Korean J Ophthalmol.
2018 Oct;32(5):382-390. 10.3341/kjo.2017.0129.
Effects of Choroidal Thickness on Refractive Outcome Following Cataract Surgery in Primary Angle Closure
- Affiliations
-
- 1Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sungeye@gmail.com
- KMID: 2422068
- DOI: http://doi.org/10.3341/kjo.2017.0129
Abstract
- PURPOSE
To identify the preoperative biometric factors, including subfoveal choroidal thickness (CT), associated with refractive outcome after cataract surgery in eyes with primary angle closure (PAC).
METHODS
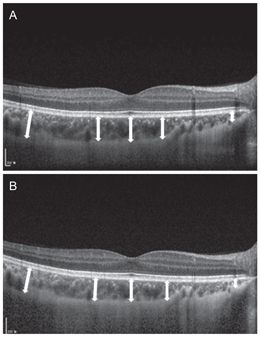
This study included 50 eyes of 50 PAC patients who underwent uneventful cataract surgery. Preoperatively, anterior segment parameters including anterior chamber depth (ACD) and lens vault were determined by anterior segment optical coherence tomography. Subfoveal CT was measured by spectral domain optical coherence tomography enhanced depth imaging before and at one month after surgery. Mean refractive error (MRE) was calculated as the difference in spherical equivalent between actual postoperative refraction determined one month postoperatively and that predicted using each of three IOL calculation formulas (SRK/II, SRK/T, and Haigis). Regression analyses were performed to investigate potential associations between MRE and putative factors.
RESULTS
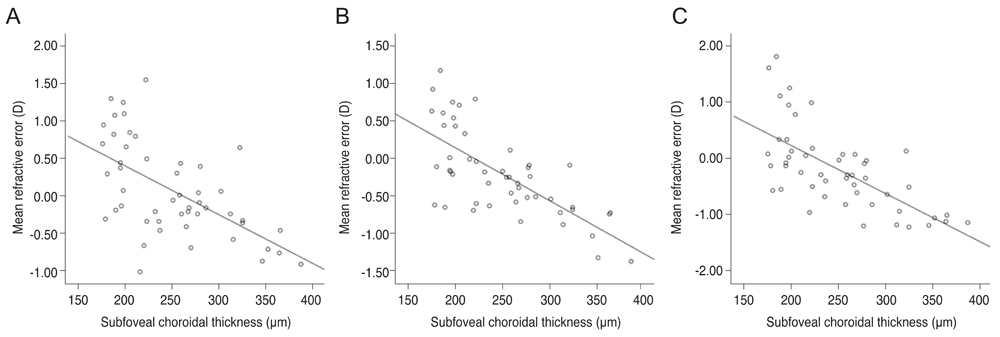
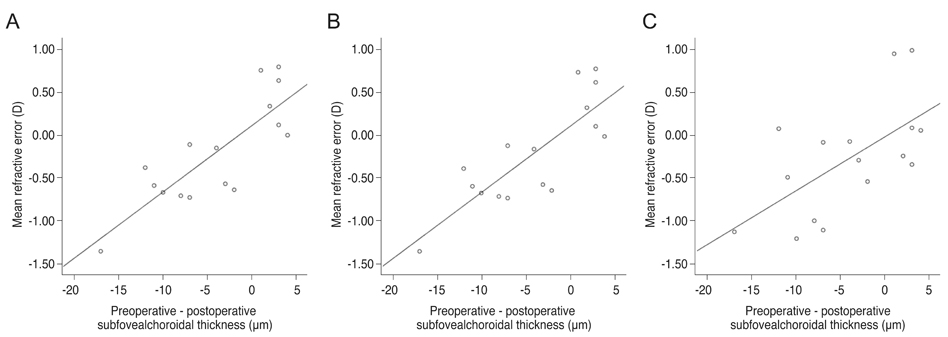
Mean ACD was 1.9 ± 0.4 mm, and preoperative subfoveal CT was 250.8 ± 56.9 µm. The SRK/T (MRE, 0.199 ± 0.567 diopters [D]) and Haigis (MRE, 0.190 ± 0.727 D) formulas showed slight hyperopic shift, while the SRK/II formula demonstrated a myopic shift (MRE, −0.077 ± 0.623 D) compared with that expected after cataract surgery. Mean absolute refractive error was not significantly different between formulas. Higher preoperative lens vault and shallower ACD were associated with a hyperopic shift in all formulas, but not in a statistically significant manner. Thicker preoperative subfoveal choroid was associated with a myopic shift after cataract surgery in all formulas (SRK/II: β = −0.511, p < 0.001; SRK/T: β = −0.652, p < 0.001; Haigis: β = −0.671, p < 0.001). Greater postoperative reduction of subfoveal CT was associated with a myopic shift after cataract surgery in all formulas (SRK/II: β = −0.511, p < 0.001; SRK/T: β = −0.652, p < 0.001; Haigis: β = −0.671, p < 0.001).
CONCLUSIONS
Our results indicate that preoperative subfoveal CT and the difference between pre- and postoperative subfoveal CT are significant factors for predicting refractive error after cataract surgery in PAC patients. These findings should be considered when performing cataract surgery to optimize visual outcomes.
Figure
Reference
-
1. Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006; 90:262–267.
Article2. Robin AL, Pollack IP. Argon laser peripheral iridotomies in the treatment of primary angle closure glaucoma. Long-term follow-up. Arch Ophthalmol. 1982; 100:919–923.3. Lam DS, Tham CC, Lai JS, Leung DY. Current approaches to the management of acute primary angle closure. Curr Opin Ophthalmol. 2007; 18:146–151.
Article4. Lai JS, Tham CC, Chan JC. The clinical outcomes of cataract extraction by phacoemulsification in eyes with primary angle-closure glaucoma (PACG) and co-existing cataract: a prospective case series. J Glaucoma. 2006; 15:47–52.
Article5. Shrivastava A, Singh K. The effect of cataract extraction on intraocular pressure. Curr Opin Ophthalmol. 2010; 21:118–122.
Article6. Azuara-Blanco A, Burr J, Ramsay C, et al. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): a randomised controlled trial. Lancet. 2016; 388:1389–1397.
Article7. Joo J, Whang WJ, Oh TH, et al. Accuracy of intraocular lens power calculation formulas in primary angle closure glaucoma. Korean J Ophthalmol. 2011; 25:375–379.
Article8. Lee HS, Park JW, Park SW. Factors affecting refractive outcome after cataract surgery in patients with a history of acute primary angle closure. Jpn J Ophthalmol. 2014; 58:33–39.
Article9. Kim YK, Yoo BW, Kim HC, et al. Relative lens vault in subjects with angle closure. BMC Ophthalmol. 2014; 14:93.
Article10. Seo S, Lee CE, Kim YK, et al. Factors affecting refractive outcome after cataract surgery in primary angle-closure glaucoma. Clin Exp Ophthalmol. 2016; 44:693–700.
Article11. Quigley HA. What's the choroid got to do with angle closure? Arch Ophthalmol. 2009; 127:693–694.
Article12. Quigley HA, Friedman DS, Congdon NG. Possible mechanisms of primary angle-closure and malignant glaucoma. J Glaucoma. 2003; 12:167–180.
Article13. Wang W, Zhang X. Choroidal thickness and primary open-angle glaucoma: a cross-sectional study and meta-analysis. Invest Ophthalmol Vis Sci. 2014; 55:6007–6014.
Article14. Wang YX, Xu L, Shao L, et al. Subfoveal choroidal thickness and glaucoma. The Beijing Eye Study 2011. PLoS One. 2014; 9:e107321.
Article15. Zhang X, Wang W, Aung T, et al. Choroidal physiology and primary angle closure disease. Surv Ophthalmol. 2015; 60:547–556.
Article16. Baek S, Sung KR, Sun JH, et al. A hierarchical cluster analysis of primary angle closure classification using anterior segment optical coherence tomography parameters. Invest Ophthalmol Vis Sci. 2013; 54:848–853.
Article17. Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. Br J Ophthalmol. 2002; 86:238–242.
Article18. Retzlaff JA, Sanders DR, Kraff MC. Development of the SRK/T intraocular lens implant power calculation formula. J Cataract Refract Surg. 1990; 16:333–340.
Article19. Hong JW, Yun SC, Sung KR, Lee JE. Clinical and anterior segment anatomical features in primary angle closure subgroups based on configurations of iris root insertion. Korean J Ophthalmol. 2016; 30:206–213.
Article20. Lee KS, Sung KR, Shon K, et al. Longitudinal changes in anterior segment parameters after laser peripheral iridotomy assessed by anterior segment optical coherence tomography. Invest Ophthalmol Vis Sci. 2013; 54:3166–3170.
Article21. Gao X, Huang W, Wang W, et al. Topographic profile of choroid in eyes after acute primary angle-closure. Can J Ophthalmol. 2016; 51:354–361.
Article22. Huang W, Wang W, Gao X, et al. Choroidal thickness in the subtypes of angle closure: an EDI-OCT study. Invest Ophthalmol Vis Sci. 2013; 54:7849–7853.
Article23. Chung HS, Sung KR, Lee KS, et al. Relationship between the lamina cribrosa, outer retina, and choroidal thickness as assessed using spectral domain optical coherence tomography. Korean J Ophthalmol. 2014; 28:234–240.
Article24. Zhou M, Wang W, Huang W, et al. Is increased choroidal thickness association with primary angle closure? Acta Ophthalmol. 2014; 92:e514–e520.
Article25. Wang W, Zhou M, Huang W, et al. Does acute primary angle-closure cause an increased choroidal thickness? Invest Ophthalmol Vis Sci. 2013; 54:3538–3545.
Article26. Song W, Huang P, Dong X, et al. Choroidal thickness decreased in acute primary angle closure attacks with elevated intraocular pressure. Curr Eye Res. 2016; 41:526–531.
Article27. Lee JR, Sung KR, Han S. Comparison of anterior segment parameters between the acute primary angle closure eye and the fellow eye. Invest Ophthalmol Vis Sci. 2014; 55:3646–3650.
Article28. Nongpiur ME, He M, Amerasinghe N, et al. Lens vault, thickness, and position in Chinese subjects with angle closure. Ophthalmology. 2011; 118:474–479.
Article29. Marchini G, Pagliarusco A, Toscano A, et al. Ultrasound biomicroscopic and conventional ultrasonographic study of ocular dimensions in primary angle-closure glaucoma. Ophthalmology. 1998; 105:2091–2098.30. How AC, Baskaran M, Kumar RS, et al. Changes in anterior segment morphology after laser peripheral iridotomy: an anterior segment optical coherence tomography study. Ophthalmology. 2012; 119:1383–1387.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Refractive Change After Cataract Surgery in Patients With Acute Primary Angle Closure
- Factors Affecting Post-Cataract OCT Parameters in Open-Angle and Angle-Closure Glaucoma Eyes: Optic Disc Head Analysis
- Influence of Biometric Variables on Refractive Outcomes after Cataract Surgery in Angle-closure Glaucoma Patients
- The Variation of Choroidal Thickness and Refractive Error after Cataract Surgery
- The Relationship among Refractive Power, Axial Length and Choroidal Thickness Measured by SD-OCT in Myopia