J Korean Ophthalmol Soc.
2010 May;51(5):751-757.
Dacryocystocele in Adult: A Report of Five Cases
- Affiliations
-
- 1Department of Ophthalmology, Hanyang University College of Medicine, Guri, Korea. lyjot@hanyang.ac.kr
Abstract
- PURPOSE
To report the clinical findings and the treatments of patients with dacryocystocele, presenting as an uncommon mass in the medial canthal area of adults.
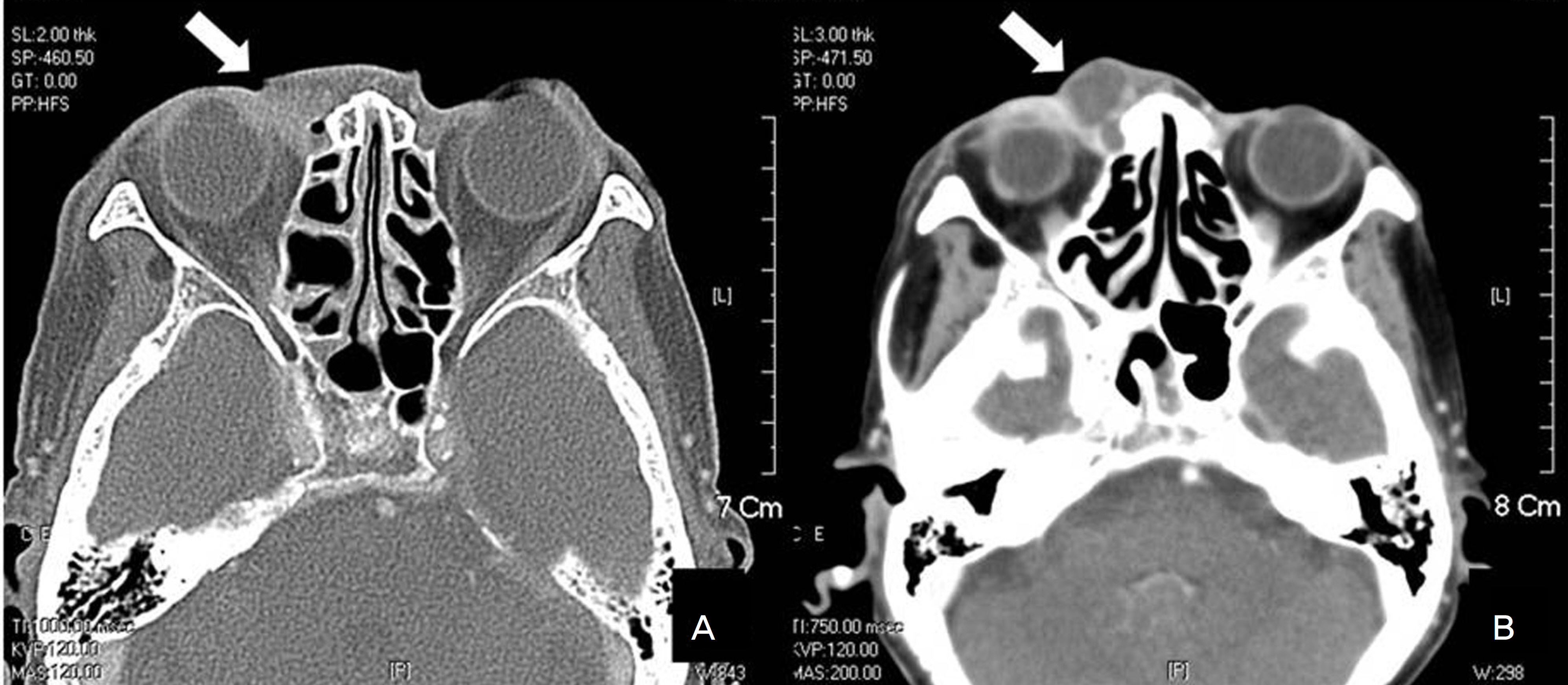
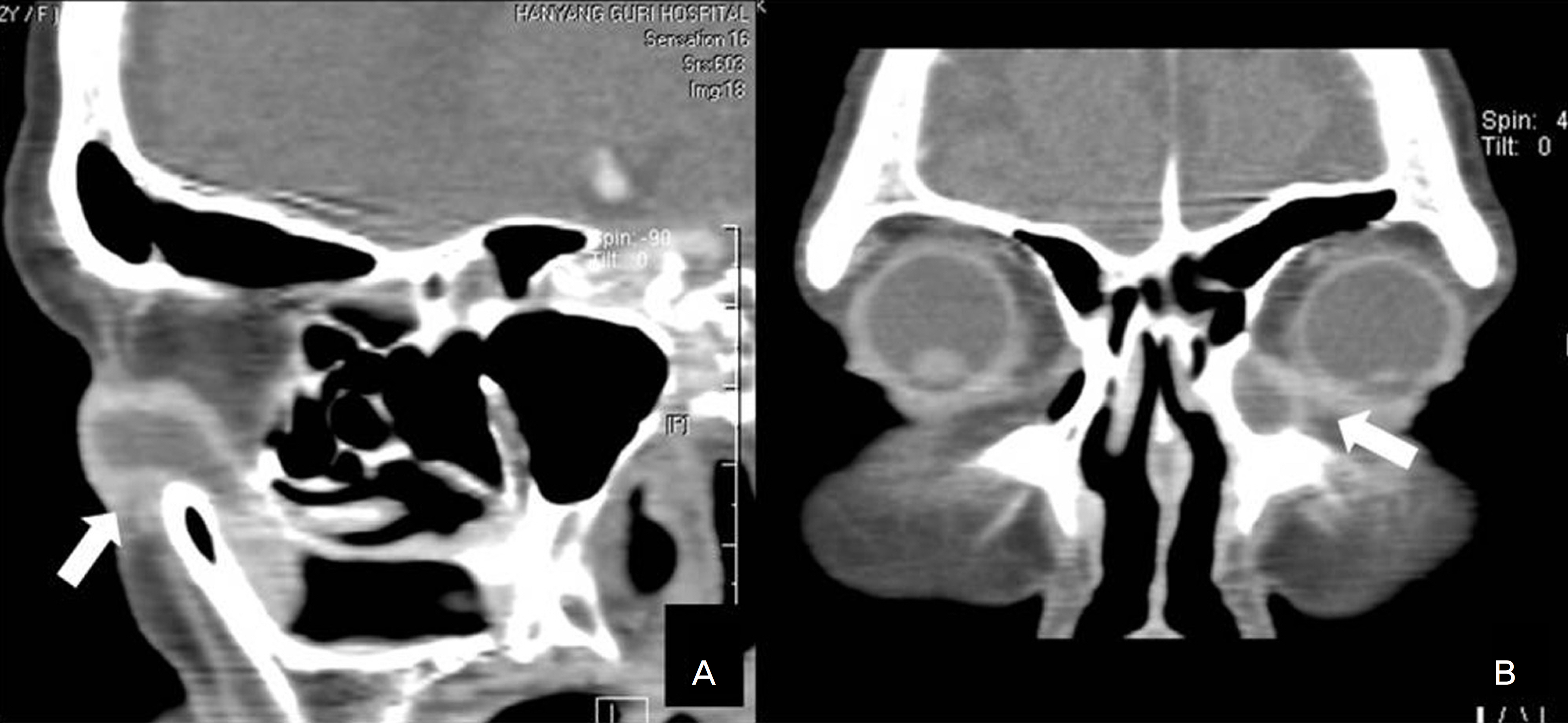
CASE SUMMARY
Five patients, diagnosed with dacryocystocele, complained of epiphora and mucopurulent discharge and were found to have a medial canthal mass. Four of these patients presented with symptoms of acute dacryocystitis. One patient underwent repeated endonasal dacryocystorhinostomy (endonasal DCR) with silicone implantation, but the epiphora returned a few months after the treatment. The patient then received external dacryocystorhinostomy (external DCR) with silicone implantation. Two patients experienced recurrence after the first endonasal DCR and, therefore, received repeat endonasal DCR with silicone implantation via a maximum excision of the enlarged lacrimal sac. One patient underwent external DCR with silicone implantation due to acute inflammation with chronic dacryocystitis, and one attempted conservative treatment after refusing any surgical procedure but suffered a relapse. In the surgical cases, no patients experienced recurrence after the final procedure, and they all had a favorable course during the 6 to 14 months of follow-up.
CONCLUSIONS
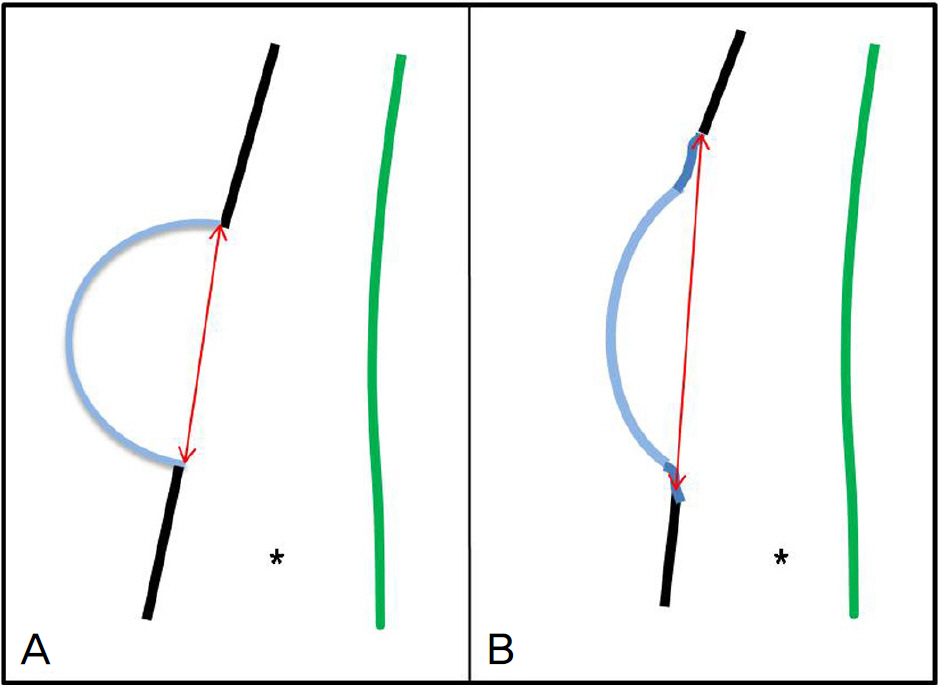
Dacryocystocele in adults always requires a surgical procedure. Additional maximum excision of the lateral wall of an enlarged lacrimal sac could be performed to reduce the possibility of recurrence.
MeSH Terms
Figure
Reference
-
References
1. Moon JH, Kim YD. A case of bilateral dacryocystocele with absence of the lacrimal puncta. J Korean Ophthalmol Soc. 1990; 31:81–5.2. Lai PC, Wang JK, Liao SL. A case of dacryocystocele in an adult. Jpn J Ophthalmol. 2004; 48:418–26.
Article3. Bhaya MH, Meehan R, Har-El G. Dacryocystocele in an adult: abdominal management. Am J Otolaryngol. 1997; 18:131–4.4. Jones LT, Wobig JL. Surgery of the Eyelids and Lacrimal system. 1st ed.Birmingham, AL: Aesculapius Publishing Co;1976. p. 162–7.5. Weinstein GS, Biglan AW, Patterson JH. Congenital lacrimal sac mucoceles. Am J Ophthalmol. 1982; 94:106–10.
Article6. Woo KI, Kim YD. Four cases of dacryocystocele. Korean J Ophthalmol. 1997; 11:65–9.
Article7. Hornblass A, Hanig CJ. Lacrimal inflammations and infections, Oculoplastic, orbital, and Reconstructive Surgery. Dryden RM, Wulc AE, editors. Orbit and Lacrimal System. 2nd ed.Baltimore Williams and Wilkins;1990. p. 1418–9.8. Cavazza S, Laffi GL, Lodi L, et al. Congenital dacryocystocele: abdominal and treatment. Acta Otorhinolaryngol Ital. 2008; 28:298–301.9. Debnam JM, Esmaeli B, Ginsberg LE. Imaging characteristics of abdominal diagnosed after surgery for sinonasal cancer. AJNR Am J Neuroradiol. 2007; 28:1872–5.10. Shashy RG, Durairaj V, Holmes JM, et al. Congenital dacryocystocele associated with intranasal cysts: diagnosis and management. Laryngoscope. 2003; 113:37–40.
Article11. Rand PK, Ball WS, Kulwin DR. Congenital nasolacrimal mucoceles: CT evaluation. Radiology. 1989; 173:691–4.
Article12. Becker BB. The treatment of congenital dacryocystocele. Am J Ophthalmol. 2006; 142:835–8.
Article13. Herbert HM, Rose GE. Air reflux after external dacryocystorhinostomy. Arch Ophthalmol. 2007; 125:1674–6.
Article14. Yazici B, Yazici Z. Anatomic position of the common canaliculus in patients with a large lacrimal sac. Ophthal Plast Reconstr Surg. 2008; 24:90–3.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Endoscopic Management of Dacryocystocele in an Adult
- Two Cases of Nasolacrimal Duct Cyst Developed in Neonate
- Four cases of dacryocystocele
- A Case of Congenital Dacryocystocele
- Successful Treatment of Dacryocystocele due to Secondary Nasolacrimal Duct Obstruction by Intraosseous Cavernous Hemangioma