J Korean Soc Radiol.
2018 Oct;79(4):218-226. 10.3348/jksr.2018.79.4.218.
A Radiologic Overview of Aspiration-Induced Lung Disease in Adults
- Affiliations
-
- 1Department of Radiology, Korea University Guro Hospital, College of Medicine, Korea University, Seoul, Korea. keyrad@korea.ac.kr
- 2Department of Radiology, Korea University Ansan Hospital, College of Medicine, Korea University, Ansan, Korea.
- 3Department of Radiology, Korea University Anam Hospital, College of Medicine, Korea University, Seoul, Korea.
- KMID: 2421225
- DOI: http://doi.org/10.3348/jksr.2018.79.4.218
Abstract
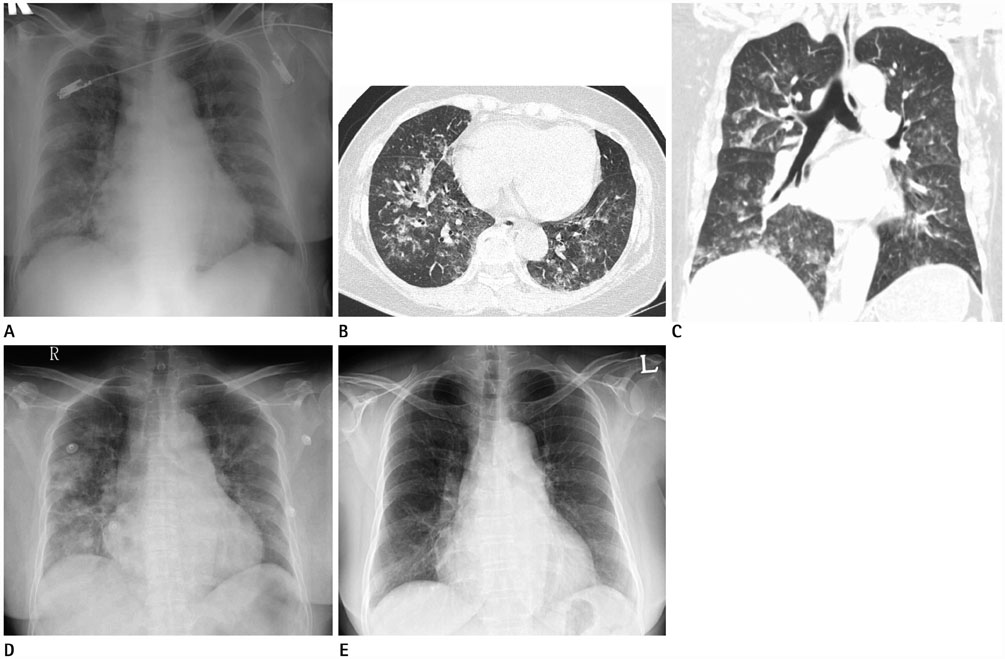
- Aspiration is defined as accidental entrance of foreign matter into the lower respiratory tract, and is a common event and can occur in healthy individuals. The type of aspiration-induced lung diseases depends on the quantity and nature of the aspirated material, the chronicity, and the host responses. Aspiration into the airways and lungs can cause a wide spectrum of lung diseases with various manifestations in adults. Diseases with predominantly airway manifestation include foreign body aspiration and diffuse aspiration bronchiolitis. Diseases with predominantly lung parenchymal manifestation include acute diseases such as aspiration pneumonia, aspiration pneumonitis, and near drowning, and chronic diseases such as chronic exogenous lipoid pneumonia and chronic interstitial lung disease. Definitive diagnosis of aspiration-induced lung diseases is challenging to make. Awareness of radiologic findings associated with these diseases is essential for accurate diagnosis and management of these diverse aspiration-induced lung diseases.
MeSH Terms
Figure
Reference
-
1. Hu X, Lee JS, Pianosi PT, Ryu JH. Aspiration-related pulmonary syndromes. Chest. 2015; 147:815–823.
Article2. Marik PE. Pulmonary aspiration syndromes. Curr Opin Pulm Med. 2011; 17:148–154.
Article3. DiBardino DM, Wunderink RG. Aspiration pneumonia: a review of modern trends. J Crit Care. 2015; 30:40–48.
Article4. Boyd M, Chatterjee A, Chiles C, Chin R Jr. Tracheobronchial foreign body aspiration in adults. South Med J. 2009; 102:171–174.
Article5. Sehgal IS, Dhooria S, Ram B, Singh N, Aggarwal AN, Gupta D, et al. Foreign body inhalation in the adult population: experience of 25998 bronchoscopies and systematic review of the literature. Respir Care. 2015; 60:1438–1448.
Article6. Franquet T, Giménez A, Rosón N, Torrubia S, Sabaté JM, Pérez C. Aspiration diseases: findings, pitfalls, and differential diagnosis. Radiographics. 2000; 20:673–685.
Article7. Matsuse T, Oka T, Kida K, Fukuchi Y. Importance of diffuse aspiration bronchiolitis caused by chronic occult aspiration in the elderly. Chest. 1996; 110:1289–1293.
Article8. Prather AD, Smith TR, Poletto DM, Tavora F, Chung JH, Nallamshetty L, et al. Aspiration-related lung diseases. J Thorac Imaging. 2014; 29:304–309.
Article9. Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001; 344:665–671.
Article10. Teramoto S, Fukuchi Y, Sasaki H, Sato K, Sekizawa K, Matsuse T. High incidence of aspiration pneumonia in community-and hospital-acquired pneumonia in hospitalized patients: a multicenter, prospective study in Japan. J Am Geriatr Soc. 2008; 56:577–579.11. Komiya K, Ishii H, Umeki K, Mizunoe S, Okada F, Johkoh T, et al. Impact of aspiration pneumonia in patients with community-acquired pneumonia and healthcare-associated pneumonia: a multicenter retrospective cohort study. Respirology. 2013; 18:514–521.
Article12. Komiya K, Ishii H, Umeki K, Kawamura T, Okada F, Okabe E, et al. Computed tomography findings of aspiration pneumonia in 53 patients. Geriatr Gerontol Int. 2013; 13:580–585.
Article13. Yi MS, Kim KI, Jeong YJ, Park HK, Lee MK. CT findings in hydrocarbon pneumonitis after diesel fuel siphonage. AJR Am J Roentgenol. 2009; 193:1118–1121.
Article14. Gentina T, Tillie-Leblond I, Birolleau S, Saidi F, Saelens T, Boudoux L, et al. Fire-eater's lung: seventeen cases and a review of the literature. Medicine (Baltimore). 2001; 80:291–229.15. Kadakal F, Uysal MA, Gülhan NB, Turan NG, Bayramogğlu S, Yilmaz V. Fire-eater's pneumonia characterized by pneumatocele formation and spontaneous resolution. Diagn Interv Radiol. 2010; 16:201–203.16. Gregorakos L, Markou N, Psalida V, Kanakaki M, Alexopoulou A, Sotiriou E, et al. Near-drowning: clinical course of lung injury in adults. Lung. 2009; 187:93–97.
Article17. Rossi SE, Erasmus JJ, Volpacchio M, Franquet T, Castiglioni T, McAdams HP. “Crazy-paving” pattern at thin-section CT of the lungs: radiologic-pathologic overview. Radiographics. 2003; 23:1509–1519.
Article18. Lee JS, Im JG, Song KS, Seo JB, Lim TH. Exogenous lipoid pneumonia: high-resolution CT findings. Eur Radiol. 1999; 9:287–291.
Article19. Tobin RW, Pope CE II, Pellegrini CA, Emond MJ, Sillery J, Raghu G. Increased prevalence of gastroesophageal reflux in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998; 158:1804–1808.
Article20. Lee JS, Song JW, Wolters PJ, Elicker BM, King TE Jr, Kim DS, et al. Bronchoalveolar lavage pepsin in acute exacerbation of idiopathic pulmonary fibrosis. Eur Respir J. 2012; 39:352–358.
Article21. Christmann RB, Wells AU, Capelozzi VL, Silver RM. Gastroesophageal reflux incites interstitial lung disease in systemic sclerosis: clinical, radiologic, histopathologic, and treatment evidence. Semin Arthritis Rheum. 2010; 40:241–249.
Article