Korean J Radiol.
2017 Dec;18(6):936-945. 10.3348/kjr.2017.18.6.936.
Post-Ischemic Bowel Stricture: CT Features in Eight Cases
- Affiliations
-
- 1Department of Radiology, College of Medicine, Ewha Womans University, Mokdong Hospital, Seoul 07985, Korea.
- 2Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea. leesoolbee@daum.net
- 3Department of Pathology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea.
- 4Department of Radiology, University of Ulsan College of Medicine, Gangneung Asan Hospital, Gangneung 25440, Korea.
- KMID: 2427203
- DOI: http://doi.org/10.3348/kjr.2017.18.6.936
Abstract
OBJECTIVE
To investigate the characteristic radiologic features of post-ischemic stricture, which can then be implemented to differentiate that specific disease from other similar bowel diseases, with an emphasis on computed tomography (CT) features.
MATERIALS AND METHODS
Eight patients with a diagnosis of ischemic bowel disease, who were also diagnosed with post-ischemic stricture on the basis of clinical or pathologic findings, were included. Detailed clinical data was collected from the available electronic medical records. Two radiologists retrospectively reviewed all CT images. Pathologic findings were also analyzed.
RESULTS
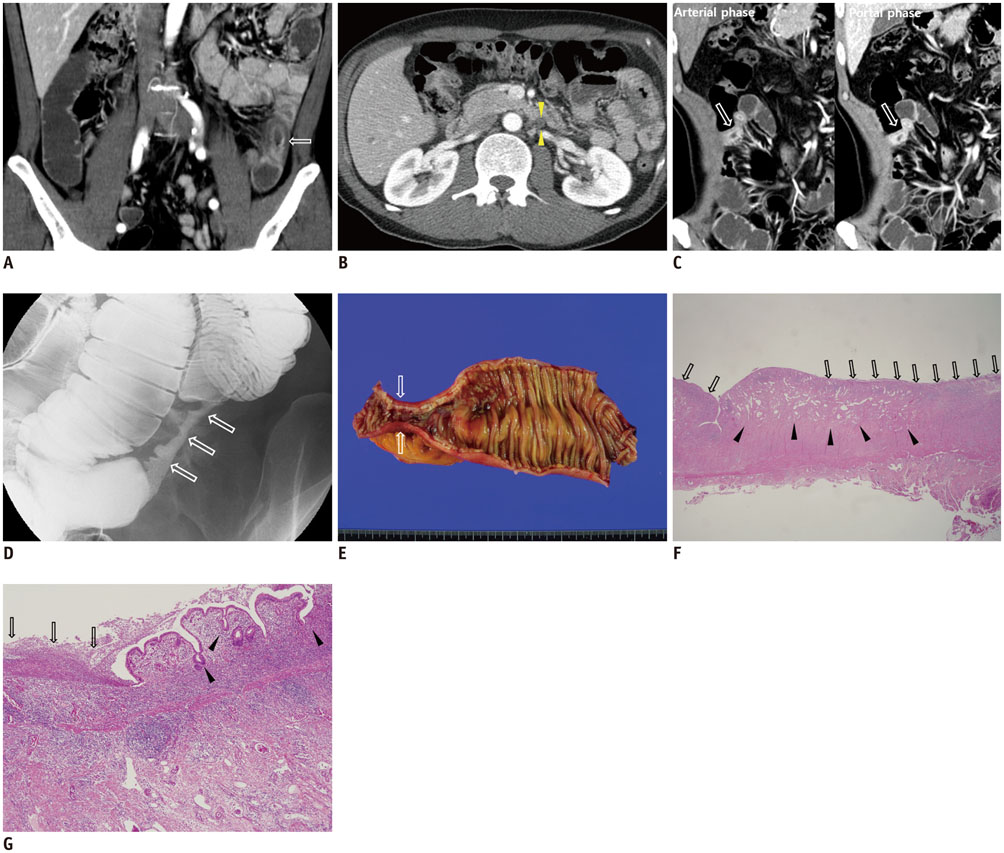
The mean interval between the diagnosis of ischemic bowel disease and stricture formation was 57 days. The severity of ischemic bowel disease was variable. Most post-ischemic strictures developed in the ileum (n = 5), followed by the colon (n = 2) and then the jejunum (n = 1). All colonic strictures developed in the "watershed zone." The pathologic features of post-ischemic stricture were deep ulceration, submucosal/subserosal fibrosis and chronic transmural inflammation. The mean length of the post-ischemic stricture was 7.4 cm. All patients in this study possessed one single stricture. On contrast-enhanced CT, most strictures possessed concentric wall thickening (87.5%), with moderate enhancement (87.5%), mucosal enhancement (50%), or higher enhancement in portal phase than arterial phase (66.7%).
CONCLUSION
Post-ischemic strictures develop in the ileum, jejunum and colon after an interval of several weeks. In the colonic segment, strictures mainly occur in the "watershed zone." Typical CT findings include a single area of concentric wall thickening of medium length (mean, 7.4 cm), with moderate and higher enhancement in portal phase and vasa recta prominence.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Colon/diagnostic imaging/pathology
Constriction, Pathologic
Female
Humans
Ileum/diagnostic imaging/pathology
Inflammatory Bowel Diseases/*diagnosis/diagnostic imaging/pathology
Jejunum/diagnostic imaging/pathology
Male
Middle Aged
Retrospective Studies
Time Factors
*Tomography, X-Ray Computed
Figure
Cited by 1 articles
-
Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.
Reference
-
1. Longstreth GF, Yao JF. Epidemiology, clinical features, highrisk factors, and outcome of acute large bowel ischemia. Clin Gastroenterol Hepatol. 2009; 7:1075–1080.2. Medina C, Vilaseca J, Videla S, Fabra R, Armengol-Miro JR, Malagelada JR. Outcome of patients with ischemic colitis: review of fifty-three cases. Dis Colon Rectum. 2004; 47:180–184.3. Takeuchi N, Naba K. Small intestinal obstruction resulting from ischemic enteritis: a case report. Clin J Gastroenterol. 2013; 6:281–286.4. Kaido T, Kano M, Suzaki S, Yanagibashi K, Shiota M. Colon stenosis caused by old portal vein thrombosis. Abdom Imaging. 2005; 30:358–360.5. Lee-Elliott C, Landells W, Keane A. Using CT to reveal traumatic ischemic stricture of the terminal ileum. AJR Am J Roentgenol. 2002; 178:403–404.6. Lien GS, Mori M, Enjoji M. Delayed posttraumatic ischemic stricture of the small intestine. A clinicopathologic study of four cases. Acta Pathol Jpn. 1987; 37:1367–1137.7. Yamazaki T, Shirai Y, Sakai Y, Hatakeyama K. Ischemic stricture of the rectosigmoid colon caused by division of the superior rectal artery below Sudeck’s point during sigmoidectomy: report of a case. Surg Today. 1997; 27:254–256.8. Chandra S, Dutta U, Das R, Vaiphei K, Nagi B, Singh K. Mesenteric venous thrombosis causing jejunal stricture: secondary to hypercoagulable states and primary portal hypertension. Dig Dis Sci. 2002; 47:2017–2019.9. Narawane NM, Phadke AY, Shah SK, Bhandarkar PV, Abraham P. Jejunal stricture complicating acute mesenteric venous thrombosis secondary to protein C deficiency and factor V Leiden gene mutation. Indian J Gastroenterol. 2000; 19:79–80.10. Yang J, Shen L, Zheng X, Zhu Y, Liu Z. Small bowel stricture complicating superior mesenteric vein thrombosis. J Huazhong Univ Sci Technolog Med Sci. 2012; 32:146–148.11. Wittenberg J, Harisinghani MG, Jhaveri K, Varghese J, Mueller PR. Algorithmic approach to CT diagnosis of the abnormal bowel wall. Radiographics. 2002; 22:1093–1107.12. Steward MJ, Punwani S, Proctor I, Adjei-Gyamfi Y, Chatterjee F, Bloom S, et al. Non-perforating small bowel Crohn’s disease assessed by MRI enterography: derivation and histopathological validation of an MR-based activity index. Eur J Radiol. 2012; 81:2080–2088.13. Krajewski K, Siewert B, Eisenberg RL. Colonic dilation. AJR Am J Roentgenol. 2009; 193:W363–W372.14. Furukawa A, Kanasaki S, Kono N, Wakamiya M, Tanaka T, Takahashi M, et al. CT diagnosis of acute mesenteric ischemia from various causes. AJR Am J Roentgenol. 2009; 192:408–416.15. Haraguchi M, Matsushima S, Fujie Y, Sugimachi K. Ischemic stricture of the jejunum--report of a case. Jpn J Surg. 1990; 20:715–719.16. Eugène C, Valla D, Wesenfelder L, Fingerhut A, Bergue A, Merrer J, et al. Small intestinal stricture complicating superior mesenteric vein thrombosis. A study of three cases. Gut. 1995; 37:292–295.17. Simi M, Pietroletti R, Navarra L, Leardi S. Bowel stricture due to ischemic colitis: report of three cases requiring surgery. Hepatogastroenterology. 1995; 42:279–281.18. Hirota C, Iida M, Aoyagi K, Matsumoto T, Yao T, Fujishima M. Posttraumatic intestinal stenosis: clinical and radiographic features in four patients. Radiology. 1995; 194:813–815.19. Loberant N, Szvalb S, Herskovits M, Cohen I, Salamon V. Posttraumatic intestinal stenosis: radiographic and sonographic appearance. Eur Radiol. 1997; 7:524–526.20. De Backer AI, De Schepper AM, Vaneerdeweg W, Pelckmans P. Intestinal stenosis from mesenteric injury after blunt abdominal trauma. Eur Radiol. 1999; 9:1429–1431.21. Reinus JF, Brandt LJ, Boley SJ. Ischemic diseases of the bowel. Gastroenterol Clin North Am. 1990; 19:319–343.22. Zappa M, Stefanescu C, Cazals-Hatem D, Bretagnol F, Deschamps L, Attar A, et al. Which magnetic resonance imaging findings accurately evaluate inflammation in small bowel Crohn’s disease? A retrospective comparison with surgical pathologic analysis? Inflamm Bowel Dis. 2011; 17:984–999.23. Wibmer AG, Kroesen AJ, Gröne J, Buhr HJ, Ritz JP. Comparison of strictureplasty and endoscopic balloon dilatation for stricturing Crohn’s disease--review of the literature. Int J Colorectal Dis. 2010; 25:1149–1157.24. Schmitz-Moormann P, Pittner PM, Malchow H, Brandes JW. The granuloma in Crohn’s disease. A bioptical study. Pathol Res Pract. 1984; 178:467–476.25. Mazor Y, Karban A, Nesher S, Weiss B, Leshinsky-Silver E, Levine A, et al. Granulomas in Crohn’s disease: are newly discovered genetic variants involved? J Crohns Colitis. 2010; 4:438–443.26. Gore RM, Balthazar EJ, Ghahremani GG, Miller FH. CT features of ulcerative colitis and Crohn’s disease. AJR Am J Roentgenol. 1996; 167:3–15.27. Levi S, de Lacey G, Price AB, Gumpel MJ, Levi AJ, Bjarnason I. “Diaphragm-like” strictures of the small bowel in patients treated with non-steroidal anti-inflammatory drugs. Br J Radiol. 1990; 63:186–189.28. Perlemuter G, Guillevin L, Legman P, Weiss L, Couturier D, Chaussade S. Cryptogenetic multifocal ulcerous stenosing enteritis: an atypical type of vasculitis or a disease mimicking vasculitis. Gut. 2001; 48:333–338.29. Kohoutová D, Bures J, Tycová V, Bártová J, Tachecí I, Rejchrt S, et al. Severe cryptogenic multifocal ulcerous stenosing enteritis A report of three cases and review of the literature. Acta Medica (Hradec Kralove). 2010; 53:25–29.30. Barbagelatta M. [Anatomic-pathologic diagnosis of ischemic colitis]. J Chir (Paris). 1997; 134:97–102.