Clin Endosc.
2018 Sep;51(5):420-424. 10.5946/ce.2018.150.
Experimental Gastric Non-Balloon Devices
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Gachon University, Gil Medical Center, Incheon, Korea. kkoimge@naver.com
- KMID: 2427714
- DOI: http://doi.org/10.5946/ce.2018.150
Abstract
- Endoscopic bariatric therapies (EBTs) are promising alternatives to the conventional surgeries used to treat obesity and related metabolic conditions, targeting gastrointestinal anatomical and physiological processes. Many EBTs are at various stages of development and are aimed at promoting an early sense of satiety via anatomical and physiological mechanisms. In the present study, we focused on relevant clinical issues and future perspectives with regard to gastric non-balloon methods treating obesity.
MeSH Terms
Figure
Reference
-
1. Bray GA, Frühbeck G, Ryan DH, Wilding JP. Management of obesity. Lancet. 2016; 387:1947–1956.
Article2. Marinos G, Eliades C, Raman Muthusamy V, Greenway F. Weight loss and improved quality of life with a nonsurgical endoscopic treatment for obesity: clinical results from a 3- and 6-month study. Surg Obes Relat Dis. 2014; 10:929–934.
Article3. Sampath K, Rothstein RI. Selected endoscopic gastric devices for obesity. Gastrointest Endosc Clin N Am. 2017; 27:267–275.
Article4. Kushner RF. Weight loss strategies for treatment of obesity. Prog Cardiovasc Dis. 2014; 56:465–472.
Article5. Telem DA, Talamini M, Shroyer AL, et al. Long-term mortality rates (>8-year) improve as compared to the general and obese population following bariatric surgery. Surg Endosc. 2015; 29:529–536.6. Bennett MC, Badillo R, Sullivan S. Endoscopic management. Gastroenterol Clin North Am. 2016; 45:673–688.
Article7. Sullivan S, Edmundowicz SA, Thompson CC. Endoscopic bariatric and metabolic therapies: new and emerging technologies. Gastroenterology. 2017; 152:1791–1801.
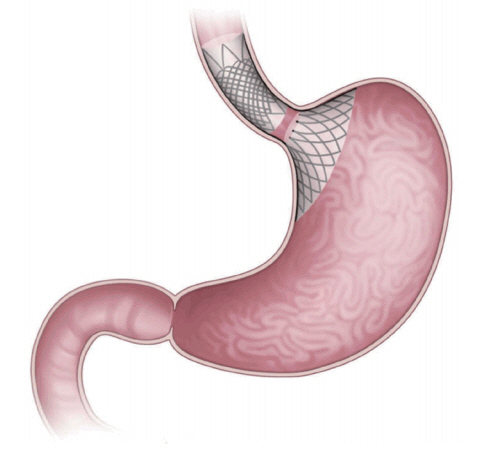
Article8. Verlaan T, de Jong K, de la Mar-Ploem ED, Veldhuyzen EA, Mathus-Vliegen EM, Fockens P. Trans-oral endoscopic restrictive implant system: endoscopic treatment of obesity? Surg Obes Relat Dis. 2016; 12:1711–1718.
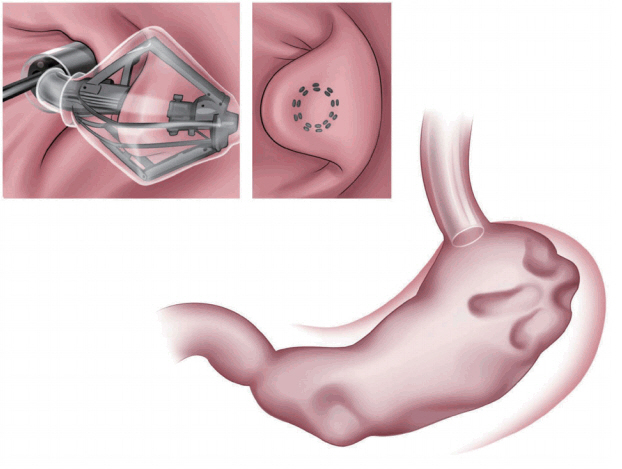
Article9. Verlaan T, Paulus GF, Mathus-Vliegen EM, et al. Endoscopic gastric volume reduction with a novel articulating plication device is safe and effective in the treatment of obesity (with video). Gastrointest Endosc. 2015; 81:312–320.
Article10. Sartoretto A, Sui Z, Hill C, et al. Endoscopic sleeve gastroplasty (ESG) is a reproducible and effective endoscopic bariatric therapy suitable for widespread clinical adoption: a large, international multicenter study. Obes Surg. 2018; 28:1812–1821.
Article11. Lopez-Nava G, Sharaiha RZ, Vargas EJ, et al. Endoscopic sleeve gastroplasty for obesity: a multicenter study of 248 patients with 24 months follow-up. Obes Surg. 2017; 27:2649–2655.12. Familiari P, Costamagna G, Bléro D, et al. Transoral gastroplasty for morbid obesity: a multicenter trial with a 1-year outcome. Gastrointest Endosc. 2011; 74:1248–1258.
Article13. Moreno C, Closset J, Dugardeyn S, et al. Transoral gastroplasty is safe, feasible, and induces significant weight loss in morbidly obese patients: results of the second human pilot study. Endoscopy. 2008; 40:406–413.
Article14. Kumar N. Endoscopic therapy for weight loss: gastroplasty, duodenal sleeves, intragastric balloons, and aspiration. World J Gastrointest Endosc. 2015; 7:847–859.
Article15. Hill C, Khashab MA, Kalloo AN, Kumbhari V. Endoluminal weight loss and metabolic therapies: current and future techniques. Ann N Y Acad Sci. 2018; 1411:36–52.
Article16. Miller K, Turró R, Greve JW, Bakker CM, Buchwald JN, Espinós JC. MILEPOST multicenter randomized controlled trial: 12-month weight loss and satiety outcomes after pose (SM) vs. medical therapy. Obes Surg. 2017; 27:310–322.
Article17. Lopez-Nava G, Bautista-Castaño I, Jimenez A, de Grado T, Fernandez-Corbelle JP. The primary obesity surgery endolumenal (POSE) procedure: one-year patient weight loss and safety outcomes. Surg Obes Relat Dis. 2015; 11:861–865.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Gastric Stricture Caused by Chemical Fertilizer
- The Role of Distal Protection Devices for Cardiovascular Intervention
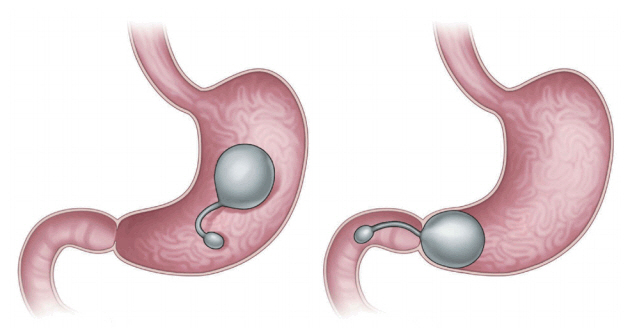
- Gastric Ulceration and Bleeding with Hemodynamic Instability Caused by an Intragastric Balloon for Weight Loss
- A Case of Endoscopic Removal of a Broken off Gastric Balloon from a Sengstaken-Blakemore Tube
- Gastric Varices Treated with Balloon-occluded Retrograde Transvenous Obliteration (BRTO)