Ann Surg Treat Res.
2018 Oct;95(4):175-182. 10.4174/astr.2018.95.4.175.
Focal change of the pancreatic texture using a direct injection mixture of N-butyl cyanoacrylate and lipiodol in the pig model: a strategy for preventing pancreatic leakage during pancreatic surgery
- Affiliations
-
- 1Department of Trauma and Surgical Critical Care, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Hepato-Biliary and Pancreas Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. gshth@catholic.ac.kr
- KMID: 2421195
- DOI: http://doi.org/10.4174/astr.2018.95.4.175
Abstract
- PURPOSE
A soft texture of the pancreas is one of the most important predisposing factors for a pancreatic fistula. Thus, in a porcine model, we investigated a method to harden the pancreas locally by directly injecting an artificial material.
METHODS
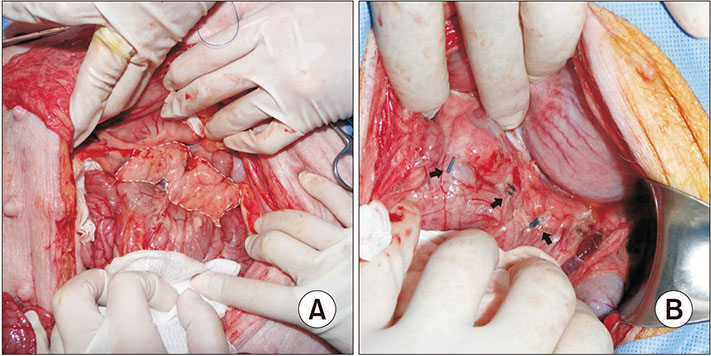
During the laparotomy, 51 samples from 17 pigs, including 13 survival models, were randomly divided into 3 groups and either received a direct injection into the pancreas of MHL (1:4 mixture of histoacryl [n-butyl cyanoacrylate] and lipiodol) (group E) or saline (group C) or only received a pinprick into the pancreas without injecting a substance (sham). We measured the change in the pancreatic hardness after the injection using a durometer and examined the histological change of the pancreas using the fibrosis grade in the survival model.
RESULTS
The postinjection hardness of the pancreas was significantly increased in group E compared to group C and the sham group (P < 0.001). Pathologically, all cases in group E showed a severe fibrotic change, whereas the other groups demonstrated mild to no fibrosis (P < 0.001). The fibrosis in group E was localized to the area of the injection, while the surrounding areas were preserved.
CONCLUSION
The direct injection of MHL could induce focal hardening and fibrotic changes in the pancreas of the porcine model.
MeSH Terms
Figure
Reference
-
1. Wellner UF, Kayser G, Lapshyn H, Sick O, Makowiec F, Hoppner J, et al. A simple scoring system based on clinical factors related to pancreatic texture predicts postoperative pancreatic fistula preoperatively. HPB (Oxford). 2010; 12:696–702.
Article2. Belyaev O, Munding J, Herzog T, Suelberg D, Tannapfel A, Schmidt WE, et al. Histomorphological features of the pancreatic remnant as independent risk factors for postoperative pancreatic fistula: a matched-pairs analysis. Pancreatology. 2011; 11:516–524.
Article3. Sato N, Yamaguchi K, Chijiiwa K, Tanaka M. Risk analysis of pancreatic fistula after pancreatic head resection. Arch Surg. 1998; 133:1094–1098.
Article4. Wellner U, Makowiec F, Fischer E, Hopt UT, Keck T. Reduced postoperative pancreatic fistula rate after pancreatogastrostomy versus pancreaticojejunostomy. J Gastrointest Surg. 2009; 13:745–751.
Article5. Konstadoulakis MM, Filippakis GM, Lagoudianakis E, Antonakis PT, Dervenis C, Bramis J. Intra-arterial bolus octreotide administration during Whipple procedure in patients with fragile pancreas: a novel technique for safer pancreaticojejunostomy. J Surg Oncol. 2005; 89:268–272.
Article6. Torer N, Ezer A, Nursal TZ. Mattress sutures for the modification of end-to-end dunking pancreaticojejunostomy. Hepatobiliary Pancreat Dis Int. 2013; 12:556–558.
Article7. Hashimoto Y, Traverso LW. Incidence of pancreatic anastomot ic fai lure and delayed gastric emptying after pancreatoduodenectomy in 507 consecutive patients: use of a web-based calculator to improve homogeneity of definition. Surgery. 2010; 147:503–515.8. Gaujoux S, Cortes A, Couvelard A, Noullet S, Clavel L, Rebours V, et al. Fatty pancreas and increased body mass index are risk factors of pancreatic fistula after pancreaticoduodenectomy. Surgery. 2010; 148:15–23.
Article9. Yeo CJ, Cameron JL, Maher MM, Sauter PK, Zahurak ML, Talamini MA, et al. A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg. 1995; 222:580–588.
Article10. Suzuki Y, Fujino Y, Tanioka Y, Hori Y, Ueda T, Takeyama Y, et al. Randomized clinical trial of ultrasonic dissector or conventional division in distal pancreatectomy for non-fibrotic pancreas. Br J Surg. 1999; 86:608–611.
Article11. Foitzik T, Gock M, Schramm C, Prall F, Klar E. Octreotide hardens the pancreas. Langenbecks Arch Surg. 2006; 391:108–112.
Article12. Yonemitsu T, Kawai N, Sato M, Sonomura T, Takasaka I, Nakai M, et al. Comparison of hemostatic durability between N-butyl cyanoacrylate and gelatin sponge particles in transcatheter arterial embolization for acute arterial hemorrhage in a coagulopathic condition in a swine model. Cardiovasc Intervent Radiol. 2010; 33:1192–1197.
Article13. Sato N, Yamaguchi K, Yokohata K, Shimizu S, Morisaki T, Mizumoto K, et al. Preoperative exocrine pancreatic function predicts risk of leakage of pancreaticojejunostomy. Surgery. 1998; 124:871–876.
Article14. Uchida E, Tajiri T, Nakamura Y, Aimoto T, Naito Z. Relationship between grade of fibrosis in pancreatic stump and postoperative pancreatic exocrine activity after pancreaticoduodenectomy: with special reference to insufficiency of pancreaticointestinal anastomosis. J Nippon Med Sch. 2002; 69:549–556.
Article15. Williams ST, Woltering EA, O'Dorisio TM, Fletcher WS. Effect of octreotide acetate on pancreatic exocrine function. Am J Surg. 1989; 157:459–462.
Article16. McCormick PA, Seifalian AM, Stansby G, McGann G, Collins P, Chin J, et al. Superior mesenteric artery blood flow in man measured with intra-arterial Doppler catheters: effect of octreotide. J Hepatol. 1993; 17:20–27.17. Ahmadi A, Nikkhoo B, Mokarizadeh A, Rahmani MR, Fakhari S, Mohammadi M, et al. An optimised mouse model of chronic pancreatitis with a combination of ethanol and cerulein. Cent Eur J Immunol. 2016; 41:54–63.
Article18. Rajoriya N, Forrest EH, Gray J, Stuart RC, Carter RC, McKay CJ, et al. Long-term follow-up of endoscopic Histoacryl glue injection for the management of gastric variceal bleeding. QJM. 2011; 104:41–47.
Article19. Yue J, Sun X, Cai J, Yin FF, Yin Y, Zhu J, et al. Lipiodol: a potential direct surrogate for cone-beam computed tomography image guidance in radiotherapy of liver tumor. Int J Radiat Oncol Biol Phys. 2012; 82:834–841.
Article20. Hawkins MA, Brock KK, Eccles C, Moseley D, Jaffray D, Dawson LA. Assessment of residual error in liver position using kV cone-beam computed tomography for liver cancer high-precision radiation therapy. Int J Radiat Oncol Biol Phys. 2006; 66:610–619.
Article21. Lee GH, Kim JH, Lee KJ, Yoo BM, Hahm KB, Cho SW, et al. Life-threatening intra-abdominal arterial embolization after histoacryl injection for bleeding gastric ulcer. Endoscopy. 2000; 32:422–424.
Article22. Fan CS, Soon MS. Portal vein embolization as a complication of Histoacryl injection for a bleeding giant gastric ulcer. Endoscopy. 2007; 39:Suppl 1. E110.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous N-Butyl Cyanoacrylate Embolization of a Pancreatic Pseudoaneurysm after Failed Attempts of Transcatheter Embolization
- The Risk Factors of Pancreatic Fistula after Pancratoduodenectomy
- A model for predicting pancreatic leakage after pancreaticoduodenectomy based on the international study group of pancreatic surgery classification
- Experimental Embolization Using Histoacryl Blue (N-butyl 2-cyanoacrylate) in Pig Rete Mirabile
- Successful endoscopic closure of an esophageal leak after endoscopic ultrasound-guided hepaticoesophagostomy by using n-butyl-2 cyanoacrylate