Korean Circ J.
2018 Oct;48(10):863-872. 10.4070/kcj.2018.0255.
De-Escalation of P2Yâ‚â‚‚ Receptor Inhibitor Therapy after Acute Coronary Syndromes in Patients Undergoing Percutaneous Coronary Intervention
- Affiliations
-
- 1Department of Cardiology, LMU Munich, Marchioninistraße 15, München, Germany. dirk.sibbing@med.uni-muenchen.de, danny.kupka@med.uni-muenchen.de
- 2DZHK (German Centre for Cardiovascular Research), Munich Heart Alliance, München, Germany.
- KMID: 2420639
- DOI: http://doi.org/10.4070/kcj.2018.0255
Abstract
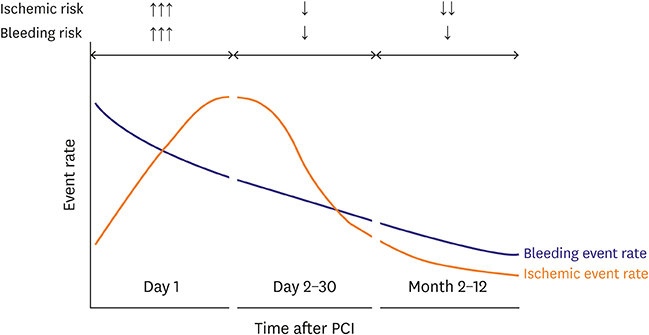
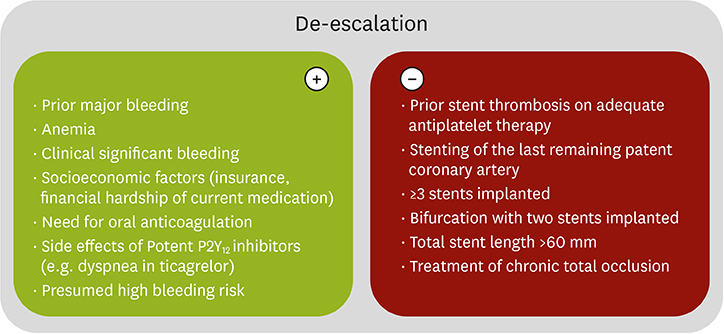
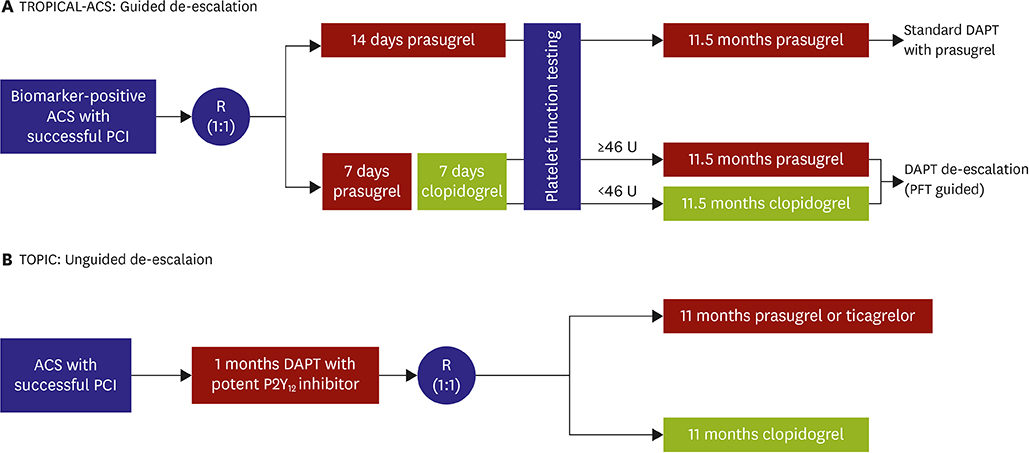
- Dual antiplatelet therapy (DAPT) "” a combination of a P2Yâ‚â‚‚ receptor inhibitor and aspirin "” has revolutionized antithrombotic treatment. Potent P2Yâ‚â‚‚ inhibitors such as prasugrel and ticagrelor exhibit a strong and more consistent platelet inhibition when compared to clopidogrel. Therefore, ticagrelor and prasugrel significantly reduce ischemic events, but at an expense of an increased bleeding risk in acute coronary syndrome (ACS) patients undergoing percutaneous coronary intervention (PCI). These observations have engaged intensive clinical research in alternative DAPT regimens to achieve sufficient platelet inhibition with an acceptable bleeding risk. Our review focusses on P2Yâ‚â‚‚ receptor therapy de-escalation defined as a switch from a potent antiplatelet agent (ticagrelor or prasugrel) to clopidogrel. Recently, both unguided (platelet function testing independent) and guided (platelet function testing dependent) DAPT de-escalation strategies have been investigated in different clinical studies and both switching strategies could be possible options to prevent bleeding complications without increasing ischemic risk. In light of the still limited data currently available, future large-scale trials should accumulate more data on various DAPT de-escalation regimens with both ticagrelor and prasugrel in unguided and guided de-escalation approaches. In the current review we aim at summarizing and discussing the current evidence on this still emerging topic in the field of antiplatelet treatment.
MeSH Terms
Figure
Cited by 2 articles
-
Unguided De-Escalation Strategy From Potent P2Y12 Inhibitors in Patients Presented With ACS: When, Whom and How?
Jin Sup Park, Young-Hoon Jeong
Korean Circ J. 2022;52(4):320-323. doi: 10.4070/kcj.2022.0022.Prasugrel-based De-Escalation of Dual Antiplatelet Therapy After Percutaneous Coronary Intervention in Patients With STEMI
You-Jeong Ki, Bong Ki Lee, Kyung Woo Park, Jang-Whan Bae, Doyeon Hwang, Jeehoon Kang, Jung-Kyu Han, Han-Mo Yang, Hyun-Jae Kang, Bon-Kwon Koo, Dong-Bin Kim, In-Ho Chae, Keon-Woong Moon, Hyun Woong Park, Ki-Bum Won, Dong Woon Jeon, Kyoo-Rok Han, Si Wan Choi, Jae Kean Ryu, Myung Ho Jeong, Kwang Soo Cha, Hyo-Soo Kim,
Korean Circ J. 2021;52(4):304-319. doi: 10.4070/kcj.2021.0293.
Reference
-
1. Schömig A, Neumann FJ, Kastrati A, et al. A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary-artery stents. N Engl J Med. 1996; 334:1084–1089.
Article2. Franchi F, Angiolillo DJ. Novel antiplatelet agents in acute coronary syndrome. Nat Rev Cardiol. 2015; 12:30–47.
Article3. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009; 361:1045–1057.4. Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007; 357:2001–2015.
Article5. Sibbing D, Angiolillo DJ, Huber K. Antithrombotic therapy for acute coronary syndrome: past, present and future. Thromb Haemost. 2017; 117:1240–1248.
Article6. Rollini F, Franchi F, Angiolillo DJ. Switching P2Y12-receptor inhibitors in patients with coronary artery disease. Nat Rev Cardiol. 2016; 13:11–27.
Article7. Angiolillo DJ, Rollini F, Storey RF, et al. International expert consensus on switching platelet P2Y12 receptor-inhibiting therapies. Circulation. 2017; 136:1955–1975.8. Velders MA, Abtan J, Angiolillo DJ, et al. Safety and efficacy of ticagrelor and clopidogrel in primary percutaneous coronary intervention. Heart. 2016; 102:617–625.
Article9. Bagai A, Peterson ED, Honeycutt E, et al. In-hospital switching between adenosine diphosphate receptor inhibitors in patients with acute myocardial infarction treated with percutaneous coronary intervention: Insights into contemporary practice from the TRANSLATE-ACS study. Eur Heart J Acute Cardiovasc Care. 2015; 4:499–508.
Article10. Motovska Z, Hlinomaz O, Kala P, et al. 1-year outcomes of patients undergoing primary angioplasty for myocardial infarction treated with prasugrel versus ticagrelor. J Am Coll Cardiol. 2018; 71:371–381.11. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 64:e139–228.12. Valgimigli M, Bueno H, Byrne RA, et al. ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2017; 2017:26.13. Ibanez B, James S, Agewall S, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2017; 2017:26.14. Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016; 37:267–315.15. Montalescot G, Wiviott SD, Braunwald E, et al. Prasugrel compared with clopidogrel in patients undergoing percutaneous coronary intervention for ST-elevation myocardial infarction (TRITON-TIMI 38): double-blind, randomised controlled trial. Lancet. 2009; 373:723–731.
Article16. Wiviott SD, Braunwald E, Angiolillo DJ, et al. Greater clinical benefit of more intensive oral antiplatelet therapy with prasugrel in patients with diabetes mellitus in the trial to assess improvement in therapeutic outcomes by optimizing platelet inhibition with prasugrel-Thrombolysis in Myocardial Infarction 38. Circulation. 2008; 118:1626–1636.
Article17. Antman EM, Wiviott SD, Murphy SA, et al. Early and late benefits of prasugrel in patients with acute coronary syndromes undergoing percutaneous coronary intervention: a TRITON-TIMI 38 (TRial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet InhibitioN with Prasugrel-Thrombolysis In Myocardial Infarction) analysis. J Am Coll Cardiol. 2008; 51:2028–2033.18. Becker RC, Bassand JP, Budaj A, et al. Bleeding complications with the P2Y12 receptor antagonists clopidogrel and ticagrelor in the PLATelet inhibition and patient Outcomes (PLATO) trial. Eur Heart J. 2011; 32:2933–2944.
Article19. Saito S, Isshiki T, Kimura T, et al. Efficacy and safety of adjusted-dose prasugrel compared with clopidogrel in Japanese patients with acute coronary syndrome: the PRASFIT-ACS study. Circ J. 2014; 78:1684–1692.20. Cannon CP, Bhatt DL, Oldgren J, et al. Dual antithrombotic therapy with dabigatran after PCI in atrial fibrillation. N Engl J Med. 2017; 377:1513–1524.
Article21. Alexopoulos D, Xanthopoulou I, Deftereos S, et al. In-hospital switching of oral P2Y12 inhibitor treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention: prevalence, predictors and short-term outcome. Am Heart J. 2014; 167:68–76.e2.
Article22. Clemmensen P, Grieco N, Ince H, et al. MULTInational non-interventional study of patients with ST-segment elevation myocardial infarction treated with PRimary Angioplasty and Concomitant use of upstream antiplatelet therapy with prasugrel or clopidogrel--the European MULTIPRAC Registry. Eur Heart J Acute Cardiovasc Care. 2015; 4:220–229.23. De Luca L, Leonardi S, Cavallini C, et al. Contemporary antithrombotic strategies in patients with acute coronary syndrome admitted to cardiac care units in Italy: The EYESHOT Study. Eur Heart J Acute Cardiovasc Care. 2015; 4:441–452.
Article24. Bonaca MP, Bhatt DL, Cohen M, et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med. 2015; 372:1791–1800.
Article25. Alexopoulos D, Xanthopoulou I, Perperis A, et al. Dyspnea in patients treated with P2Y12 receptor antagonists: insights from the GReek AntiPlatElet (GRAPE) registry. Platelets. 2017; 28:691–697.26. Bonaca MP, Bhatt DL, Oude Ophuis T, et al. Long-term tolerability of ticagrelor for the secondary prevention of major adverse cardiovascular events: a secondary analysis of the PEGASUS-TIMI 54 trial. JAMA Cardiol. 2016; 1:425–432.27. Cuisset T, Deharo P, Quilici J, et al. Benefit of switching dual antiplatelet therapy after acute coronary syndrome: the TOPIC (timing of platelet inhibition after acute coronary syndrome) randomized study. Eur Heart J. 2017; 38:3070–3078.
Article28. Sibbing D, Aradi D, Jacobshagen C, et al. A randomised trial on platelet function-guided de-escalation of antiplatelet treatment in ACS patients undergoing PCI. Rationale and design of the Testing Responsiveness to Platelet Inhibition on Chronic Antiplatelet Treatment for Acute Coronary Syndromes (TROPICAL-ACS) Trial. Thromb Haemost. 2017; 117:188–195.29. Sibbing D, Aradi D, Jacobshagen C, et al. Guided de-escalation of antiplatelet treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention (TROPICAL-ACS): a randomised, open-label, multicentre trial. Lancet. 2017; 390:1747–1757.30. Zettler ME, Peterson ED, McCoy LA, et al. Switching of adenosine diphosphate receptor inhibitor after hospital discharge among myocardial infarction patients: Insights from the Treatment with Adenosine Diphosphate Receptor Inhibitors: Longitudinal Assessment of Treatment Patterns and Events after Acute Coronary Syndrome (TRANSLATE-ACS) observational study. Am Heart J. 2017; 183:62–68.
Article31. Motovska Z, Hlinomaz O, Miklik R, et al. Prasugrel versus ticagrelor in patients with acute myocardial infarction treated with primary percutaneous coronary intervention: multicenter randomized PRAGUE-18 Study. Circulation. 2016; 134:1603–1612.32. De Luca L, D'Ascenzo F, Musumeci G, et al. Incidence and outcome of switching of oral platelet P2Y12 receptor inhibitors in patients with acute coronary syndromes undergoing percutaneous coronary intervention: the SCOPE registry. EuroIntervention. 2017; 13:459–466.
Article33. Deharo P, Quilici J, Camoin-Jau L, et al. Benefit of switching dual antiplatelet therapy after acute coronary syndrome according to on-treatment platelet reactivity: the TOPIC-VASP pre-specified analysis of the TOPIC randomized study. JACC Cardiovasc Interv. 2017; 10:2560–2570.34. Gurbel PA, Bliden KP, Hiatt BL, O'Connor CM. Clopidogrel for coronary stenting: response variability, drug resistance, and the effect of pretreatment platelet reactivity. Circulation. 2003; 107:2908–2913.35. Tantry US, Bonello L, Aradi D, et al. Consensus and update on the definition of on-treatment platelet reactivity to adenosine diphosphate associated with ischemia and bleeding. J Am Coll Cardiol. 2013; 62:2261–2273.
Article36. Gurbel PA, Bliden KP, Samara W, et al. Clopidogrel effect on platelet reactivity in patients with stent thrombosis: results of the CREST Study. J Am Coll Cardiol. 2005; 46:1827–1832.37. Sibbing D, Braun S, Morath T, et al. Platelet reactivity after clopidogrel treatment assessed with point-of-care analysis and early drug-eluting stent thrombosis. J Am Coll Cardiol. 2009; 53:849–856.
Article38. Aradi D, Kirtane A, Bonello L, et al. Bleeding and stent thrombosis on P2Y12-inhibitors: collaborative analysis on the role of platelet reactivity for risk stratification after percutaneous coronary intervention. Eur Heart J. 2015; 36:1762–1771.
Article39. Stone GW, Witzenbichler B, Weisz G, et al. Platelet reactivity and clinical outcomes after coronary artery implantation of drug-eluting stents (ADAPT-DES): a prospective multicentre registry study. Lancet. 2013; 382:614–623.
Article40. Cayla G, Cuisset T, Silvain J, et al. Platelet function monitoring to adjust antiplatelet therapy in elderly patients stented for an acute coronary syndrome (ANTARCTIC): an open-label, blinded-endpoint, randomised controlled superiority trial. Lancet. 2016; 388:2015–2022.
Article41. Sibbing D, Massberg S. Antiplatelet strategies in elderly people: still a long way to go. Lancet. 2016; 388:1962–1964.
Article42. Sibbing D, Gross L, Trenk D, et al. Age and outcomes following guided de-escalation of antiplatelet treatment in acute coronary syndrome patients undergoing percutaneous coronary intervention: results from the randomized TROPICAL-ACS trial. Eur Heart J. 2018; 39:2749–2758.
Article43. Levine GN, Jeong YH, Goto S, et al. Expert consensus document: World Heart Federation expert consensus statement on antiplatelet therapy in East Asian patients with ACS or undergoing PCI. Nat Rev Cardiol. 2014; 11:597–606.44. Mega JL, Close SL, Wiviott SD, et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009; 360:354–362.
Article45. Mega JL, Close SL, Wiviott SD, et al. Genetic variants in ABCB1 and CYP2C19 and cardiovascular outcomes after treatment with clopidogrel and prasugrel in the TRITON-TIMI 38 trial: a pharmacogenetic analysis. Lancet. 2010; 376:1312–1319.
Article46. Mega JL, Simon T, Collet JP, et al. Reduced-function CYP2C19 genotype and risk of adverse clinical outcomes among patients treated with clopidogrel predominantly for PCI: a meta-analysis. JAMA. 2010; 304:1821–1830.47. Wallentin L, James S, Storey RF, PLATO investigators, et al. Effect of CYP2C19 and ABCB1 single nucleotide polymorphisms on outcomes of treatment with ticagrelor versus clopidogrel for acute coronary syndromes: a genetic substudy of the PLATO trial. Lancet. 2010; 376:1320–1328.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- De-escalation strategies of dual antiplatelet therapy in patients undergoing percutaneous coronary intervention for acute coronary syndrome
- Dual antiplatelet therapy and non-cardiac surgery: evolving issues and anesthetic implications
- Recent Advances in Percutaneous Coronary Intervention in Coronary Artery Disease
- Staged versus One-Time Percutaneous Coronary Intervention Strategy for Multivessel Non-ST Segment Elevation Acute Coronary Syndrome
- Forearm Compartment Syndrome after Transradial Percutaneous Coronary Artery Intervention