J Korean Ophthalmol Soc.
2018 Nov;59(11):1091-1096. 10.3341/jkos.2018.59.11.1091.
Bilateral Delayed Nonarteritic Anterior Ischemic Neuropathy Following Acute Primary Angle-closure Crisis
- Affiliations
-
- 1Department of Ophthalmology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea. njmoon@cau.ac.kr
- KMID: 2426373
- DOI: http://doi.org/10.3341/jkos.2018.59.11.1091
Abstract
- PURPOSE
We report a case of bilateral nonarteritic anterior ischemic optic neuropathy (NAION) following acute angle-closure crisis (AACC).
CASE SUMMARY
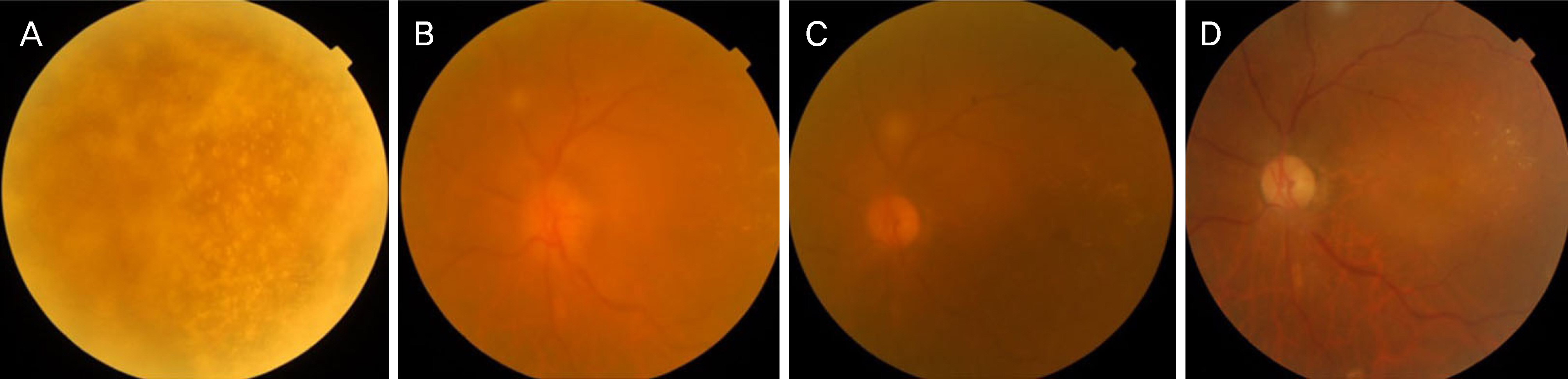
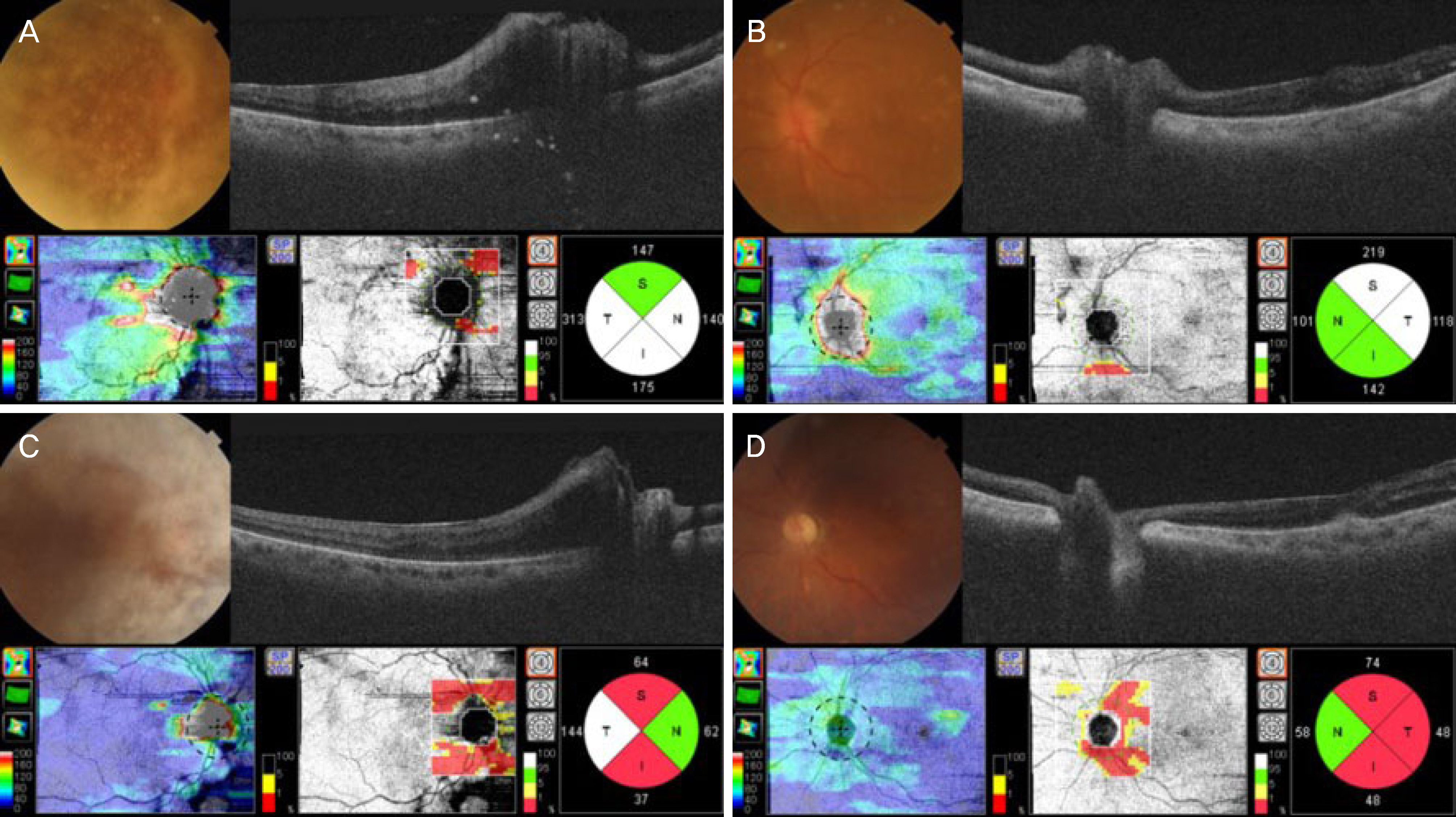
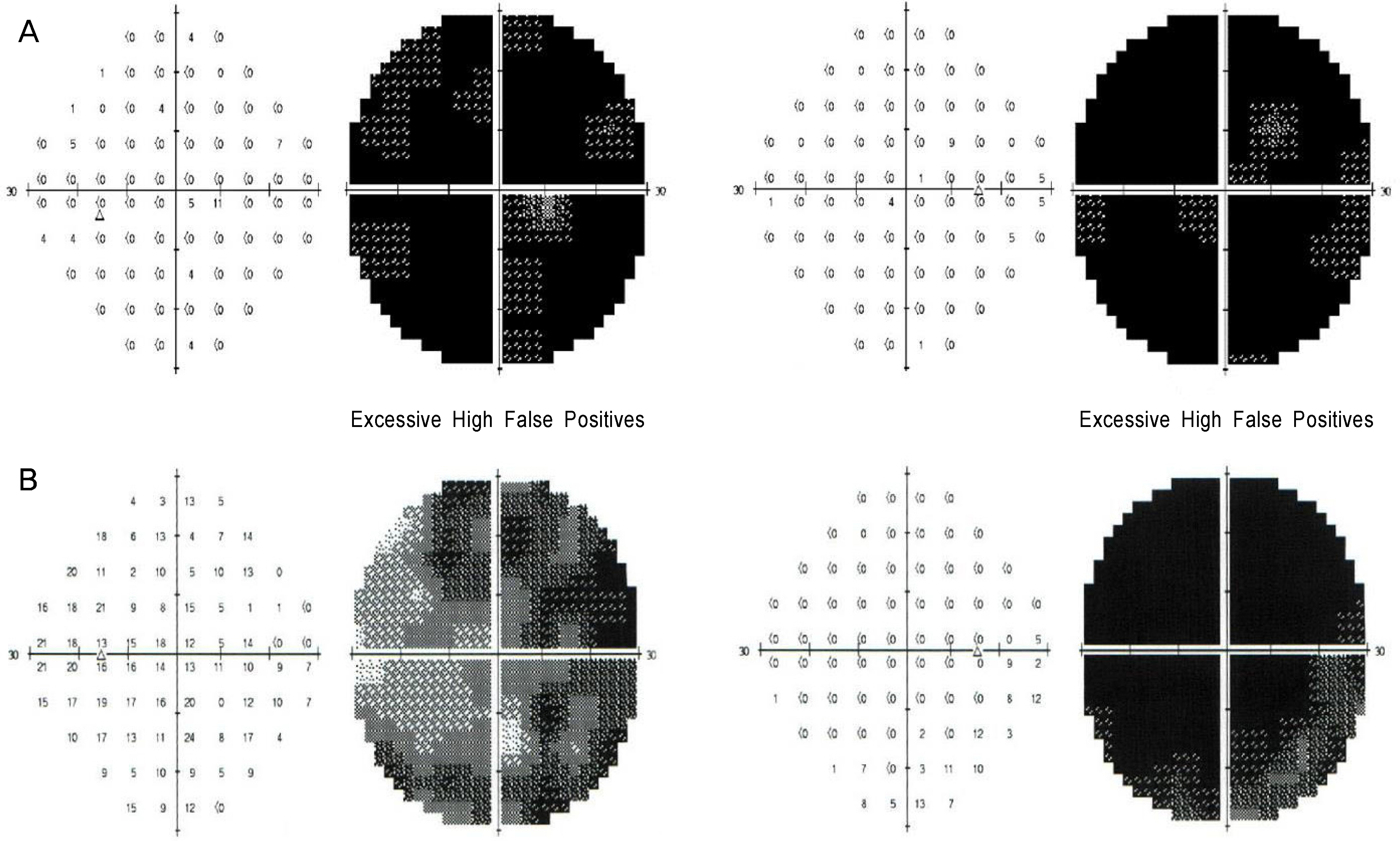
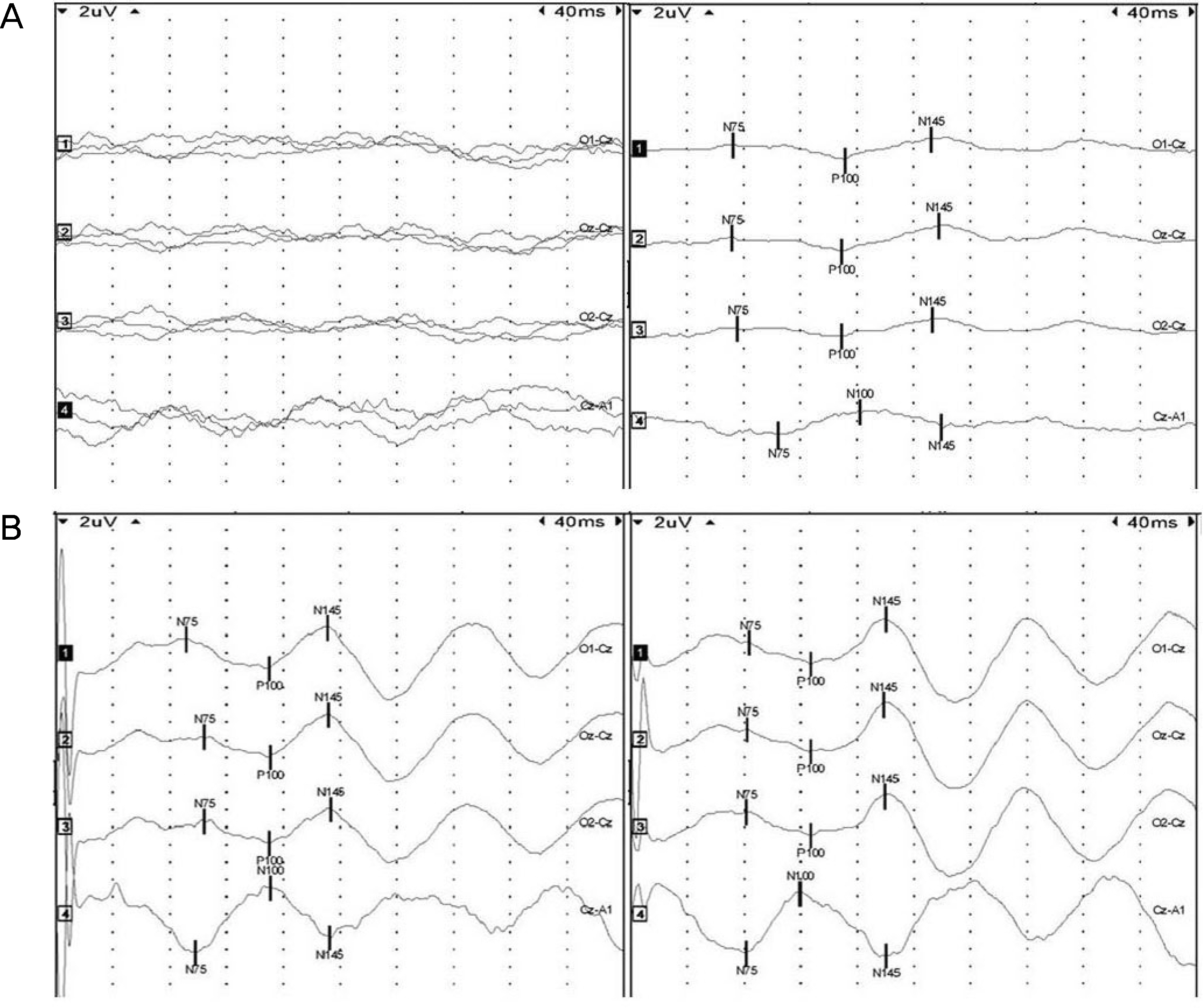
A 76-year-old female visited our clinic because of a 1-day history of ocular pain and vision loss in both eyes. The visual acuity was 0.02 in both eyes and her intraocular pressure (IOP) was 52 mmHg in the right eye (RE) and 50 mmHg in the left eye (LE). She had corneal edema and a shallow anterior chamber in both eyes, with 4 mm fixed dilated pupils. After decreasing the IOP with intravenous mannitol, laser iridotomy was performed. However, 2 days later, visual acuity was further reduced to finger counting at 10 cm RE and at 50 cm LE, and her optic disc was swollen. Bilateral NAION following AACC was diagnosed. One month later, visual acuity slightly improved to 0.02 RE and 0.04 LE, and the optic disc edema resolved. A small cup-disc ratio, optic disc pallor, and atrophy were observed. Humphrey visual fields demonstrated superior and inferior altitudial visual field defects in the LE, and almost total scotoma in the RE.
CONCLUSIONS
AACC can be a predisposing factor for NAION, so the relative afferent pupillary defect, papilledema, and presentation of other risk factors are important clues to a diagnosis of NAION.
MeSH Terms
Figure
Reference
-
References
1. Arnold AC. Pathogenesis of nonarteritic anterior ischemic optic neuropathy. J Neuroophthalmol. 2003; 23:157–63.
Article2. Sonty S, Schwartz B. Vascular accidents in acute angle closure glaucoma. Ophthalmology. 1981; 88:225–8.
Article3. Slavin ML, Margulis M. Anterior ischemic optic neuropathy abdominal acute angle– closure glaucoma. Arch Ophthalmol. 2001; 119:1215.4. Nahum Y, Newman H, Kurtz S, Rachmiel R. Nonarteritic anterior ischemic optic neuropathy in a patient with primary acute angle closureglaucoma. Can J Ophthalmol. 2008; 43:723–4.5. Choudhari NS, George R, Kankaria V, Sunil GT. Anterior ischemic optic neuropathy precipitated by acute primary– angle closure. Indian J Ophthalmol. 2010; 58:437–40.
Article6. Torricelli A, Reis AS, Abucham JZ, et al. Bilateral nonarteritic abdominal ischemic neuropathy following acute angle– closure abdominal in a patient with iridoschisis: case report. Arq Bras Oftalmol. 2011; 74:61–3.7. Kuriyan AE, Lam BL. Non– arteritic anterior ischemic optic abdominal secondary to acute primary– angle closure. Clin Ophthalmol. 2013; 7:1233–8.8. Kim R, Van Stavern G, Juzych M. Nonarteritic anterior ischemic optic neuropathy associated with acute glaucoma secondary to Posner– Schlossman syndrome. Arch Ophthalmol. 2003; 121:127–8.9. Irak I, Katz BJ, Zabriskie NA, Zimmerman PL. Posner– Schlossman syndrome and nonarteritic anterior ischemic optic neuropathy. J Neuroophthalmol. 2003; 23:264–7.10. Shin JH, Lee JW, Choi HY. A case of nonarteritic anterior ischemic optic neuropathy following acute angle– closure glaucoma. J Korean Ophthalmol Soc. 2011; 52:753–8.11. Kim KN, Kim CS, Lee SB, Lee YH. Delayed non– arteritic anterior ischemic optic neuropathy following acute primary angle closure. Korean J Ophthalmol. 2015; 29:209–11.12. Hayreh SS, Joos KM, Podhajsky PA, Long CR. Systemic diseases associated with nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol. 1994; 118:766–80.
Article13. Kim DH, Hwang JM. Risk factors for Korean patients with anterior ischemic optic neuropathy. J Korean Ophthalmol Soc. 2007; 48:1527–31.
Article14. Bayraktar Z, Alacali N, Bayraktar S. Diabetic papillopathy in type II diabetic patients. Retina. 2002; 22:752–8.
Article15. Kim JH, Kang SY, Kim NR, et al. Prevalence and characteristics of glaucoma among korean adults. Korean J Ophthalmol. 2011; 25:110–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nonarteritic Anterior Ischemic Optic Neuropathy Accompanying Appositional Angle-closure Glaucoma Mimicking Glaucomatocyclitic Crisis
- A Case of Nonarteritic Anterior Ischemic Optic Neuropathy Following Acute Angle-Closure Glaucoma
- Delayed Non-arteritic Anterior Ischemic Optic Neuropathy Following Acute Primary Angle Closure
- The Effect of an Intravitreal Triamcinolone Acetonide Injection for Acute Nonarteritic Anterior Ischemic Optic Neuropathy
- The Function of the Fellow Eye in Patients with Unilateral Nonarteritic Anterior Ischemic Optic Neuropathy