Korean J Pain.
2018 Oct;31(4):289-295. 10.3344/kjp.2018.31.4.289.
The comparison of two different intraarticular injections using a sonographic anterolateral approach in patients with osteoarthritic knee
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chonbuk National University Medical School and Hospital, Jeonju, Korea. sjs6803@chonbuk.ac.kr
- 2Department of Preventive Medicine, Chonbuk National University Medical School, Jeonju, Korea.
- 3Department of Oral and Maxillofacial Surgery, Chonbuk National University School of Dentistry, Jeonju, Korea.
- KMID: 2421520
- DOI: http://doi.org/10.3344/kjp.2018.31.4.289
Abstract
- BACKGROUND
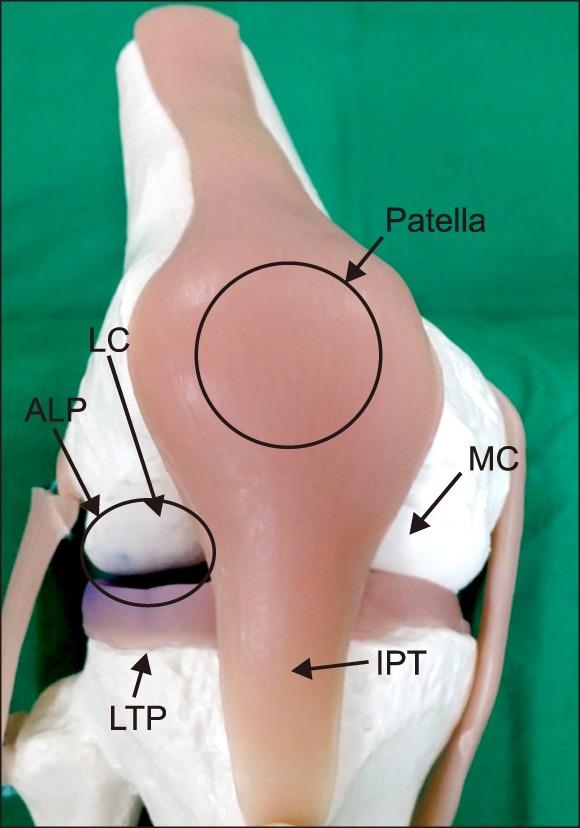
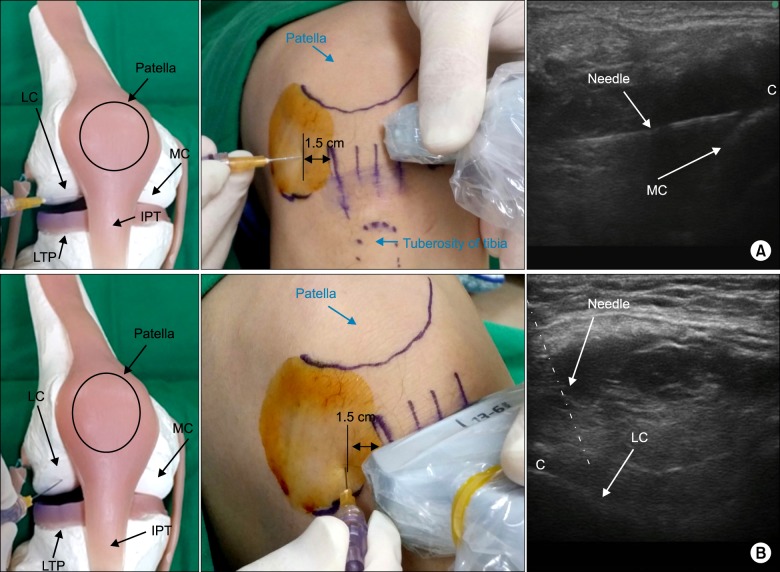
The intraarticular (IA) injection has become popular for the management of the osteoarthritic knee without an effusion. The success rate of IA injection would be better if it was able to be visually confirmed. We hypothesized that an anterolateral approach, which targets the synovial membrane of the lateral condyle using ultrasound, would provide an equivalent alternative to the anterolateral approach, targeting the synovial membrane of the medial condyle for IA injection of the knee.
METHODS
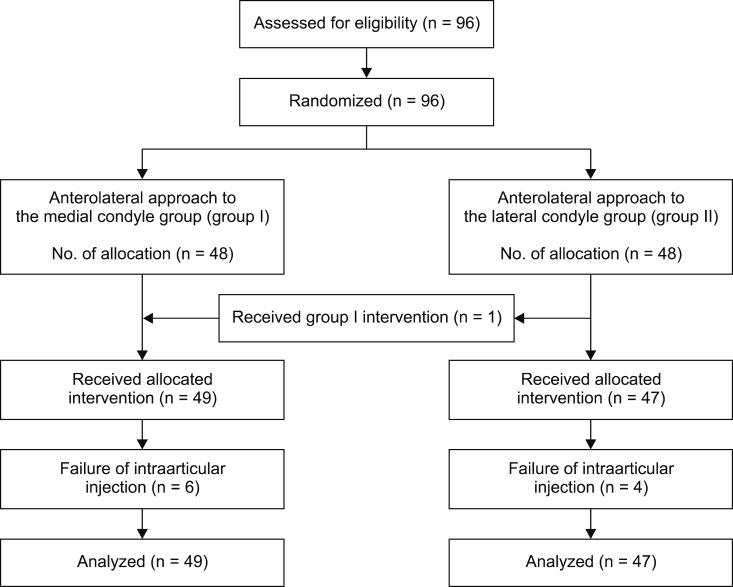
A total of 96 knees with osteoarthritis were randomized placed into the two groups, which were group I (anterolateral approach to the medial condyle) and group II (anterolateral approach to the lateral condyle). The primary outcome was to compare the success rate of the two methods of IA injection. The required length of the needle for injection was also measured and compared. Pain intensity was assessed using the Numeric Rating Scale in order to evaluate the success of injection.
RESULTS
There were no significant differences in the success rate between both groups. The success rate of group I and group II were 87.8% (95%, CI 78.7-97.0) and 91.5% (95%, CI 83.6-99.5), respectively (P = 0.549). The needle depth was 5.0 ± 0.8 (3.0 to 6.1 cm) in group I, and 3.0 ± 0.8 (1.5 to 5 cm) in group II (P < 0.001).
CONCLUSIONS
The anterolateral approach to the lateral femoral condyle, using ultrasound, is an alternative method to the approach targeting the medial femoral condyle, using shorter needle.
Keyword
MeSH Terms
Figure
Reference
-
1. Jackson DW, Simon TM, Aberman HM. Symptomatic articular cartilage degeneration: the impact in the new millennium. Clin Orthop Relat Res. 2001; (391 Suppl):S14–S25. PMID: 11603698.2. Balazs EA, Denlinger JL. Viscosupplementation: a new concept in the treatment of osteoarthritis. J Rheumatol Suppl. 1993; 39:3–9. PMID: 8410881.3. Leopold SS, Redd BB, Warme WJ, Wehrle PA, Pettis PD, Shott S. Corticosteroid compared with hyaluronic acid injections for the treatment of osteoarthritis of the knee. A prospective, randomized trial. J Bone Joint Surg Am. 2003; 85-A:1197–1203. PMID: 12851342.4. Schumacher HR, Chen LX. Injectable corticosteroids in treatment of arthritis of the knee. Am J Med. 2005; 118:1208–1214. PMID: 16271901.
Article5. Jackson DW, Evans NA, Thomas BM. Accuracy of needle placement into the intra-articular space of the knee. J Bone Joint Surg Am. 2002; 84-A:1522–1527. PMID: 12208907.
Article6. Chavez-Chiang CE, Sibbitt WL Jr, Band PA, Chavez-Chiang NR, DeLea SL, Bankhurst AD. The highly accurate anteriolateral portal for injecting the knee. Sports Med Arthrosc Rehabil Ther Technol. 2011; 3:6. PMID: 21447197.
Article7. Sibbitt WL Jr, Peisajovich A, Michael AA, Park KS, Sibbitt RR, Band PA, et al. Does sonographic needle guidance affect the clinical outcome of intraarticular injections? J Rheumatol. 2009; 36:1892–1902. PMID: 19648304.
Article8. Qvistgaard E, Kristoffersen H, Terslev L, Danneskiold-Samsøe B, Torp-Pedersen S, Bliddal H. Guidance by ultrasound of intra-articular injections in the knee and hip joints. Osteoarthritis Cartilage. 2001; 9:512–517. PMID: 11520164.
Article9. Esenyel C, Demirhan M, Esenyel M, Sonmez M, Kahraman S, Senel B, et al. Comparison of four different intra- articular injection sites in the knee: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2007; 15:573–577. PMID: 17149645.
Article10. Cunnington J, Marshall N, Hide G, Bracewell C, Isaacs J, Platt P, et al. A randomized, double-blind, controlled study of ultrasound-guided corticosteroid injection into the joint of patients with inflammatory arthritis. Arthritis Rheum. 2010; 62:1862–1869. PMID: 20222114.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterolateral Portal Is Less Painful than Superolateral Portal in Knee Intra-Articular Injection
- The Analgesic Effect of Intraarticular Morphine in Osteoarthritis of Knee
- Septic Arthritis after Intra-articular Hyaluronic Acid Injections in Patients with Knee Osteoarthritis: A report of two cases
- The Analgesic Effect of Intraarticular Bupivacaine and Morphine after Arthroscopic Knee Surgery
- Tumoral Calcinosis in The Knee Joint Causing Acute Symptoms : A Case Report