Clin Orthop Surg.
2018 Dec;10(4):508-512. 10.4055/cios.2018.10.4.508.
Unilateral Biportal Endoscopic Spinal Surgery Using a 30° Arthroscope for L5–S1 Foraminal Decompression
- Affiliations
-
- 1Department of Orthopedic Surgery, Andong Hospital, Andong, Korea.
- 2Department of Spine Surgery, Barun Hospital, Jinju, Korea. djchoi9@hanmail.net
- KMID: 2426538
- DOI: http://doi.org/10.4055/cios.2018.10.4.508
Abstract
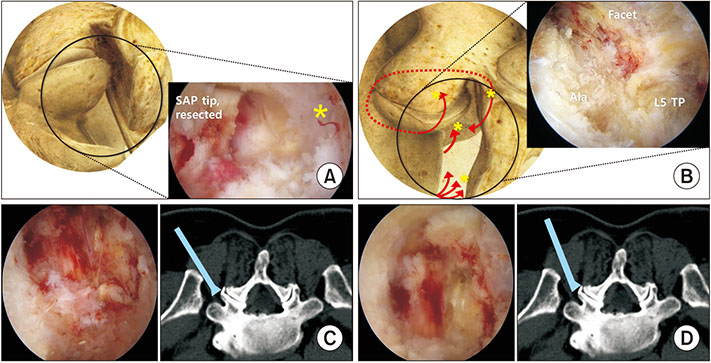
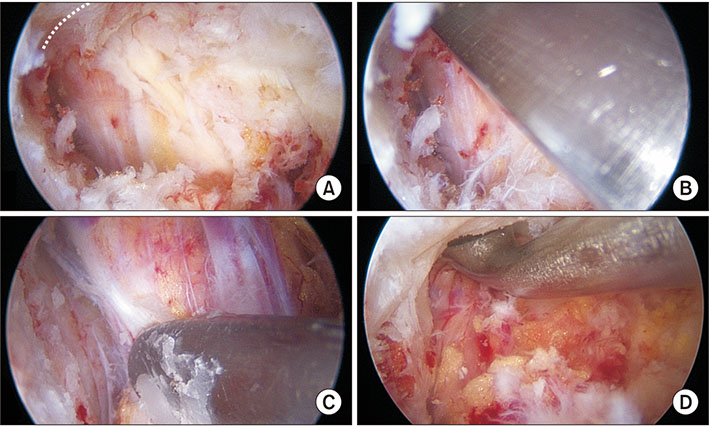
- Foraminal decompression using a minimally invasive technique to preserve facet joint stability and function without fusion reportedly improves the radicular symptoms in approximately 80% of patients and is considered one of the good surgical treatment choices for lumbar foraminal or extraforaminal stenosis. However, proper decompression was not possible because of the inability to access the foramen at the L5-S1 level due to prominence of the iliac crest. To overcome this challenge, endoscopy-based minimally invasive spine surgery has recently gained attention. Here, we report the technical skills required in unilateral extraforaminal biportal endoscopic spinal surgery using a 30° arthroscope to enable foraminal decompression at the L5-S1 level. Two 0.8-cm portals were created 2 cm lateral from the lateral border of the pedicles at the L5-S1 level. After sufficient working space was made, half of the superior articular process (SAP) in the hypertrophied facet joint was removed using a high-speed burr and a 5-mm wide osteotome, whereas the remaining inside part of the SAP was removed using a Kerrison punch and pituitary punch. The foraminal ligamentum flavum should be removed to inspect the conditions of the L5 exiting root and disc. Removing of the extruded disc could decompress the L5 root. The extraforaminal approach using a 30° arthroscope is considered a minimally invasive alternative technique for decompressing foraminal stenosis at the L5-S1 level that preserves facet stability and provides symptomatic relief.
Keyword
MeSH Terms
Figure
Reference
-
1. Ahn Y, Oh HK, Kim H, Lee SH, Lee HN. Percutaneous endoscopic lumbar foraminotomy: an advanced surgical technique and clinical outcomes. Neurosurgery. 2014; 75(2):124–133.2. Jenis LG, An HS. Spine update: lumbar foraminal stenosis. Spine (Phila Pa 1976). 2000; 25(3):389–394.3. Chang SB, Lee SH, Ahn Y, Kim JM. Risk factor for unsatisfactory outcome after lumbar foraminal and far lateral microdecompression. Spine (Phila Pa 1976). 2006; 31(10):1163–1167.
Article4. Kang K, Rodriguez-Olaverri JC, Schwab F, Hashem J, Razi A, Farcy JP. Partial facetectomy for lumbar foraminal stenosis. Adv Orthop. 2014; 2014:534658.
Article5. Wiltse LL, Spencer CW. New uses and refinements of the paraspinal approach to the lumbar spine. Spine (Phila Pa 1976). 1988; 13(6):696–706.
Article6. Choi DJ, Jung JT, Lee SJ, Kim YS, Jang HJ, Yoo B. Biportal endoscopic spinal surgery for recurrent lumbar disc herniations. Clin Orthop Surg. 2016; 8(3):325–329.
Article7. Cho SI, Chough CK, Choi SC, Chun JY. Microsurgical foraminotomy via Wiltse paraspinal approach for foraminal or extraforaminal stenosis at L5-S1 Level: risk factor analysis for poor outcome. J Korean Neurosurg Soc. 2016; 59(6):610–614.
Article8. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976). 2008; 33(9):931–939.
Article9. Yamada K, Matsuda H, Nabeta M, Habunaga H, Suzuki A, Nakamura H. Clinical outcomes of microscopic decompression for degenerative lumbar foraminal stenosis: a comparison between patients with and without degenerative lumbar scoliosis. Eur Spine J. 2011; 20(6):947–953.
Article10. Orita S, Inage K, Eguchi Y, et al. Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. Eur J Orthop Surg Traumatol. 2016; 26(7):685–693.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biportal endoscopic non-facetectomy foraminal decompression and discectomy (ligamentum flavum turn-down technique)
- Current Status of Biportal Endoscopic Decompression for Lumbar Foraminal Stenosis: Endoscopic Partial Facetectomy and Outcome Factors
- Unilateral Biportal Endoscopy for Decompression of Extraforaminal Stenosis at the Lumbosacral Junction: Surgical Techniques and Clinical Outcomes
- Biportal Endoscopic Spine Surgery for Various Foraminal Lesions at the Lumbosacral Lesion
- Management of a Rare Case of C2–3 Cervical Foraminal Disc Herniation by Unilateral Biportal Endoscopic Foraminotomy