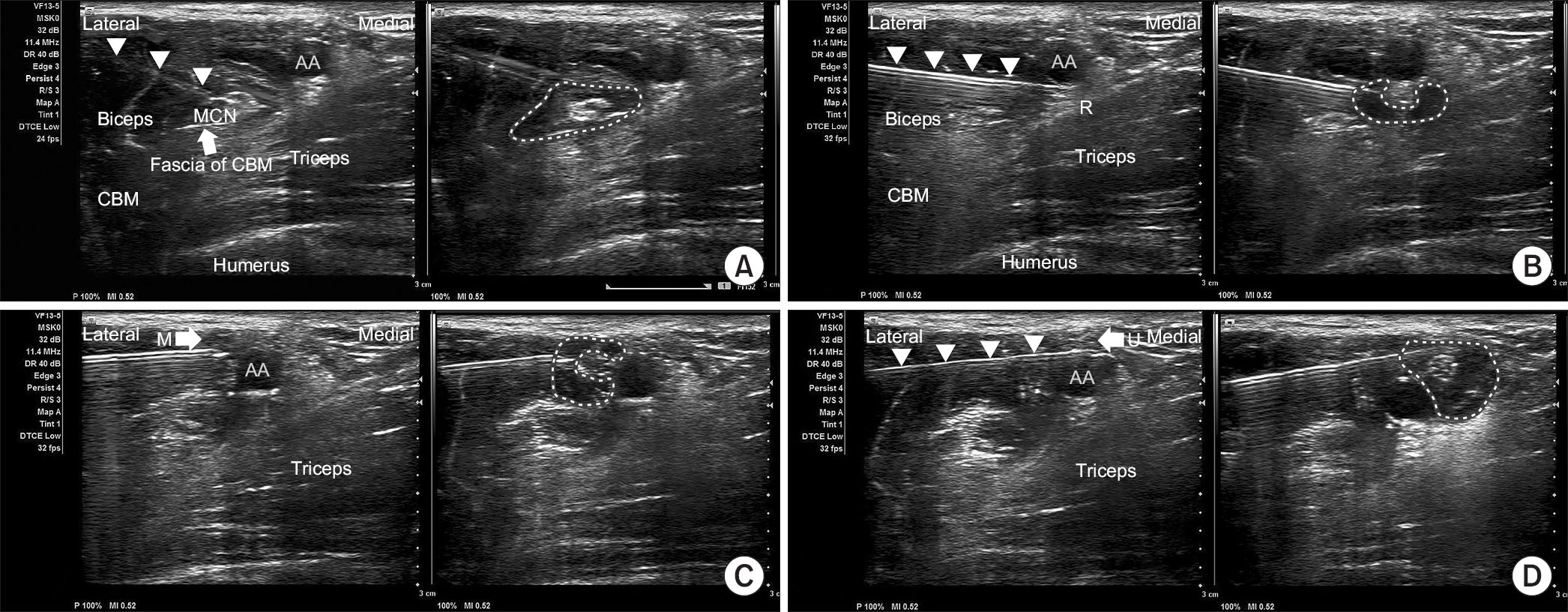
From March to May 2017, an ultrasound-guided axillary brachial plexus block was performed on a total of 103 cases of surgery. A VF13-5 transducer from Siemens Acuson X300 was used. The surgical site was included in the range of the anatomic sensory distribution of the blocked nerve, except for the case where an operation time of more than 2 hours was expected due to multiple injuries and the operation of the upper arm. The procedure was performed by 2 orthopedic surgeons in the same method using 50 ml of solution (20 ml of lidocaine HCl in 2%, 20 ml of ropivacaine in 0.75%, 10 ml of normal saline in 0.9%). The success rate of anesthesia induction during surgery, anesthetic induction time, anatomical range of operation, duration of postoperative analgesia and complications were investigated.
RESULTS
The results from the 2 practices were similar. The anesthesia was successful in 100 out of 103 patients (97.1%). In these patients, the average needling time was 5.5 minutes (2.5-13.2 minutes), the average induction time to complete anesthesia was 18.4 minutes (5-40 minutes), and the average duration of postoperative analgesia was 402.8 minutes (141-540 minutes). The post-anesthesia immediate complications were dizziness in 1 case, nausea and vomiting in 4 cases, and peri-oral numbness in 2 cases, but surgery was performed without problems. All these 7 cases with complications recovered on the same day. A total of 3 cases failed with anesthesia, and they were treated by an injection with local anesthesia in the operation room in 2 cases and switched to general anesthesia in 1 case.
CONCLUSION
An ultrasound-guided axillary brachial plexus block, which was performed by orthopedic surgeons allows anesthesia in a brief period and the high success rates of anesthesia for certain surgeries of the elbow and surgeries on forearm, wrist and hand. Therefore, it can reduce the waiting time to the operating room. This technique is a relatively safe procedure and dose selective anesthesia is possible.
MeSH Terms
Figure
Cited by 1 articles
-
Ultrasound-Guided Axillary Brachial Plexus Block Performed by OIrthopedic Surgeon for Distal Radius Fracture Surgery
Doohoon Sun, Chul-Hyung Lee, Cheol-U Kim, Deukhee Jung, Chung-Han An
Arch Hand Microsurg. 2019;24(2):152-161. doi: 10.12790/ahm.2019.24.2.152.
Reference
-
1. De Jong RH. Axillary block of the brachial plexus. Anesthesiology. 1961; 22:215–25.2. Hartung HJ, Rupprecht A. The axillary brachial plexus block. A study of 178 patients. Reg Anaesth. 1989; 12:21–4.3. Smith BL. Efficacy of a nerve stimulator in regional analgesia; experience in a resident training programme. Anaesthesia. 1976; 31:778–82.
Article4. Kapral S, Krafft P, Eibenberger K, Fitzgerald R, Gosch M, Weinstabl C. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994; 78:507–13.
Article5. Kang C, Hwang DS, Kim YM. . Ultrasound-guided femorosciatic nerve block by orthopaedist for ankle fracture operation. J Korean Foot Ankle Soc. 2010; 14:90–6.6. Zaric D, Nydahl PA, Philipson L, Samuelsson L, Heierson A, Axelsson K. The effect of continuous lumbar epidural infusion of ropivacaine (0.1%, 0.2%, and 0.3%) and 0.25% bupivacaine on sensory and motor block in volunteers: a double-blind study. Reg Anesth. 1996; 21:14–25.7. Venieratos D, Anagnostopoulou S. Classification of communications between the musculocutaneous and median nerves. Clin Anat. 1998; 11:327–31.
Article8. Schafhalter-Zoppoth I, Gray AT. The musculocutaneous nerve: ultrasound appearance for peripheral nerve block. Reg Anesth Pain Med. 2005; 30:385–90.9. Lee HY, Kim SH, So KY, Kim DJ. Effects of interscalene brachial plexus block to intra-operative hemodynamics and postoperative pain for arthroscopic shoulder surgery. Korean J Anesthesiol. 2012; 62:30–4.
Article10. Choi IG, Choi YS, Kim YH. . The effects of postoperative brachial plexus block using MgSO(4) on the postoperative pain after upper extremity surgery. Korean J Pain. 2011; 24:158–63.
Article11. de Morais BS, Cruvinel MG, Carneiro FS, Lago F, Silva YP. Postoperative analgesic efficacy of different volumes and masses of ropivacaine in posterior brachial plexus block. Rev Bras Anestesiol. 2012; 62:19–27.
Article12. Marhofer P, Willschke H, Kettner SC. Ultrasound-guided upper extremity blocks-tips and tricks to improve the clinical practice. Paediatr Anaesth. 2012; 22:65–71.13. Aysel I, Topçu I, Kurt FF. Ultrasound guided brachial plexus block can be advantageous in patients with avulsion type upper extremity injuries. Agri. 2013; 25:145–6.
Article14. Sultan SF, Iohom G, Saunders J, Shorten G. A clinical assessment tool for ultrasound-guided axillary brachial plexus block. Acta Anaesthesiol Scand. 2012; 56:616–23.
Article15. Perlas A, Lobo G, Lo N, Brull R, Chan VW, Karkhanis R. Ultrasound-guided supraclavicular block: outcome of 510 consecutive cases. Reg Anesth Pain Med. 2009; 34:171–6.16. O’Donnell BD, Ryan H, O'sullivan O, Iohom G. Ultrasound-guided axillary brachial plexus block with 20 millili-ters local anesthetic mixture versus general anesthesia for upper limb trauma surgery: an observer-blinded, prospective, randomized, controlled trial. Anesth Analg. 2009; 109:279–83.
Article17. Ootaki C, Hayashi H, Amano M. Ultrasound-guided infraclavicular brachial plexus block: an alternative technique to anatomical landmark-guided approaches. Reg Anesth Pain Med. 2000; 25:600–4.
Article18. Luyet C, Schüpfer G, Wipfli M, Greif R, Luginbühl M, Eichenberger U. Different learning curves for axillary brachial plexus block: ultrasound guidance versus nerve stimulation. Anesthesiol Res Pract. 2010; 2010:309462.
Article19. Rongstad K, Mann RA, Prieskorn D, Nichelson S, Horton G. Popliteal sciatic nerve block for postoperative analgesia. Foot Ankle Int. 1996; 17:378–82.
Article20. Rah JH, Kwon SM, Cha JH, Lee JP, Kim JH. The efficacy of ultrasound-guided brachial plexus block in trauma patients. J Korean Soc Surg Hand. 2014; 19:13–8.
Article21. Tetzlaff JE, Walsh M, Yoon HJ. PH adjustment of mepivacaine decreases the incidence of tourniquet pain during axillary brachial plexus anaesthesia. Can J Anaesth. 1993; 40:133–6.
Article22. Tetzlaff JE, Yoon HJ, Walsh M. Regional anaesthetic technique and the incidence of tourniquet pain. Can J Anaesth. 1993; 40:591–5.
Article23. Stan TC, Krantz MA, Solomon DL, Poulos JG, Chaouki K. The incidence of neurovascular complications following axillary brachial plexus block using a transarterial approach. A prospective study of 1,000 consecutive patients. Reg Anesth. 1995; 20:486–92.24. Andersson A, Akeson J, Dahlin LB. Efficacy and safety of axillary brachial plexus block for operations on the hand. Scand J Plast Reconstr Surg Hand Surg. 2006; 40:225–9.
Article25. Bernucci F, Gonzalez AP, Finlayson RJ, Tran DQ. A prospective randomized comparison between perivascular and perineural ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med. 2012; 37:473–7.
Article26. Ranganath A, Srinivasan KK, Iohom G. Ultrasound guided axillary brachial plexus block. Med Ultrason. 2014; 16:246–51.
Article27. Moore KL, Dalley AF. Clinically oriented anatomy. 1999. 4th ed. Philadelphia: Lippincott Willams& Wilkins;p. 699–712.28. Thompson GE, Rorie DK. Functional anatomy of the brachial plexus sheaths. Anesthesiology. 1983; 59:117–22.
Article29. Jung MJ, Byun HY, Lee CH, Moon SW, Oh MK, Shin H. Medial antebrachial cutaneous nerve injury after brachial plexus block: two case reports. Ann Rehabil Med. 2013; 37:913–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-Guided Axillary Brachial Plexus Block Performed by OIrthopedic Surgeon for Distal Radius Fracture Surgery
- Comparison of Axillary and Supraclavicular Approach in Ultrasound-Guided Brachial Plexus Block
- Bilateral variant locations of the musculocutaneous nerve during ultrasound-guided bilateral axillary brachial plexus block: A case report
- Proximal Median Neuropathy Caused by Axillary Brachial Plexus Block
- Ultrasound-guided Continuous Axillary Brachial Plexus Block Using a Nerve Stimulating Catheter: EpiStim(R) Catheter