Hip Pelvis.
2017 Dec;29(4):240-246. 10.5371/hp.2017.29.4.240.
Perioperative Comparison of Hip Arthroplasty Using the Direct Anterior Approach with the Posterolateral Approach
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chosun University School of Medicine, Gwangju, Korea. jo.suenghwan@chosun.ac.kr
- KMID: 2424250
- DOI: http://doi.org/10.5371/hp.2017.29.4.240
Abstract
- PURPOSE
The aim of the current study is to report the advantage and disadvantage of total hip arthroplasty performed in direct anterior approach (DAA) by comparing it to the posterolateral approach (PLA).
MATERIALS AND METHODS
Twenty-five hip arthroplasty done in DAA (12 total hip arthroplasty [THA] and 13 bipolar hemiarthroplasty [BHA]) were compared with the same number done in PLA (13 THA and 12 BHA). Intraoperative assessments including operation time, anesthetic time, bleeding amount were recorded with intraoperative complications. Immediate postoperatively, position of the prosthesis and leg length discrepancy were measured and were compared between the two approaches.
RESULTS
The operation time was 22 minutes and 19 minutes longer in DAA for THA and BHA respectively while the anesthetic time difference was 26 and 10 respectively. However, these parameters showed no statistical difference. No significance was found when bleeding amount was compared. For DAA, cup alignment was within safe zone in 100% both for inclination and for anteversion while this was 83.3% and 75.0% respectively in PLA. Leg length difference was 3 mm in DAA and 5 mm in PLA but had no significant difference. Tensor fascia lata tear was the most common complication occurring in 9 patients.
CONCLUSION
Although significant was not reached there was trend toward more operation time and anesthetic time when DAA was used. However, the trend also showed that cup and stem were likely to be in more accurate position and in adequate size which is likely due to the accurate use of fluoroscopy.
Keyword
MeSH Terms
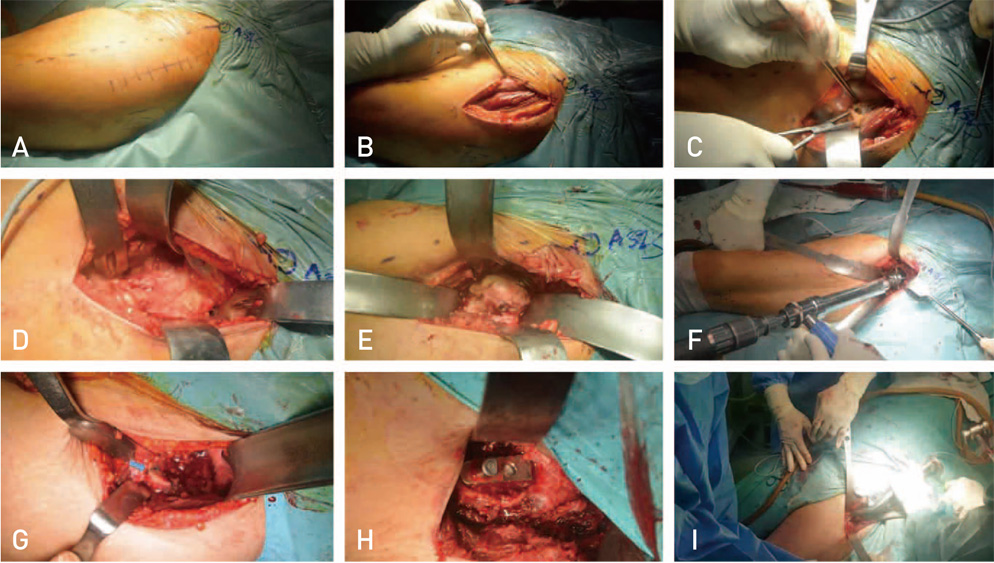
Figure
Reference
-
1. Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 2001; 87:62–72.
Article2. Eckel R, Ros R, Decker B, Mattay J, Anselmetti D. Supramolecular chemistry at the single-molecule level. Angew Chem Int Ed Engl. 2005; 44:484–488.
Article3. Mayr E, Nogler M, Benedetti MG, et al. A prospective randomized assessment of earlier functional recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech (Bristol, Avon). 2009; 24:812–818.
Article4. Meermans G, Konan S, Das R, Volpin A, Haddad FS. The direct anterior approach in total hip arthroplasty: a systematic review of the literature. Bone Joint J. 2017; 99-B:732–740.5. Connolly KP, Kamath AF. Direct anterior total hip arthroplasty: Comparative outcomes and contemporary results. World J Orthop. 2016; 7:94–101.
Article6. Matta JM, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005; 441:115–124.
Article7. Pradhan R. Planar anteversion of the acetabular cup as determined from plain anteroposterior radiographs. J Bone Joint Surg Br. 1999; 81:431–435.
Article8. Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982; 64:1295–1306.
Article9. Chang RW, Pellisier JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996; 275:858–865.
Article10. Sutherland R, Rowe MJ Jr. Simplified surgical approach to the hip. Arch Surg. 1944; 48:144–145.
Article11. Higgins BT, Barlow DR, Heagerty NE, Lin TJ. Anterior vs. posterior approach for total hip arthroplasty, a systematic review and meta-analysis. J Arthroplasty. 2015; 30:419–434.
Article12. Alecci V, Valente M, Crucil M, Minerva M, Pellegrino CM, Sabbadini DD. Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings. J Orthop Traumatol. 2011; 12:123–129.
Article13. Barrett WP, Turner SE, Leopold JP. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty. 2013; 28:1634–1638.
Article14. Berend KR, Lombardi AV Jr, Seng BE, Adams JB. Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty. J Bone Joint Surg Am. 2009; 91:Suppl 6. 107–120.
Article15. Goebel S, Steinert AF, Schillinger J, et al. Reduced postoperative pain in total hip arthroplasty after minimal-invasive anterior approach. Int Orthop. 2012; 36:491–498.
Article16. Zawadsky MW, Paulus MC, Murray PJ, Johansen MA. Early outcome comparison between the direct anterior approach and the mini-incision posterior approach for primary total hip arthroplasty: 150 consecutive cases. J Arthroplasty. 2014; 29:1256–1260.
Article17. Poehling-Monaghan KL, Kamath AF, Taunton MJ, Pagnano MW. Direct anterior versus miniposterior THA with the same advanced perioperative protocols: surprising early clinical results. Clin Orthop Relat Res. 2015; 473:623–631.
Article18. D'Arrigo C, Speranza A, Monaco E, Carcangiu A, Ferretti A. Learning curve in tissue sparing total hip replacement: comparison between different approaches. J Orthop Traumatol. 2009; 10:47–54.19. Rodriguez JA, Deshmukh AJ, Rathod PA, et al. Does the direct anterior approach in THA offer faster rehabilitation and comparable safety to the posterior approach? Clin Orthop Relat Res. 2014; 472:455–463.
Article20. Martin CT, Pugely AJ, Gao Y, Clark CR. A comparison of hospital length of stay and short-term morbidity between the anterior and the posterior approaches to total hip arthroplasty. J Arthroplasty. 2013; 28:849–854.
Article21. Spaans AJ, van den Hout JA, Bolder SB. High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop. 2012; 83:342–346.
Article22. de Steiger RN, Lorimer M, Solomon M. What is the learning curve for the anterior approach for total hip arthroplasty? Clin Orthop Relat Res. 2015; 473:3860–3866.
Article23. Barton C, Kim PR. Complications of the direct anterior approach for total hip arthroplasty. Orthop Clin North Am. 2009; 40:371–375.
Article24. Rathod PA, Bhalla S, Deshmukh AJ, Rodriguez JA. Does fluoroscopy with anterior hip arthroplasty decrease acetabular cup variability compared with a nonguided posterior approach? Clin Orthop Relat Res. 2014; 472:1877–1885.
Article25. Abe H, Sakai T, Takao M, Nishii T, Nakamura N, Sugano N. Difference in stem alignment between the direct anterior approach and the posterolateral approach in total hip arthroplasty. J Arthroplasty. 2015; 30:1761–1766.
Article26. Mohan R, Yi PH, Hansen EN. Evaluating online information regarding the direct anterior approach for total hip arthroplasty. J Arthroplasty. 2015; 30:803–807.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Approaches in Hip Surgery
- Modified Posterior Approach to Total Hip Arthroplasty
- Patient-Reported Outcome Measures of Staged Direct Anterior Approach and Direct Lateral Approach for Total Hip Arthroplasty Performed on the Same Patient
- Posterior Approach to Total Hip Joint Replacement Arthroplasty
- Surgical Approach to the Hip: Direct Lateral Approach