J Menopausal Med.
2018 Apr;24(1):1-10. 10.6118/jmm.2018.24.1.1.
Therapeutic Approaches to Atrophic Vaginitis in Postmenopausal Women: A Systematic Review with a Network Meta-analysis of Randomized Controlled Trials
- Affiliations
-
- 1Department of Interdisciplinary Program in Biomedical Science, Soonchunhyang University, Asan, Korea.
- 2Department of Obstetrics and Gynecology, Soonchunhyang University College of Medicine, Bucheon, Korea. heeobgy@schmc.ac.kr
- 3Department of Obstetrics and Gynecology, Etemo Clininc, Ulaanbaatar, Mongolia.
- 4Department of Biostatistics, Graduate School of Chung-Ang University, Seoul, Korea.
- KMID: 2429214
- DOI: http://doi.org/10.6118/jmm.2018.24.1.1
Abstract
OBJECTIVES
Atrophic vaginitis (AV), which is common in postmenopausal women, is characterized by vaginal dryness, dyspareunia, and discomfort. There are a variety of therapeutic agents for the treatment of AV, besides hormone replacement therapy. We performed this systematic review to compare the effectiveness of various therapies for symptom improvement in AV patients.
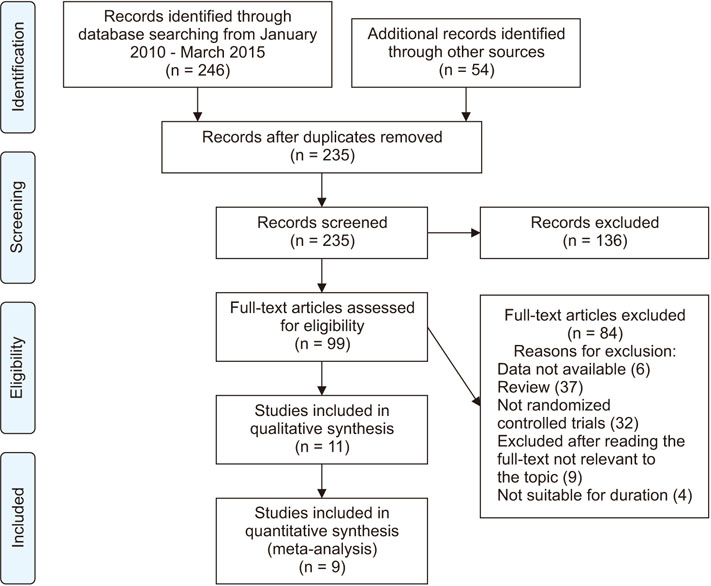
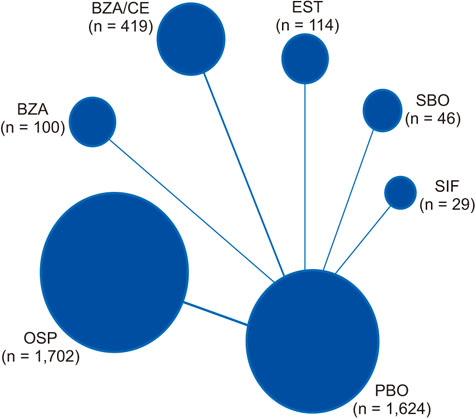
METHODS
We searched the Cochrane Library, EMBASE, MEDLINE, and other literature (Google Scholar, Web of Science, and hand search) for studies published between January 2010 and March 2015. AV was evaluated by the following outcomes: vaginal pH, dyspareunia, vaginal dryness, or cytological change (endometrial thickness, percentages of superficial cells and parabasal cells). They measured treatment efficacy with various outcomes pertaining to AV symptoms.
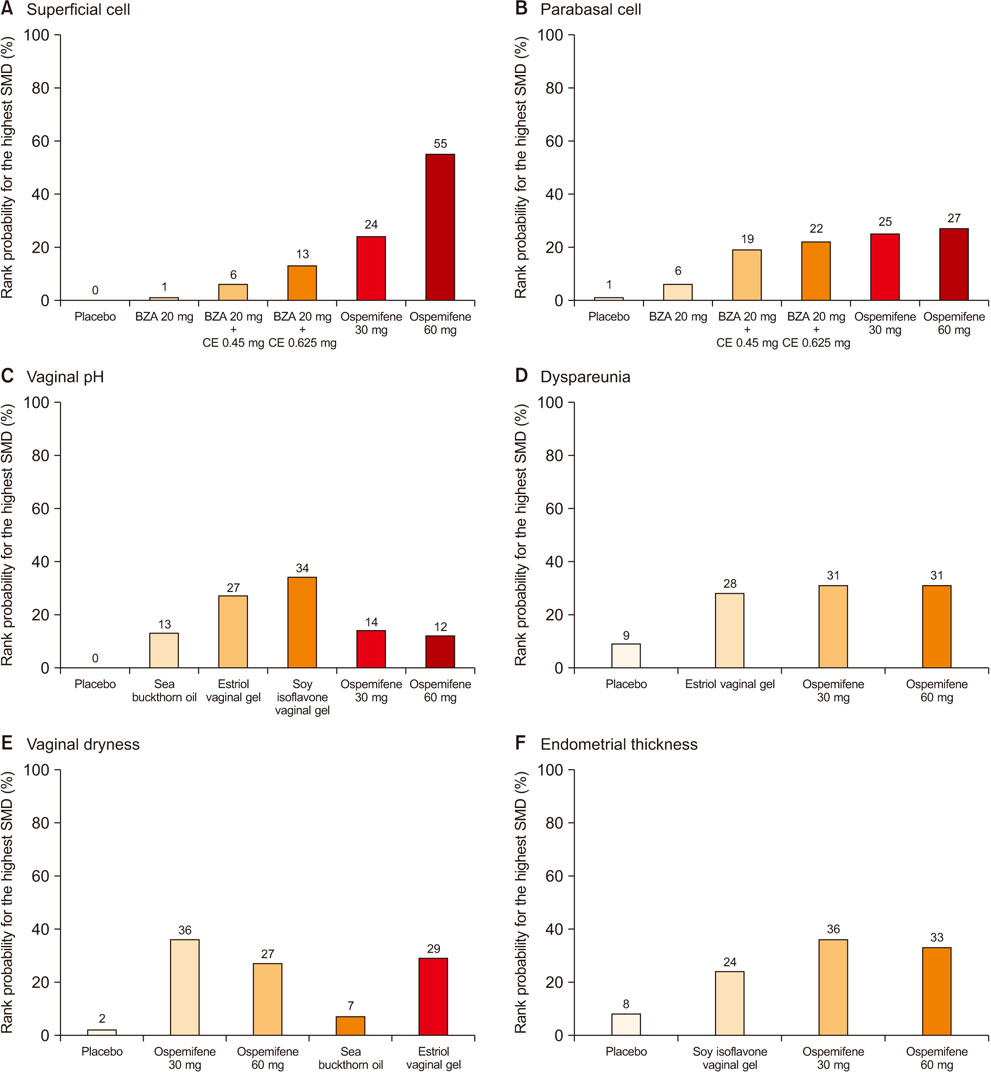
RESULTS
Meta-analysis suggested that ospemifene was effective against dyspareunia, vaginal dryness, endometrial thickness, and percentage changes in superficial and parabasal cells. Vaginal pH was most affected by soy isoflavone vaginal gel. Ospemifene was effective for AV symptoms.
CONCLUSIONS
This systematic review compared the effects of several therapeutic agents on symptoms of AV through a network meta-analysis. This study provides objective evidence for clinical treatment and efficacy management in AV.
MeSH Terms
Figure
Reference
-
1. Nappi RE, Panay N, Bruyniks N, Castelo Branco C, De Villiers TJ, Simon JA. The clinical relevance of the effect of ospemifene on symptoms of vulvar and vaginal atrophy. Climacteric. 2015; 18:233–240.
Article2. Cui Y, Zong H, Yan H, Li N, Zhang Y. The efficacy and safety of ospemifene in treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy: a systematic review and meta-analysis. J Sex Med. 2014; 11:487–497.
Article3. Goldstein I, Dicks B, Kim NN, Hartzell R. Multidisciplinary overview of vaginal atrophy and associated genitourinary symptoms in postmenopausal women. Sex Med. 2013; 1:44–53.
Article4. Kim HK, Kang SY, Chung YJ, Kim JH, Kim MR. The recent review of the genitourinary syndrome of menopause. J Menopausal Med. 2015; 21:65–71.
Article5. Lethaby A, Ayeleke RO, Roberts H. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst Rev. 2016; Cd001500.
Article6. Lee HH, Kim TH, Park J, Lee A, Park Y, Byun DW, et al. Expression of ezrin in vagina cells of postmenopausal rats after dietary administration of omega-3 Fatty Acid formula. J Menopausal Med. 2014; 20:97–103.
Article7. Santen RJ, Pinkerton JV, Conaway M, Ropka M, Wisniewski L, Demers L, et al. Treatment of urogenital atrophy with low-dose estradiol: preliminary results. Menopause. 2002; 9:179–187.
Article8. Wills S, Ravipati A, Venuturumilli P, Kresge C, Folkerd E, Dowsett M, et al. Effects of vaginal estrogens on serum estradiol levels in postmenopausal breast cancer survivors and women at risk of breast cancer taking an aromatase inhibitor or a selective estrogen receptor modulator. J Oncol Pract. 2012; 8:144–148.
Article9. Kagan R, Williams RS, Pan K, Mirkin S, Pickar JH. A randomized, placebo- and active-controlled trial of bazedoxifene/conjugated estrogens for treatment of moderate to severe vulvar/vaginal atrophy in postmenopausal women. Menopause. 2010; 17:281–289.
Article10. Shin JJ, Kim SK, Lee JR, Suh CS. Ospemifene: A novel option for the treatment of vulvovaginal atrophy. J Menopausal Med. 2017; 23:79–84.
Article11. Jaisamrarn U, Triratanachat S, Chaikittisilpa S, Grob P, Prasauskas V, Taechakraichana N. Ultra-low-dose estriol and lactobacilli in the local treatment of postmenopausal vaginal atrophy. Climacteric. 2013; 16:347–355.
Article12. Lima SM, Bernardo BF, Yamada SS, Reis BF, da Silva GM, Galvão MA. Effects of Glycine max (L.) Merr. soy isoflavone vaginal gel on epithelium morphology and estrogen receptor expression in postmenopausal women: a 12-week, randomized, double-blind, placebo-controlled trial. Maturitas. 2014; 78:205–211.
Article13. Larmo PS, Yang B, Hyssala J, Kallio HP, Erkkola R. Effects of sea buckthorn oil intake on vaginal atrophy in postmenopausal women: a randomized, double-blind, placebo-controlled study. Maturitas. 2014; 79:316–321.
Article14. Kim SH, Park ES, Kim TH. Rejuvenation using plateletrich plasma and lipofilling for vaginal atrophy and lichen sclerosus. J Menopausal Med. 2017; 23:63–68.
Article15. DeGregorio MW, Zerbe RL, Wurz GT. Ospemifene: a first-in-class, non-hormonal selective estrogen receptor modulator approved for the treatment of dyspareunia associated with vulvar and vaginal atrophy. Steroids. 2014; 90:82–93.
Article16. Constantine G, Graham S, Portman DJ, Rosen RC, Kingsberg SA. Female sexual function improved with ospemifene in postmenopausal women with vulvar and vaginal atrophy: results of a randomized, placebo-controlled trial. Climacteric. 2015; 18:226–232.
Article17. Cano A, Estèvez J, Usandizaga R, Gallo JL, Guinot M, Delgado JL, et al. The therapeutic effect of a new ultra low concentration estriol gel formulation (0.005% estriol vaginal gel) on symptoms and signs of postmenopausal vaginal atrophy: results from a pivotal phase III study. Menopause. 2012; 19:1130–1139.18. Bachmann GA, Komi JO. Ospemifene effectively treats vulvovaginal atrophy in postmenopausal women: results from a pivotal phase 3 study. Menopause. 2010; 17:480–486.19. Portman D, Palacios S, Nappi RE, Mueck AO. Ospemifene, a non-oestrogen selective oestrogen receptor modulator for the treatment of vaginal dryness associated with postmenopausal vulvar and vaginal atrophy: a randomised, placebo-controlled, phase III trial. Maturitas. 2014; 78:91–98.
Article20. Portman DJ, Bachmann GA, Simon JA. Ospemifene, a novel selective estrogen receptor modulator for treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy. Menopause. 2013; 20:623–630.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of isoflavone on vaginal dryness and dyspareunia in postmenopausal symptoms: a systematic review and meta-analysis
- Vaginal Vitamin E for Treatment of Genitourinary Syndrome of Menopause: A Systematic Review of Randomized Controlled Trials
- Introduction to systematic review and meta-analysis
- Effect of Herbal Medicine on Vaginal Epithelial Cells: A Systematic Review and Meta-analysis
- Efficacy and Safety of Intravaginal Estrogen in the Treatment of Atrophic Vaginitis: A Systematic Review and Meta-Analysis