J Korean Med Assoc.
2018 Dec;61(12):724-731. 10.5124/jkma.2018.61.12.724.
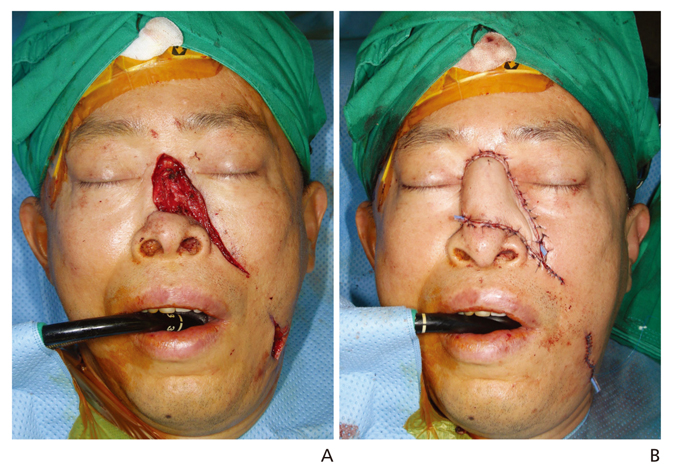
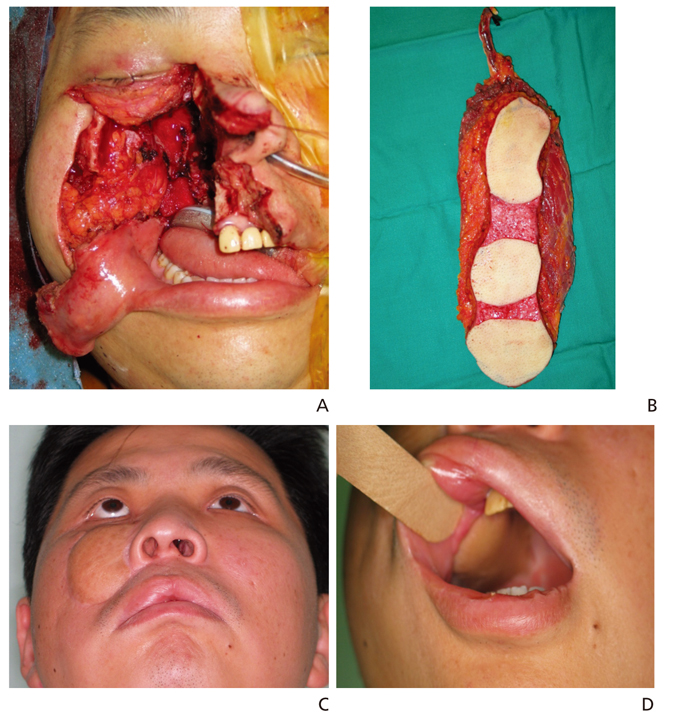
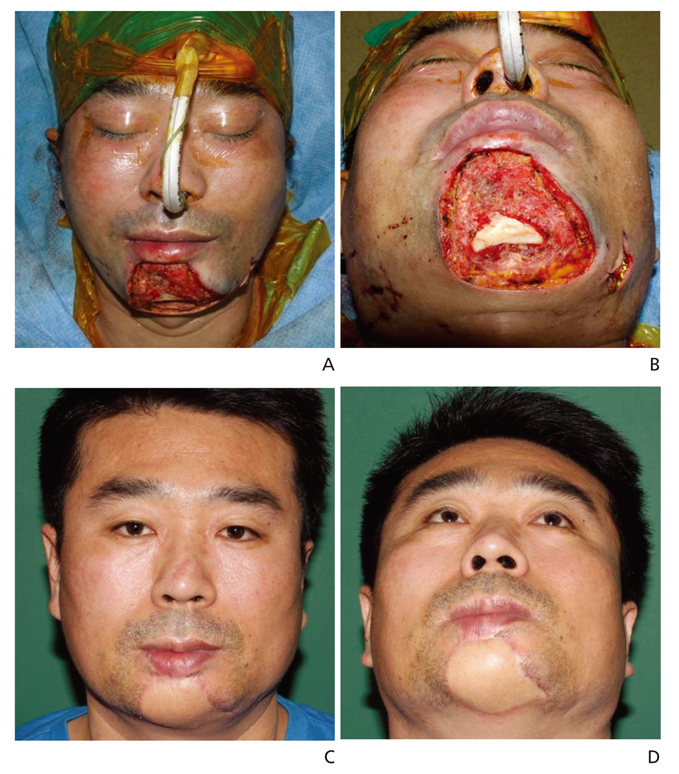
Microsurgical reconstruction of posttraumatic large soft tissue defects on face
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Yonsei University College of Medicine, Seoul, Korea. pswjlee@yuhs.ac
- KMID: 2429336
- DOI: http://doi.org/10.5124/jkma.2018.61.12.724
Abstract
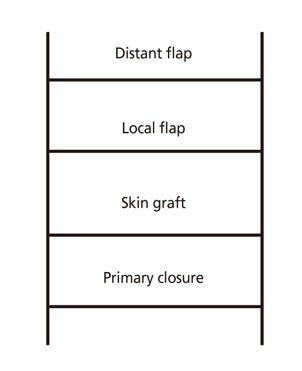
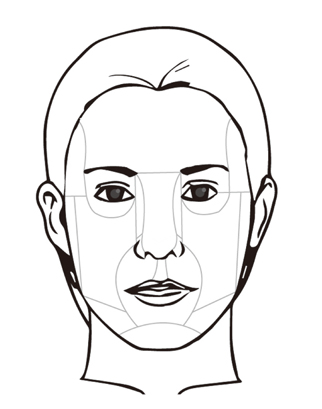
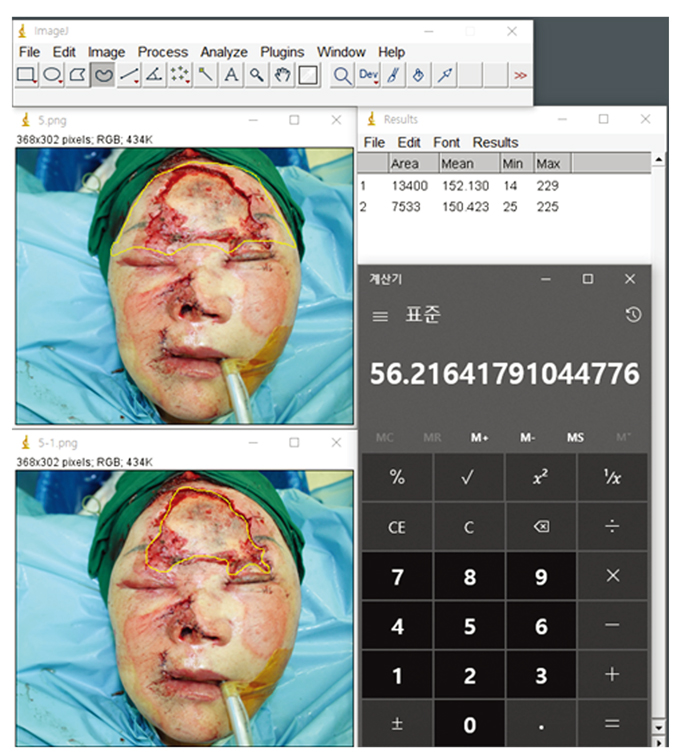
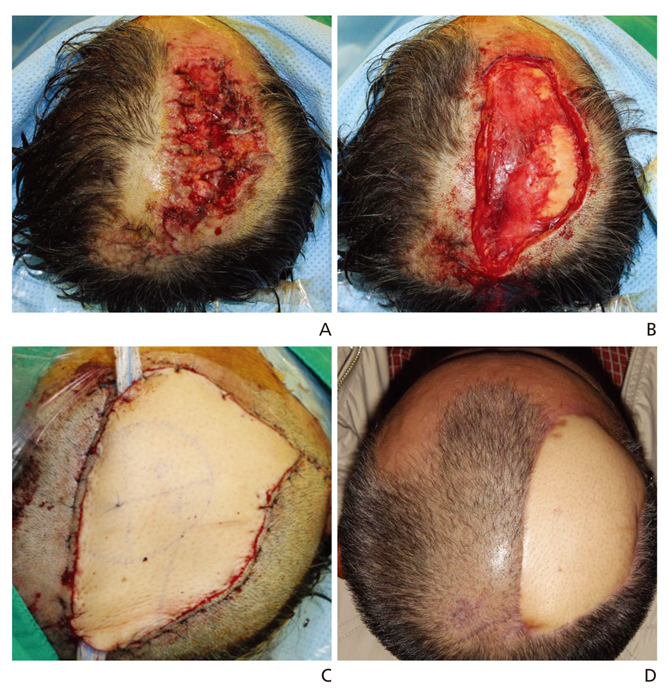
- Our faces can express a remarkable range of subtle emotions and silent messages. Because the face is so essential for complex social interactions that are part of our everyday lives, aesthetic repair and restoration of function are an important tasks that we must not take lightly. Soft-tissue defects occur in trauma patients and require thorough evaluation, planning, and surgical treatment to achieve optimal functional and aesthetic outcomes, while minimizing the risk of complications. Recognizing the full nature of the injury and developing a logical treatment plan help determine whether there will be future aesthetic or functional deformities. Proper classification of the wound enables appropriate treatment, and helps predict the postoperative appearance and function. Comprehensive care of trauma patients requires a diverse breadth of skills, beginning with an initial evaluation, followed by resuscitation. Traditionally, facial defects have been managed with closure or grafting, and prosthetic obturators. Sometimes, however, large defects cannot be closed using simple methods. Such cases, which involve exposure of critical structures, bone, joint spaces, and neurovascular structures, requires more complex treatment. We reviewed and classified causes of significant trauma resulting in facial injuries that were reconstructed by microsurgical techniques without simple sutures or coverage with partial flaps. A local flap is a good choice for reconstruction, but large defects are hard to cover with a local flap alone. Early microsurgical reconstruction of a large facial defect is an excellent choice for aesthetic and functional outcomes.
MeSH Terms
Figure
Reference
-
1. Janis JE, Kwon RK, Attinger CE. The new reconstructive ladder: modifications to the traditional model. Plast Reconstr Surg. 2011; 127:Suppl 1. 205S–212S.
Article2. Neligan Peter C., Warren Richard J.. Plastic Surgery-Principles. 1:Elsevier Health Sciences;2012. p. 534–538.3. Papel ID, Frodel JL, Holt GR, Larrabee WF, Nachlas NE, Park SS, Sykes JM. Facial plastic and reconstructive surgery. 4th ed. New York: Thieme;2016.4. Fattahi TT. An overview of facial aesthetic units. J Oral Maxillofac Surg. 2003; 61:1207–1211.
Article5. Gonzalez-Ulloa M. Skin Grafting: Restoration of the Face Covering by Means of Selected Skin in Regional Esthetic Units. Plast Reconstr Surg. 1957; 19(4):350.6. Byun IH, Byun D, Baek WY. Facial flap repositioning in posttraumatic facial asymmetry. Arch Craniofac Surg. 2016; 17:240–243.
Article7. McCarthy CM, Cordeiro PG. Microvascular reconstruction of oncologic defects of the midface. Plast Reconstr Surg. 2010; 126:1947–1959.
Article8. Costa H, Zenha H, Sequeira H, Coelho G, Gomes N, Pinto C, Martins J, Santos D, Andresen C. Microsurgical reconstruction of the maxilla: algorithm and concepts. J Plast Reconstr Aesthet Surg. 2015; 68:e89–e104.
Article9. Santamaria E, de la Concha E. Lessons learned from delayed versus immediate microsurgical reconstruction of complex maxillectomy and midfacial defects: experience in a tertiary center in Mexico. Clin Plast Surg. 2016; 43:719–727.
Article10. Kim YH, Kim GH, Kim SW. Reconstruction of a complex scalp defect after the failure of free flaps: changing plans and strategy. Arch Craniofac Surg. 2017; 18:112–116.
Article11. Nichter LS, Morgan RF, Nichter MA. The impact of Indian methods for total nasal reconstruction. Clin Plast Surg. 1983; 10:635–647.12. Thornton JF, Weathers WM. Nasolabial flap for nasal tip reconstruction. Plast Reconstr Surg. 2008; 122:775–781.
Article13. Goh CS, Perrett JG, Wong M, Tan BK. Delayed bipedicled nasolabial flap in facial reconstruction. Arch Plast Surg. 2018; 45:253–258.
Article14. Choi JS, Bae YC, Nam SB, Bae SH, Kim GW. Evaluation of the donor site after the median forehead flap. Arch Plast Surg. 2018; 45:259–265.
Article15. Kim KP, Sim HS, Choi JH, Lee SY, Lee DH, Kim SH, Kim HM, Hwang JH, Kim KS. The versatility of cheek rotation flaps. Arch Craniofac Surg. 2016; 17:190–197.
Article16. Jeong HH, Hong JP, Suh HS. Thin elevation: a technique for achieving thin perforator flaps. Arch Plast Surg. 2018; 45:304–313.
Article17. Park SO, Chang H, Imanishi N. Anatomic basis for flap thinning. Arch Plast Surg. 2018; 45:298–303.
Article18. Park BY. Flap thinning: defatting after conventional elevation. Arch Plast Surg. 2018; 45:314–318.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of Large Defects of the Face Utilizing Purse-String Suture
- Reconstruction of the Tissue Defects of Extremities with Anterolateral Thigh Free Flap
- Microsurgical reconstruction for traumatic hand defects in pediatric patients
- Platysma myocutaneous flap - its current role in reconstructive surgery of oral soft tissue defects
- The Use Of A Variety Of Intraoral Flaps In Reconstruction Of Intraoral Soft Tissue Defects