Clin Exp Otorhinolaryngol.
2018 Sep;11(3):186-191. 10.21053/ceo.2017.01753.
Swing-Door Overlay Tympanoplasty: Surgical Technique and Outcomes
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea. snparkmd@catholic.ac.kr
- KMID: 2429008
- DOI: http://doi.org/10.21053/ceo.2017.01753
Abstract
OBJECTIVES
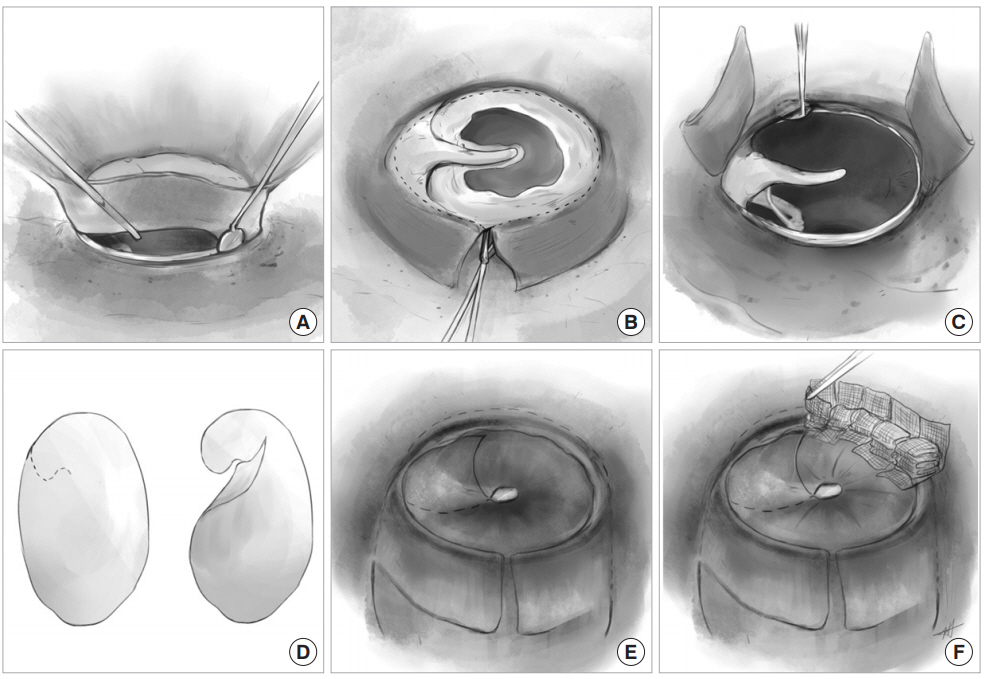
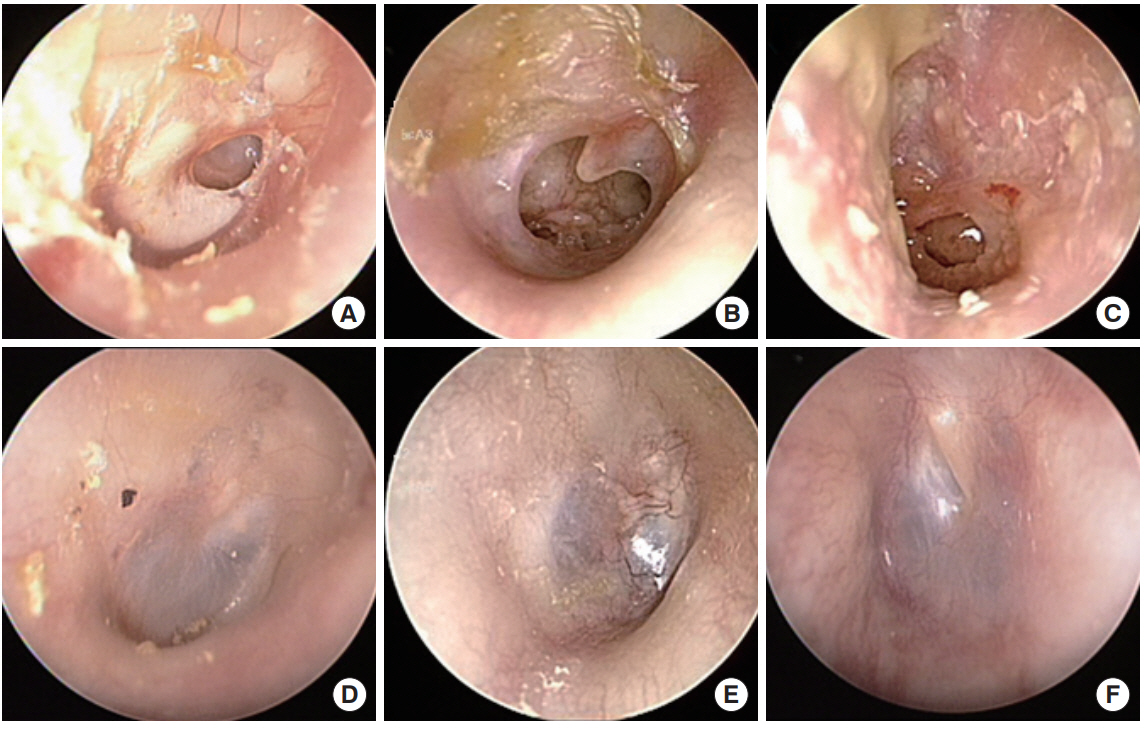
The classical overlay tympanoplasty is technically difficult with some disadvantages and thus less popular. However, it is particularly useful for large, anterior perforations. In this study, we describe the technique of a modified overlay graft in the tympanoplasty coined as the swing-door overlay tympanoplasty and report its outcomes.
METHODS
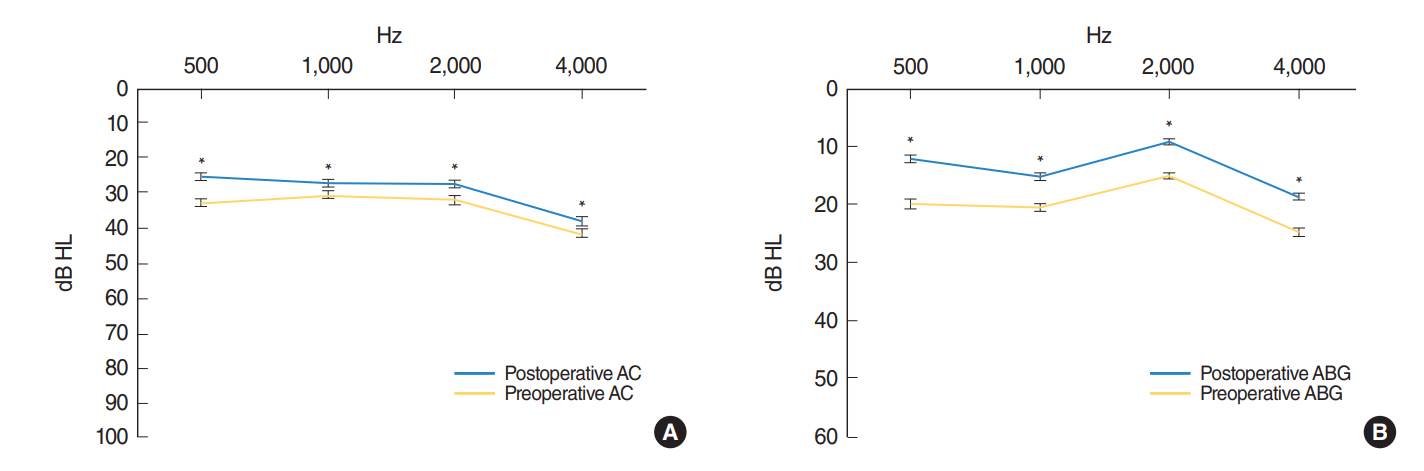
Retrospective review of patients undergoing the swing-door overlay tympanoplasty at a tertiary referral center between 2003 and 2016 was performed. Patient who had ossicular abnormality, previous tympanoplasty, and profound hearing loss were excluded. The surgical technique is described in detail. The outcomes were evaluated by the graft success rate, complication rate, and hearing results. The hearing level was determined by four pure-tone average at 0.5, 1, 2, and 4 kHz. Air-bone gap closure was mainly assessed.
RESULTS
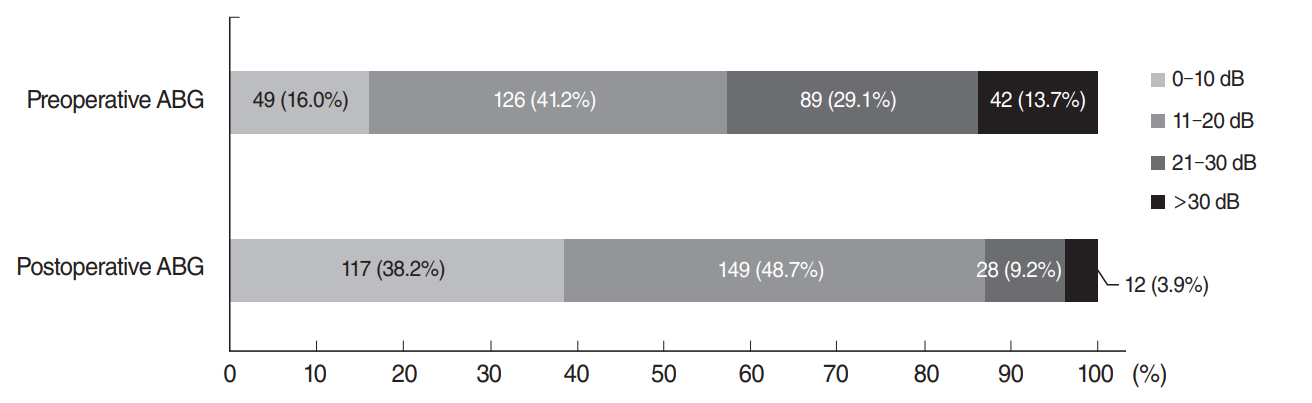
A total of 306 patients (110 males and 196 females) were included. The mean age was 49.1±16.6 years. Follow-up periods ranged from 6 to 108 months with an average of 18.4 months. The overall graft success rate reached 98.4%. Five graft failures occurred with reperforation in three cases and lateralization in two cases. Postoperative complications occurred in 12 cases (3.9%). Air-bone gap changes (closures) were 7.8±12.8, 5.2±12.2, 5.7±10.2, and 6.0± 12.8 dB at 0.5, 1, 2, and 4 kHz, respectively (all P < 0.001) with an average improvement of 6.2 dB. Postoperative airbone gap was closed to ≤20 dB in 86.9%.
CONCLUSION
The swing-door overlay tympanoplasty is a highly successful surgical technique suitable for all types of tympanic membrane perforations. This approach is technically easier than classical overlay tympanoplasty and affords an excellent graft success rate with satisfying hearing results.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Outcomes of Anterior Scutum-Anchoring Tympanoplasty for Reconstruction of Tympanic Membrane Perforation Extending to Anterosuperior Quadrant
Seung Woo Hong, Sung Wook Jeong
Korean J Otorhinolaryngol-Head Neck Surg. 2022;65(4):202-207. doi: 10.3342/kjorl-hns.2021.00465.
Reference
-
1. Briggs RJ, Luxford WM. Chronic ear surgery: a historical review. Am J Otol. 1994; Jul. 15(4):558–67.2. Kartush JM, Michaelides EM, Becvarovski Z, LaRouere MJ. Over-under tympanoplasty. Laryngoscope. 2002; May. 112(5):802–7.
Article3. Farrior JB. The anterior tympanomeatal angle in tympanoplasty: surgical techniques for the prevention of blunting. Laryngoscope. 1983; Aug. 93(8):992–7.4. Jung TT, Park SK. Mediolateral graft tympanoplasty for anterior or subtotal tympanic membrane perforation. Otolaryngol Head Neck Surg. 2005; Apr. 132(4):532–6.
Article5. Schwaber MK. Postauricular undersurface tympanic membrane grafting: some modifications of the “swinging door” technique. Otolaryngol Head Neck Surg. 1986; Sep. 95(2):182–7.
Article6. Rizer FM. Overlay versus underlay tympanoplasty. Part I: historical review of the literature. Laryngoscope. 1997; Dec. 107(12 Pt 2):1–25.
Article7. Stage J, Bak-Pedersen K. Underlay tympanoplasty with the graft lateral to the malleus handle. Clin Otolaryngol Allied Sci. 1992; Feb. 17(1):6–9.
Article8. Yawn RJ, Carlson ML, Haynes DS, Rivas A. Lateral-to-malleus underlay tympanoplasty: surgical technique and outcomes. Otol Neurotol. 2014; Dec. 35(10):1809–12.9. Tos M. Underlay techniques. In : Tos M, editor. Manual of middle ear surgery. Vol 1. New York (NY): Thieme Medical Publishers;1993. p. 188–94.10. Farrior JB. Sandwich graft tympanoplasty: experience, results, and complications. Laryngoscope. 1989; Feb. 99(2):213–7.11. Sergi B, Galli J, De Corso E, Parrilla C, Paludetti G. Overlay versus underlay myringoplasty: report of outcomes considering closure of perforation and hearing function. Acta Otorhinolaryngol Ital. 2011; Dec. 31(6):366–71.12. Nardone M, Sommerville R, Bowman J, Danesi G. Myringoplasty in simple chronic otitis media: critical analysis of long-term results in a 1,000-adult patient series. Otol Neurotol. 2012; Jan. 33(1):48–53.13. Applebaum EL, Deutsch EC. An endoscopic method of tympanic membrane fluorescein angiography. Ann Otol Rhinol Laryngol. 1986; Sep-Oct. 95(5 Pt 1):439–43.
Article14. Schraff S, Dash N, Strasnick B. “Window shade” tympanoplasty for anterior marginal perforations. Laryngoscope. 2005; Sep. 115(9):1655–9.
Article15. Ryan JE, Briggs RJ. Outcomes of the overlay graft technique in tympanoplasty. ANZ J Surg. 2010; Sep. 80(9):624–9.
Article16. Peng R, Lalwani AK. Efficacy of “hammock” tympanoplasty in the treatment of anterior perforations. Laryngoscope. 2013; May. 123(5):1236–40.
Article17. Shim DB, Kim HJ, Kim MJ, Moon IS. Three-point fix tympanoplasty. Acta Otolaryngol. 2015; May. 135(5):429–34.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Variations of the Technique in Endoscopic Tympanoplasty
- Long-Term Surgical Outcome of Canal-Tympanoplasty in Patients With Schuknecht Type B Congenital Aural Stenosis
- Microscopic versus Endoscopic Inlay Butterfly Cartilage Tympanoplasty
- Outcomes of Anterior Scutum-Anchoring Tympanoplasty for Reconstruction of Tympanic Membrane Perforation Extending to Anterosuperior Quadrant
- Inferior Turbinate Swing Approach for Inaccessible Maxillary Sinus Lesions