J Periodontal Implant Sci.
2018 Oct;48(5):274-283. 10.5051/jpis.2018.48.5.274.
Early Wound Healing Score: a system to evaluate the early healing of periodontal soft tissue wounds
- Affiliations
-
- 1Section of Periodontics, Department of Oral and Maxillofacial Sciences, Sapienza University of Rome, Rome, Italy. dr.lorenzomarini@gmail.com
- 2Clinic of Preventive Dentistry, Periodontology and Cariology, Center of Dental Medicine, University of Zurich, Zurich, Switzerland.
- KMID: 2424861
- DOI: http://doi.org/10.5051/jpis.2018.48.5.274
Abstract
- PURPOSE
Numerous indices have been proposed to analyse wound healing in oral soft tissues, but each has specific shortcomings. A new method of analysis, the Early Wound Healing Score (EHS), was evaluated in the present study. The aim was to assess more accurately early healing by primary intention of surgical incisions in periodontal soft tissues.
METHODS
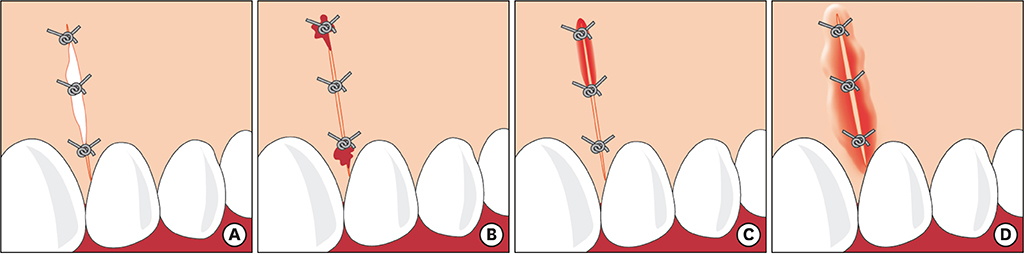
Twenty-one patients were treated with different surgical procedures comprising 1 or 2 vertical releasing incisions as part of a surgical access flap. Twenty-four hours after surgery, early wound healing at the vertical releasing incisions was assessed using the EHS. This score assessed clinical signs of re-epithelialization (CSR), clinical signs of haemostasis (CSH), and clinical signs of inflammation (CSI). Since complete wound epithelialization was the main outcome, the CSR score was weighted to be 60% of the total final score. Accordingly, a score of 0, 3, or 6 points was possible for the assessment of CSR, whereas scores of 0, 1, or 2 points were possible for CSH and CSI. Higher values indicated better healing. Accordingly, the score for ideal early wound healing was 10.
RESULTS
Thirty vertical releasing incisions were assessed in 21 patients. At 24 hours after incision, 16 vertical releasing incisions (53.33%) received the maximum score of CSR, while 6 cases (20%) received an EHS of 10. None of the cases received 0 points.
CONCLUSION
The EHS system may be a useful tool for assessing early wound healing in periodontal soft tissue by primary intention after surgery.
MeSH Terms
Figure
Reference
-
1. American Academy of Periodontology. Glossary of periodontal terms. 4th ed. Chicago (IL): American Academy of Periodontology;2001.2. Wikesjö UM, Selvig KA. Periodontal wound healing and regeneration. Periodontol 2000. 1999; 19:21–39.
Article3. Aukhil I. Biology of wound healing. Periodontol 2000. 2000; 22:44–50.
Article4. Häkkinen L, Uitto VJ, Larjava H. Cell biology of gingival wound healing. Periodontol 2000. 2000; 24:127–152.
Article5. Polimeni G, Xiropaidis AV, Wikesjö UM. Biology and principles of periodontal wound healing/regeneration. Periodontol 2000. 2006; 41:30–47.
Article6. Hiatt WH, Stallard RE, Butler ED, Badgett B. Repair following mucoperiosteal flap surgery with full gingival retention. J Periodontol. 1968; 39:11–16.
Article7. Werfully S, Areibi G, Toner M, Bergquist J, Walker J, Renvert S, et al. Tensile strength, histological and immunohistochemical observations of periodontal wound healing in the dog. J Periodontal Res. 2002; 37:366–374.
Article8. Susin C, Fiorini T, Lee J, De Stefano JA, Dickinson DP, Wikesjö UM. Wound healing following surgical and regenerative periodontal therapy. Periodontol 2000. 2015; 68:83–98.
Article9. Landry RG, Turnbull RS, Howley T. Effectiveness of benzydamyne HCl in the treatment of periodontal post-surgical patients. Res Clin Forums. 1988; 10:105–118.10. Wachtel H, Schenk G, Böhm S, Weng D, Zuhr O, Hürzeler MB. Microsurgical access flap and enamel matrix derivative for the treatment of periodontal intrabony defects: a controlled clinical study. J Clin Periodontol. 2003; 30:496–504.
Article11. Hagenaars S, Louwerse PH, Timmerman MF, Van der Velden U, Van der Weijden GA. Soft-tissue wound healing following periodontal surgery and Emdogain application. J Clin Periodontol. 2004; 31:850–856.
Article12. Tonetti MS, Fourmousis I, Suvan J, Cortellini P, Brägger U, Lang NP, et al. Healing, post-operative morbidity and patient perception of outcomes following regenerative therapy of deep intrabony defects. J Clin Periodontol. 2004; 31:1092–1098.
Article13. Huang LH, Neiva RE, Wang HL. Factors affecting the outcomes of coronally advanced flap root coverage procedure. J Periodontol. 2005; 76:1729–1734.
Article14. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013; 310:2191–2194.15. Woodley DT. Reepithelialization. In : Clark RAF, editor. The molecular and cellular biology of wound repair. New York (NY): Plenum Press;1996. p. 339–354.16. Gale AJ. Continuing education course #2: current understanding of hemostasis. Toxicol Pathol. 2011; 39:273–280.
Article17. Politis C, Schoenaers J, Jacobs R, Agbaje JO. Wound healing problems in the mouth. Front Physiol. 2016; 7:507.
Article18. Larjava H. Oral wound healing: cell biology and clinical management. Chichester: John Wiley & Sons, Inc.;2012.19. Harrison JW. Healing of surgical wounds in oral mucoperiosteal tissues. J Endod. 1991; 17:401–408.
Article20. Kumar KR, Kumar J, Sarvagna J, Gadde P, Chikkaboriah S. Hemostasis and post-operative care of oral surgical wounds by hemcon dental dressing in patients on oral anticoagulant therapy: a split mouth randomized controlled clinical trial. J Clin Diagn Res. 2016; 10:ZC37–ZC40.
Article21. Martin P, Leibovich SJ. Inflammatory cells during wound repair: the good, the bad and the ugly. Trends Cell Biol. 2005; 15:599–607.
Article22. Young EE, Lariviere WR, Belfer I. Genetic basis of pain variability: recent advances. J Med Genet. 2012; 49:1–9.
Article23. Pippi R. Post-surgical clinical monitoring of soft tissue wound healing in periodontal and implant surgery. Int J Med Sci. 2017; 14:721–728.
Article24. Cairo F, Rotundo R, Miller PD Jr, Pini Prato GP. Root coverage esthetic score: a system to evaluate the esthetic outcome of the treatment of gingival recession through evaluation of clinical cases. J Periodontol. 2009; 80:705–710.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Homologous fibronectin enhances healing of excised wounds in rats
- The Clinical Uses of Collagen-Based Matrices in the Treatment of Chronic Wounds
- Cell Therapy for Wound Healing
- Gene therapy of scarring: a lesson learned from fetal scarless wound healing
- Control of Scarring in Adult Wounds using Antisense Connective Tissue Growth Factor Ollgodeoxynucleotides