J Korean Ophthalmol Soc.
2010 May;51(5):784-789.
A Case of Tsutsugamushi Disease Associated With Intermediate Uveitis and Retinal Detachment
- Affiliations
-
- 1Department of Ophthalmology, Maryknoll Hospital, Busan, Korea. pjm1438@hanmail.net
Abstract
- PURPOSE
The authors report a Tsutsugamushi patient who has intermediate uveitis and rhegmatogenous retinal detachment without a typical skin eschar, which may be rare.
CASE SUMMARY
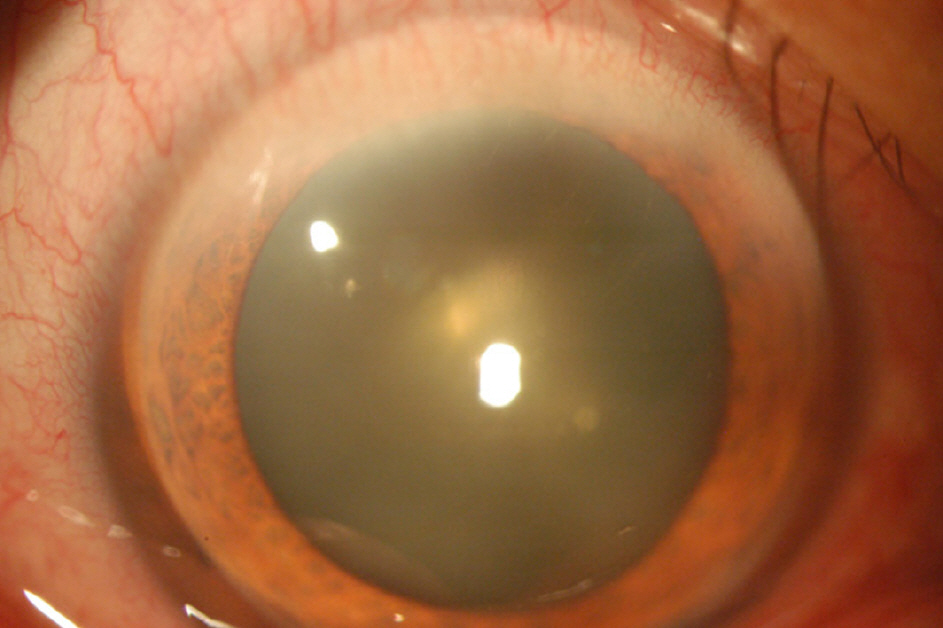
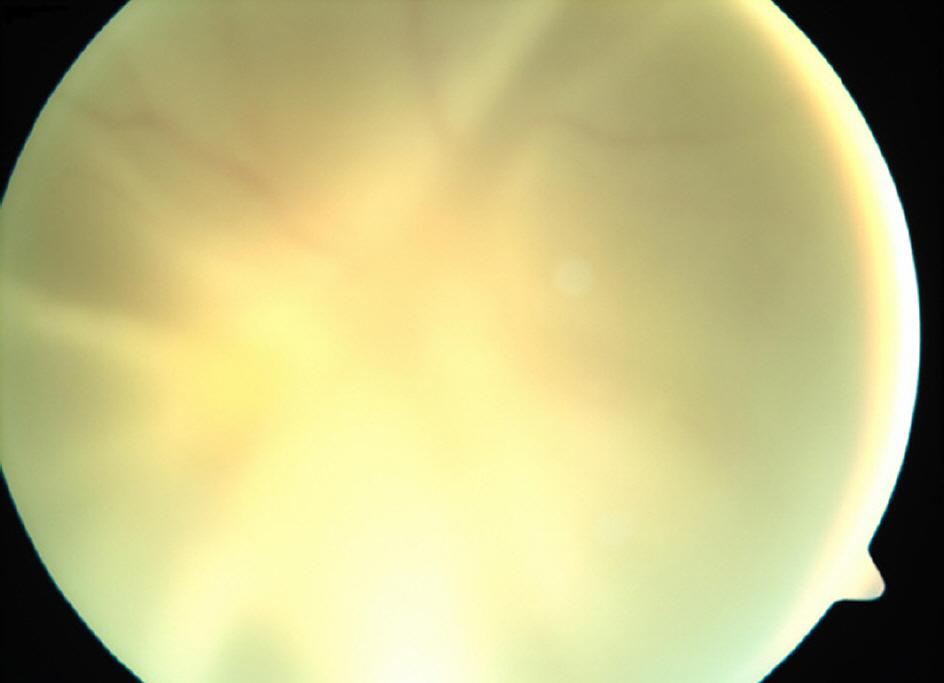
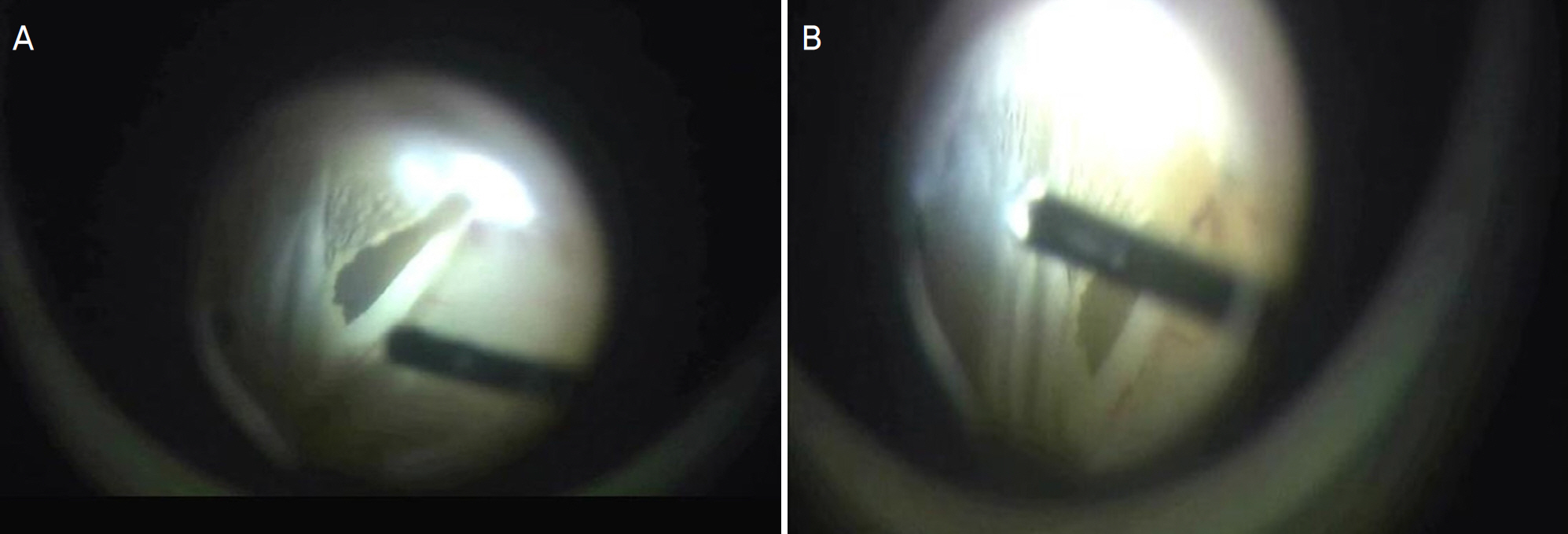
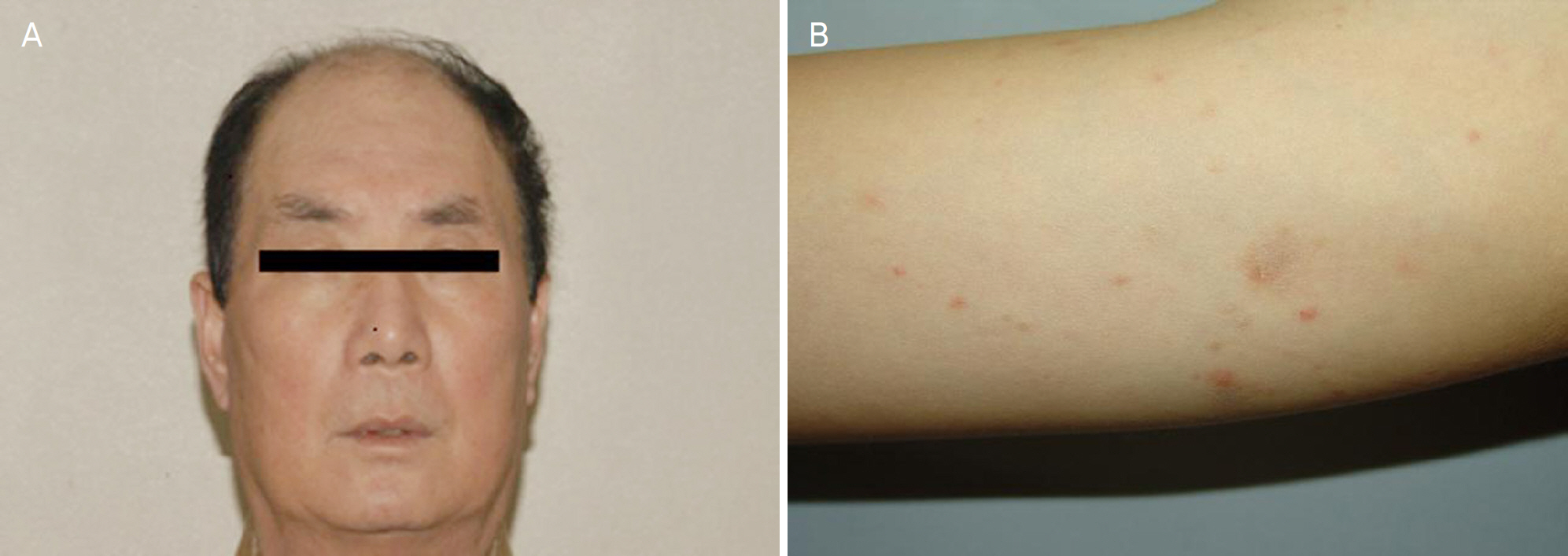
The authors present a case of a 63-year-old man who complained of fever, chills, and headache, with lymphadenopathy, hepatomegaly, reticulonodular pneumonia, and blurred vision in the right eye after descending a mountain in autumn. Serological findings showed elevated titers for strains of Rickettsia tsutsugamushi, even though no eschar could be found on his body. In addition, the ophthalmologic examination disclosed vitreous opacity as uveitis in his right eye; thus, the patient was treated for Tsutsugamushi disease. However, retinal detachment was found in his right eye even after treatment. Thus, a vitrectomy and intravitreal silicone oil injection was performed, and the patient's best corrected visual acuity improved from hand motion to 0.04 on the 7th day after the operation.
MeSH Terms
Figure
Reference
-
References
1. Brown GW. Recent studies of scrub typhus: A review. J Roy Soc Med. 1978; 71:507–10.2. Paul SR, Karanth S, Dickson C. Scrub typhus along the Thai-Kampuchean border: New treatment regimen. Trop Doct. 1987; 17:104–7.
Article3. Tachibana N. Tsutsugamushi disease. Jpn J Clin Med. 1985; 43:728–32.4. Yamasaku F. Tsutusgamushi disease. Handbook of internal medicine. 53B. Tokyo: Nakayama-Shoten;1979. p. 251–53.5. Chamberlain WP Jr. Ocular findings in scrub typhus. Arch Ophthalmol. 1952; 48:313–21.
Article6. Park JI, Han SH, Cho SC, et al. Outbreak of Hepatitis by orientia abdominal in the Early Years of the New Millenium. Korean J Hepatol. 2003; 9:198–204.7. Kuwabara Y. Iridocyclitis in tsutsugamushi disease. Jpn RevClin Opthalmol. 1919; 15:101–6.8. Yoneyama T, Ibaraki M. An insect bite lesion of the eyelid in abdominal disease. Jpn J Clin Ophthalmol. 1951; 5:752–53.9. Kim SY, Roh KH, Jung MS. Two cases of Tsutsugamushi Disease with Ocular Disease and Eschars on the Lower Eyelid. J Korean Ophthalmol. 2006; 47:1834–39.10. Fauchi AS. Harrison's principles of Internal Medicine. 17th ed.New York: The McGraw-Hill;2008. p. 1059–65.11. Scheie HG. Ocular changes associated with scrub typhus: a study of 451 patients. Arch Ophthalmol. 1948; 40:245–67.12. Kato T, Watanabe K, Katori M, et al. Conjunctival Injection, Episcleral Vessel Dilatation, and Subconjunctival Hemorrhage in abdominals with New Tsutsugamushi Disease. Jpn J Ophthalmol. 1997; 41:196–9.13. Allen Ac, Spitz S. A comparative study of pathology of scrub typhus and other rickettsial disease. Am J Pathol. 1945; 21:603–81.14. Seong SY, Choi MS, Kim IS. Orientia tsutsugamushi infection: abdominal and immune responses. Microbes infect. 2001; 3:11–21.15. Cho NH, Seong SY, Choi MS, Kim IS. Expression of chemokine gene in human dermal microvascular endothelial cell lines infected with Orientia tsutsugamushi. Infect Immun. 2001; 69:1265–72.16. Kim MK, Kee SH, Cho KA, et al. Apotosis of endothelial cell line ECV304 persistently infected with Orientia tsutsugamushi. Microbiol Immunol. 1999; 43:751–7.17. Yotsukura M, Aoki N, Fukuzumi N, Ishikawa K. Review of a case of a case of tsutsugamushi disease showing myocarditis and confirmation of Rickettsia by endocardial biopsy. Jpn Circ J. 1991; 55:149–53.18. Pongponratn E, Maneerat Y, Chaisri U, et al. Electronmicroscopic abdominal of Rickettsia tsutsugamushi infected human liver. Trop Med Int Health. 1998; 3:242–8.19. Scheie HG. Ocular changes associated with scrub typhus: A study of 451 patients. Arch Ophthalmol. 1948; 40:245–67.20. Henderly DE, Haymond RS, Rso NA, Smith RE. The significance of the pars plana exudates in pars planitis. Am J Ophthalmol. 1987; 103:669–71.21. Breeveld J, Rothova A, Kuiper H. Intermediate uveitis and Lyme bor-reliosis. Br J Ophthalmol. 1992; 76:181–2.
Article22. Ormerod LD, Dailey JP. Ocular manifestations of cat-scratch disease. Curr Opin Ophthalmol. 1999; 10:209–16.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Results of Pars Plana Vitrectomy in Intermediate Uveitis
- Clineal Analysis of Peripheral Uveitis
- Clinical Analysis for Complications of Nd-YAG Laser Posterior Capsulotomy in Uveitis Patients
- Secondary Giant Retinal Cyst
- A Case of Post. Scleritis Associated with Ciliochoroidal Detachment and Ant. Uveitis in Background Diabetic Retinopathy Patient