J Korean Soc Radiol.
2018 Dec;79(6):332-336. 10.3348/jksr.2018.79.6.332.
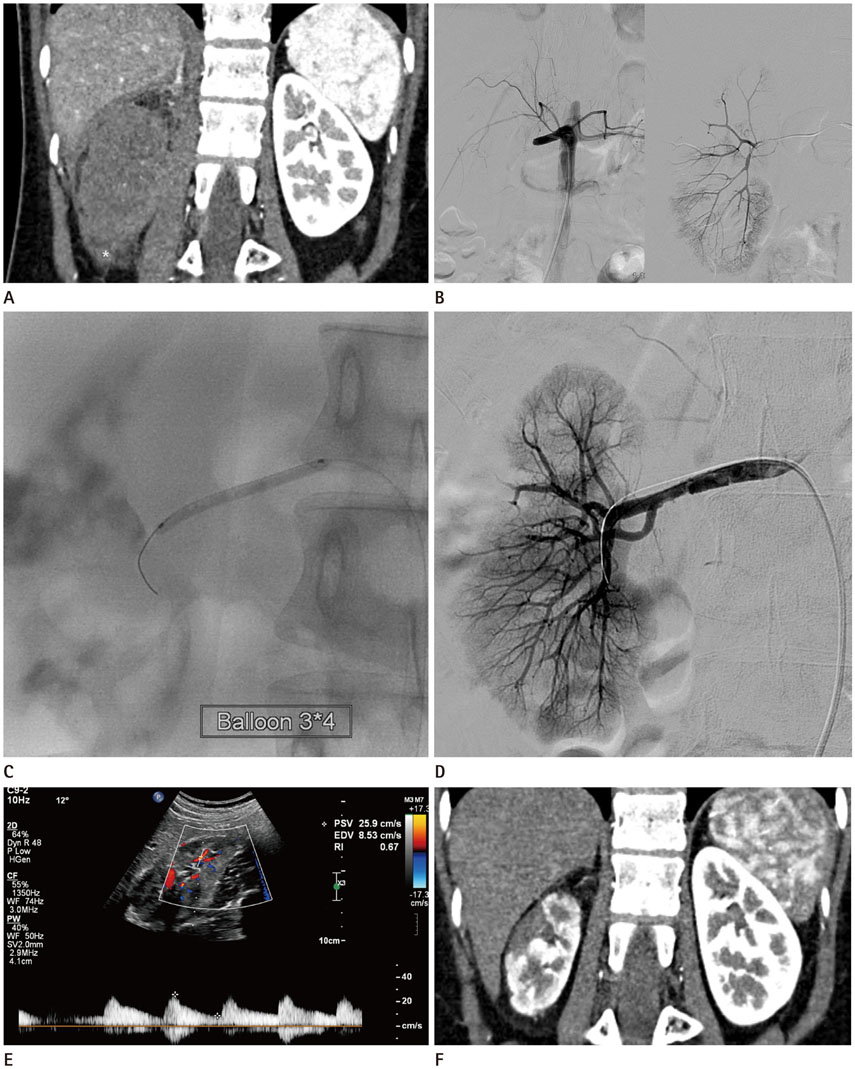
Balloon Angioplasty in a Pediatric Renal Artery Occlusion
- Affiliations
-
- 1Department of Radiology, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 2Department of Radiology, Human Medical Imaging and Intervention Center, Seoul, Korea. humic.jhd@gmail.com
- KMID: 2427381
- DOI: http://doi.org/10.3348/jksr.2018.79.6.332
Abstract
- Renal artery injury is a rare complication in blunt trauma, but can cause devascularization of the kidney, leading to renal failure. It requires early diagnosis and management. The treatment of renal artery injury still remains controversial, but recent studies have reported the successful treatment outcome with endovascular stent placement. Nevertheless, there is no standard treatment strategy in cases of pediatric patients. We report a case of a 16-year-old girl with right renal artery occlusion associated with a grade IV liver laceration. She was treated with only balloon angioplasty, and the kidney showed marked improvement of parenchymal perfusion with normalized renal function. Treatment with only balloon angioplasty can be a treatment option in pediatric patients with renal artery injury.
MeSH Terms
Figure
Reference
-
1. Bruce LM, Croce MA, Santaniello JM, Miller PR, Lyden SP, Fabian TC. Blunt renal artery injury: incidence, diagnosis, and management. Am Surg. 2001; 67:550–554.2. Abu-Gazala M, Shussman N, Abu-Gazala S, Elazary R, Bala M, Rozenberg S, et al. Endovascular management of blunt renal artery trauma. Isr Med Assoc J. 2013; 15:210–215.3. Brown SL, Elder JS, Spirnak JP. Are pediatric patients more susceptible to major renal injury from blunt trauma? A comparative study. J Urol. 1998; 160:138–140.
Article4. Dinchman KH, Spirnak JP. Traumatic renal artery thrombosis: evaluation and treatment. Semin Urol. 1995; 13:90–93.5. Haas CA, Dinchman KH, Nasrallah PF, Spirnak JP. Traumatic renal artery occlusion: a 15-year review. J Trauma. 1998; 45:557–561.
Article6. Spirnak JP, Resnick MI. Revascularization of traumatic thrombosis of the renal artery. Surg Gynecol Obstet. 1987; 164:22–26.7. Cass AS. Renovascular injuries from external trauma. Diagnosis, treatment, and outcome. Urol Clin North Am. 1989; 16:213–220.8. Flye MW, Anderson RW, Fish JC, Silver D. Successful surgical treatment of anuria caused by renal artery occlusion. Ann Surg. 1982; 195:346–353.
Article9. Breyer BN, Master VA, Marder SR, McAninch JW. Endovascular management of trauma related renal artery thrombosis. J Trauma. 2008; 64:1123–1125.
Article10. Yokoyama S, Sekioka A, Utsunomiya H, Shimada K. Traumatic renal artery occlusion associated with a grade III hepatic injury in an 11-year-old boy: a case report. J Pediatr Surg Case Rep. 2014; 2:126–129.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous transluminal angioplasty in Takayasu's arteritis
- One Case of Percutaneous Transluminal Angioplasty of Renal Artery Stenosis Caused by Takayasu's Arteritis
- Aspiration Thromboembolectomy in the Management of Acute Coronary Occlusion during Pertaneous Transluminal Coronary Angioplasty
- Two Cases of Renal Artery Stenosis Caused by Takayasu's Arteritis : Treatment with the Palmaz-Schatz Biliary Stent
- A Case of Renovascular Hypertension Controlled by Percutaneous Transluminal Renal Angioplasty with Balloon Dilatatio