Clin Exp Otorhinolaryngol.
2018 Sep;11(3):151-157. 10.21053/ceo.2017.01781.
The Clinical Efficacy of Silicone Stents for Endoscopic Dacryocystorhinostomy: A Meta-Analysis
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Otolaryngology-Head and Neck Surgery, Bucheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea. yellobird@catholic.ac.kr
- KMID: 2429003
- DOI: http://doi.org/10.21053/ceo.2017.01781
Abstract
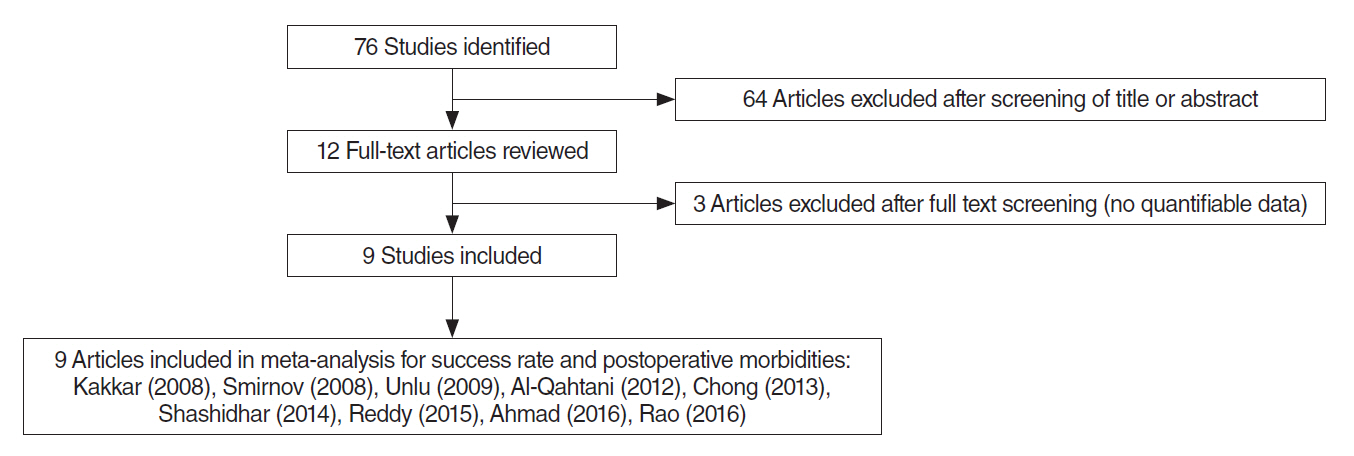
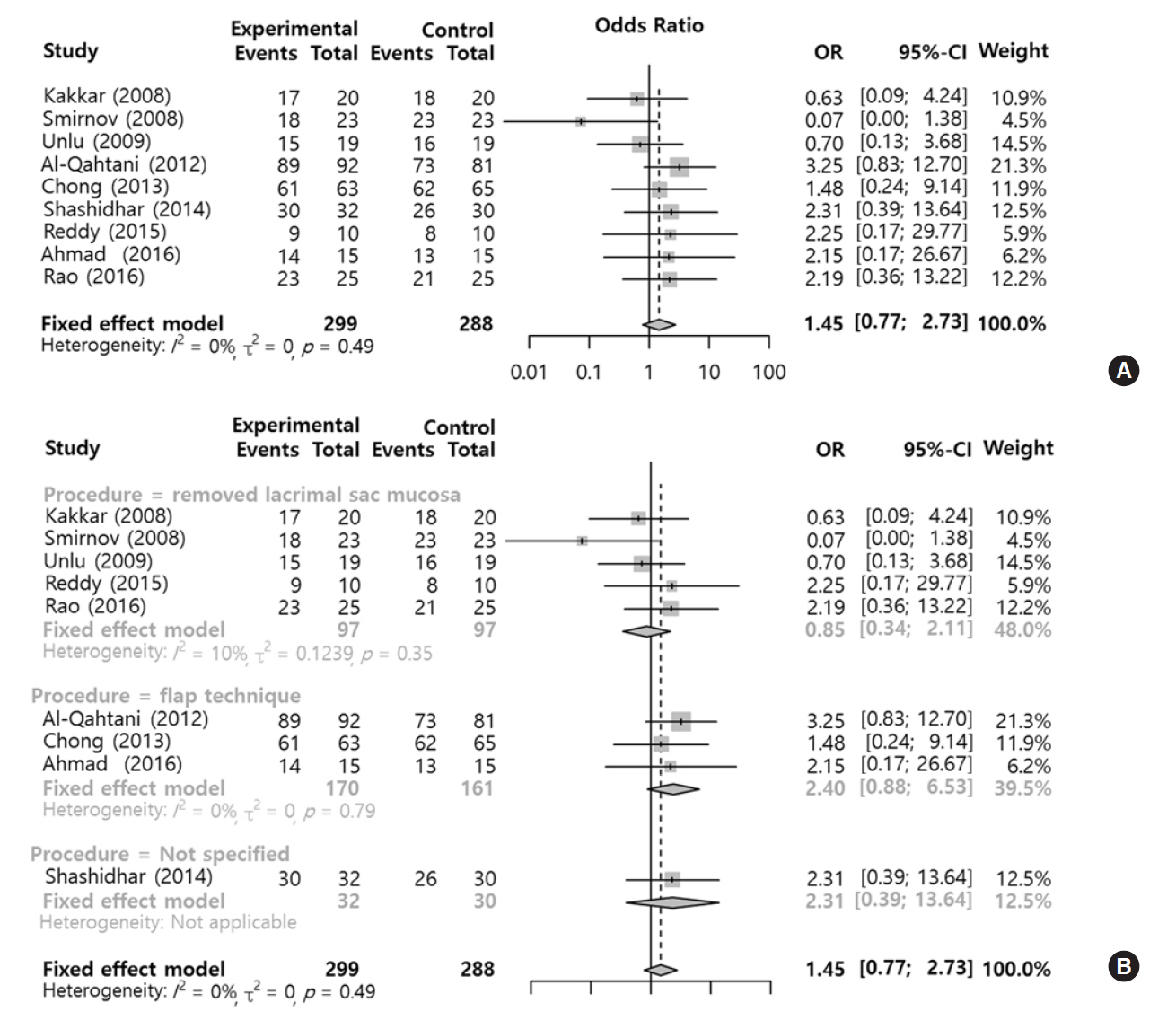
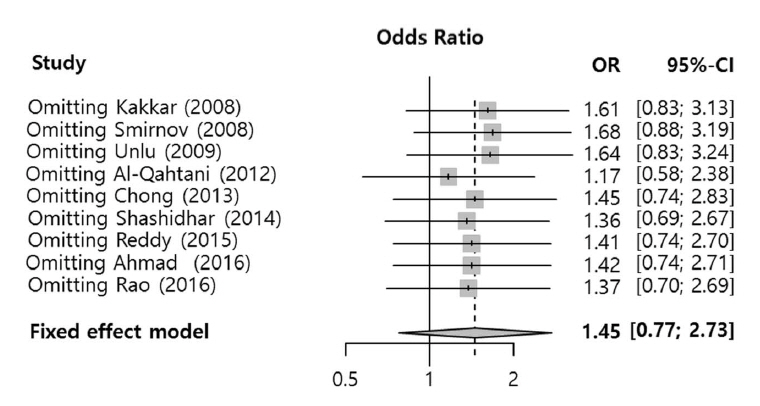
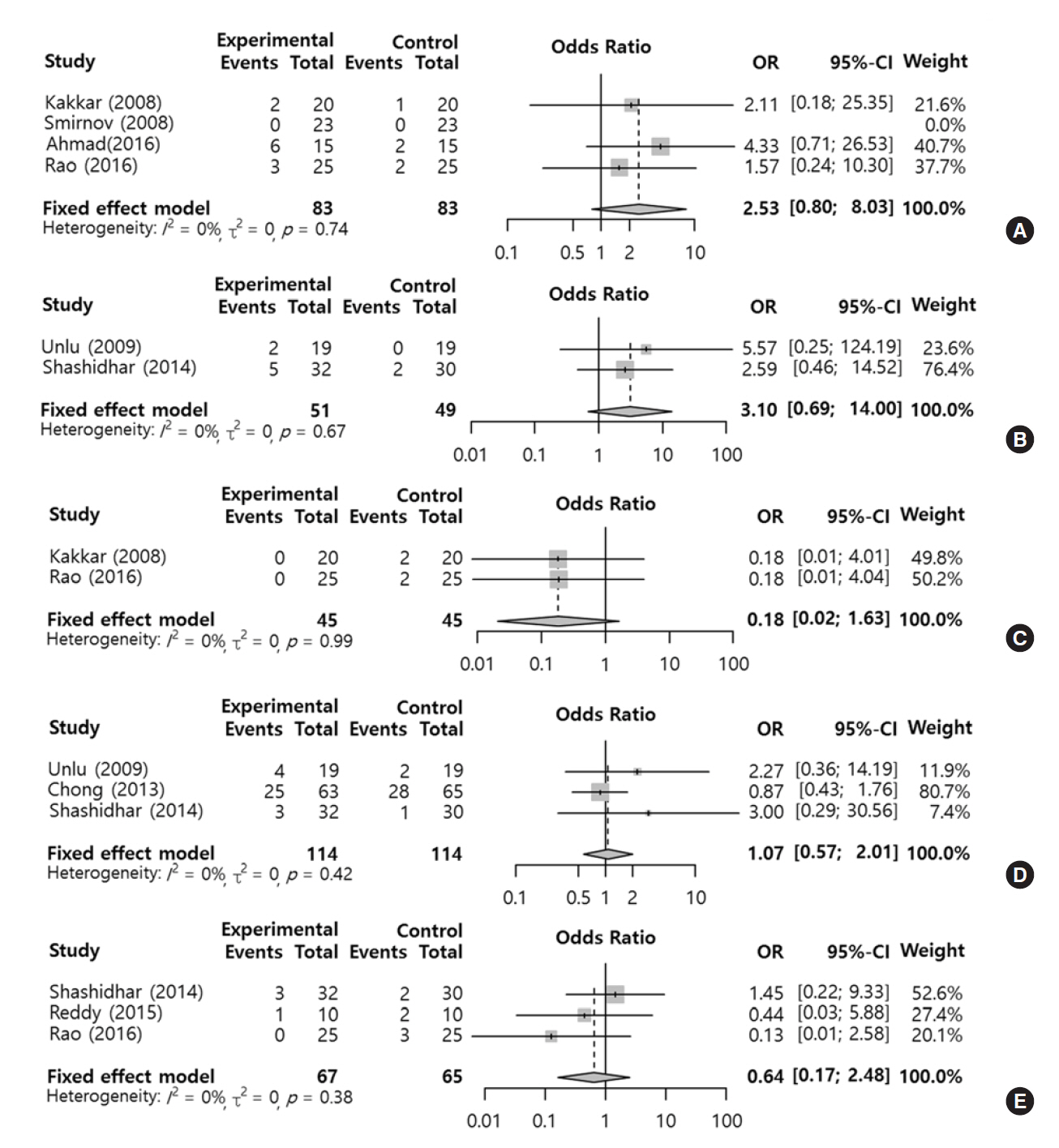
- We evaluated the effect of silicone stent use during endoscopic dacryocystorhinostomy on postoperative morbidities in comparison with versus without a silicone stent. Two authors independently searched six databases (PubMed, Embase, Scopus, the Web of Science, the Cochrane library, and Google Scholar) from inception of article collection to July 2017. The analysis included prospective randomized studies that compared intraoperative silicone stent insertion (silicone group) with no application of a silicone stent (control group), in which the outcomes of interest were success rate (lacrimal passage patent check with syringing, symptom relief, or endoscopic confirmation of fluorescein dye from the opening of Hasner's valve) and morbidities (e.g., postoperative bleeding, rhinostomy closure, granulation tissue, synechia, and eyelid problems) after certain follow-up periods (over 10 weeks). Nine studies involving a total of 587 participants were included. Functional success rates tended to be higher in the silicone group than in the control, but there was no statistically significant difference in success rates (odds ratio, 1.45; 95% confidence interval, 0.77 to 2.73). According to the surgical type such as mucosal removal and mucosal flap surgery, the results from types didn't demonstrate any significant effect, but the mucosal flap technique seemed to be more beneficial. Regarding postoperative morbidities, although the outcomes of the groups did not present any statistically significant difference, eyelid problems and postoperative bleeding tended to occur more frequently in the silicone group, but rhinostomy closure tended to occur more frequently in the control group. Success and morbidity rates showed no difference between the silicone stent group and control group in the meta-analysis. However, additional analyses revealed that the success rate of endonasal dacryocystorhinostomy using silicone intubation with mucosal flap has shown an improving trend, and morbidities such as granulation and synechia showed decreasing trends compared with the group without silicone intubation.
MeSH Terms
Figure
Reference
-
1. Xie C, Zhang L, Liu Y, Ma H, Li S. Comparing the success rate of dacryocystorhinostomy with and without silicone intubation: a trial sequential analysis of randomized control trials. Sci Rep. 2017; May. 7(1):1936.
Article2. Unlu HH, Gunhan K, Baser EF, Songu M. Long-term results in endoscopic dacryocystorhinostomy: is intubation really required? Otolaryngol Head Neck Surg. 2009; Apr. 140(4):589–95.
Article3. Mohamad SH, Khan I, Shakeel M, Nandapalan V. Long-term results of endonasal dacryocystorhinostomy with and without stenting. Ann R Coll Surg Engl. 2013; Apr. 95(3):196–9.
Article4. Smirnov G, Tuomilehto H, Terasvirta M, Nuutinen J, Seppa J. Silicone tubing is not necessary after primary endoscopic dacryocystorhinostomy: a prospective randomized study. Am J Rhinol. 2008; Mar-Apr. 22(2):214–7.
Article5. Unlu HH, Toprak B, Aslan A, Guler C. Comparison of surgical outcomes in primary endoscopic dacryocystorhinostomy with and without silicone intubation. Ann Otol Rhinol Laryngol. 2002; Aug. 111(8):704–9.
Article6. Kakkar V, Chugh J, Sachdeva S, Sharma N, Ramesh. Endoscopic dacryocystorhinostomy with and without silicone stent: a comparative study. J Otolaryngol. 2008; 9(1):7. Al-Qahtani AS. Primary endoscopic dacryocystorhinostomy with or without silicone tubing: a prospective randomized study. Am J Rhinol Allergy. 2012; Jul-Aug. 26(4):332–4.
Article8. Chong KK, Lai FH, Ho M, Luk A, Wong BW, Young A. Randomized trial on silicone intubation in endoscopic mechanical dacryocystorhinostomy (SEND) for primary nasolacrimal duct obstruction. Ophthalmology. 2013; Oct. 120(10):2139–45.
Article9. Shashidhar K, Nagalotimath U, Dixit D. Endoscopic dacryocystorhinostomy with and without silicone stenting: a comparative study. Al Ameen J Med Sci. 2014; Jul. 7(3):244–7.10. Reddy YJ, Reddy YM, Kiran M, Reddy YG, Kumar SP. A comparative study of outcomes of dacryocystorhinostomy with and without silicone stenting. IOSR J Dent Med Sci. 2015; Jul. 14(7):82–5.11. Ahmad S, Pant B. Role of silicone stenting in endoscopic dacryocystorhinostomy: a comparative study. Int J Adv Integr Med Sci. 2016; Jan. 1(1):4–6.
Article12. Rao SV, Rajshekar MM. Dacryocystorhinostomy stent insertion in initial endoscopic dacryocystorhinostomy. Clin Rhinol Int J. 2016; Sep. 9(3):120–4.13. Feng YF, Cai JQ, Zhang JY, Han XH. A meta-analysis of primary dacryocystorhinostomy with and without silicone intubation. Can J Ophthalmol. 2011; Dec. 46(6):521–7.
Article14. Selig YK, Biesman BS, Rebeiz EE. Topical application of mitomycin-C in endoscopic dacryocystorhinostomy. Am J Rhinol. 2000; May-Jun. 14(3):205–7.
Article15. Shah H, Sharma S, Suri N, Patel A. Comparison of surgical outcome in endoscopic dacryocystorhinostomy with and without silicon stent placement. Natl J Med Res. 2013; Jan-Mar. 3(1):34–7.16. Mantynen J, Yoshitsugu M, Rautiainen M. Results of dacryocystorhinostomy in 96 patients. Acta Otolaryngol Suppl. 1997; 529:187–9.17. Allen K, Berlin AJ. Dacryocystorhinostomy failure: association with nasolacrimal silicone intubation. Ophthalmic Surg. 1989; Jul. 20(7):486–9.
Article18. Reifler DM. Results of endoscopic KTP laser-assisted dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 1993; Dec. 9(4):231–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Systematic Review of Benefit of Silicone Intubation in Endoscopic Dacryocystorhinostomy
- The Effects of Placement of Bicanalicular Silicon Tube and Silicone Stent on Granuloma Formation in Endoscopic Intranasal Dacryocystorhinostomy
- Results with Silicone Stent in Lacrimal Drainage System
- Effects of Triamcinolone-soaked Packing for Endonasal Revision in Patients with Failed Endoscopic Dacryocystorhinostomy
- The Effects of Placement of Silicone Tube and e-PTFE Stent in External Dacryocystorhinostomy