J Korean Soc Radiol.
2018 Dec;79(6):337-339. 10.3348/jksr.2018.79.6.337.
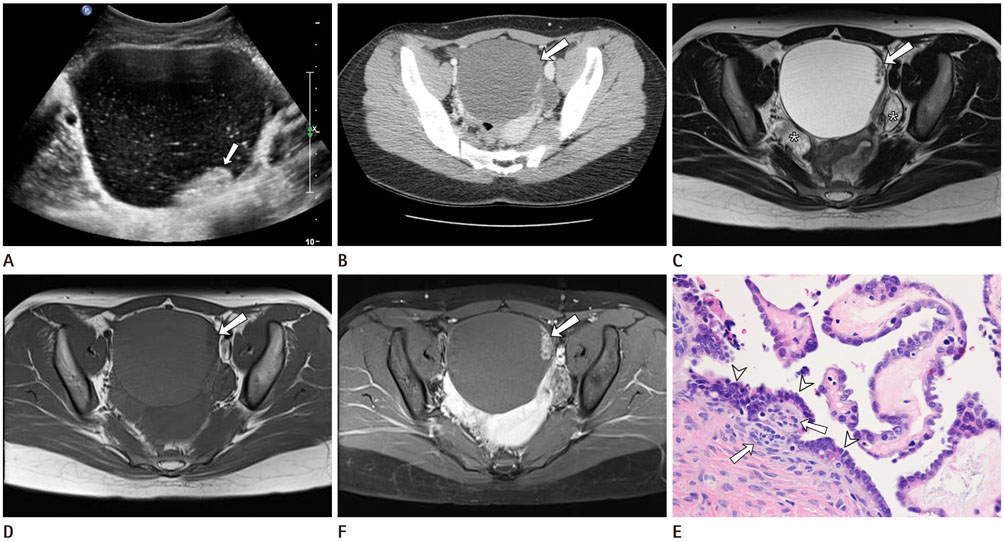
Paraovarian Serous Borderline Tumor: A Case Report
- Affiliations
-
- 1Department of Radiology, Keimyung University, Dongsan Medical Center, Daegu, Korea. kseehdr@dsmc.or.kr
- 2Department of Pathology, Keimyung University, Dongsan Medical Center, Daegu, Korea.
- KMID: 2427382
- DOI: http://doi.org/10.3348/jksr.2018.79.6.337
Abstract
- Parovarian cyst is usually simple cyst, and accounts for 10%-20% of adnexal masses. Borderline or malignant parovarian tumor is rare, and it contains papillary projection at the smooth inner wall. We report the ultrasonography, CT and MRI findings of a parovarian serous borderline tumor in 19-year-old female presenting left lower quadrant abdominal discomfort for 2 days.
MeSH Terms
Figure
Reference
-
1. Zhao F, Zhang H, Ren Y, Kong F. Transvaginal sonographic characteristics of paraovarian borderline tumor. Int J Clin Exp Med. 2015; 8:2684–2688.2. Korbin CD, Brown DL, Welch WR. Paraovarian cystadenomas and cystadenofibromas: sonographic characteristics in 14 cases. Radiology. 1998; 208:459–462.
Article3. Suzuki S, Furukawa S, Kyozuka H, Watanabe T, Takahashi H, Fujimori K. Two cases of paraovarian tumor of borderline malignancy. J Obstet Gynaecol Res. 2013; 39:437–441.
Article4. Bider D, Rabinovitch O, Schinder OM, Menczer J. Parovarian serous cystadenocarcinoma of borderline malignancy diagnosed during pregnancy. Gynecol Obstet Invest. 1988; 26:262–264.
Article5. Altaras MM, Jaffe R, Corduba M, Holtzinger M, Bahary C. Primary paraovarian cystadenocarcinoma: clinical and management aspects and literature review. Gynecol Oncol. 1990; 38:268–272.
Article6. Savelli L, Ghi T, De Iaco P, Ceccaroni M, Venturoli S, Cacciatore B. Paraovarian/paratubal cysts: comparison of transvaginal sonographic and pathological findings to establish diagnostic criteria. Ultrasound Obstet Gynecol. 2006; 28:330–334.
Article7. De Areia AL, Frutuoso C, Amaral N, Dias I, De Oliveira C. Paraovarian tumor of borderline malignancy—a case report. Int J Gynecol Cancer. 2004; 14:680–682.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of paraovarian tumor of boderline malignance
- Serous borderline tumor of the fallopian tube
- A Serous Papillary Cystadenoma of Borderline Malignancy in Testis
- Papillary Serous Cystadenoma of Borderline Malignancy Arising from a Paramesonephric Parovarian Cyst: A case report
- Paratubal serous borderline tumor