J Korean Med Assoc.
2016 May;59(5):387-394. 10.5124/jkma.2016.59.5.387.
A systematic review of amniopatch
- Affiliations
-
- 1Division for New Health Technology Assessment, National Evidence-based Healthcare Collaborating Agency, Seoul, Korea. krjworld@neca.re.kr
- KMID: 2420638
- DOI: http://doi.org/10.5124/jkma.2016.59.5.387
Abstract
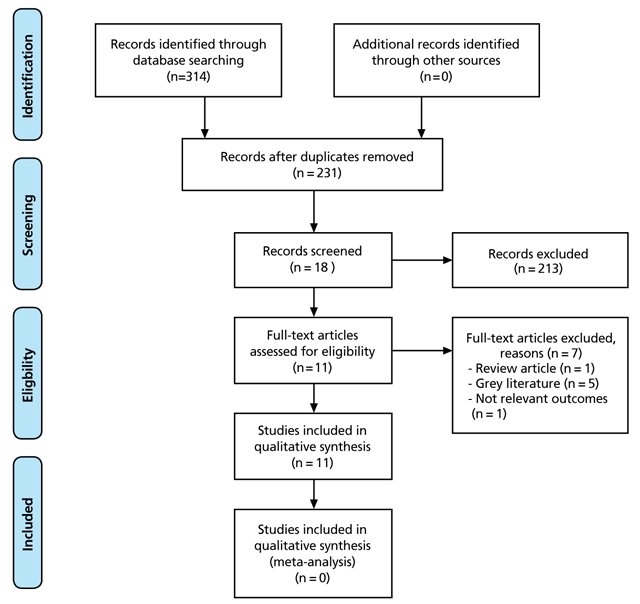
- The objective of this review is to evaluate the safety and effectiveness of the amniopatch procedure for the treatment ofpreterm premature rupture of the membranes. The searches were conducted via electronic databases including Ovid-MEDLINE, Ovid-Embase, the Cochrane Library, and eight Korean databases. In the study design, in addition to randomized controlled trials, case report studies in which patients underwent the amniopatch procedure were included. Two reviewers independently selected data in standardized form and assessed the methodological quality. Quality evaluation was performed by the SIGN (Scottish Intercollegiate Guideline Network) method. A total of 11 studies (2 cohort studies, 1 case series, and 8 case reports) were included. There were no serious maternal or fetal complications. It was reported that there were lower rates of maternal chorioamnionitis after the amniopatch relative to conservative treatment (control). The mean gestational age at delivery was 27.7 weeks (a total of 70 cases in 10 studies; spontaneous group, 27.6 weeks; iatrogenic group, 27.8 weeks). The amniopatch was successful in 46.6% of cases (33/71 cases in 11 studies). The overall neonatal survival rate was 55.3% (52/94 cases in 11 studies). Neonatal morbidity was 23.4% (11/47 cases in 7 studies). Although this systematic review, did not find clear evidence of the safety and effectiveness, the amniopatch procedure is a viable treatment option to prolong a pregnancy with previable premature rupture of membranes.
MeSH Terms
Figure
Reference
-
1. Bryant-Greenwood GD. The extracellular matrix of the human fetal membranes: structure and function. Placenta. 1998; 19:1–11.
Article2. Chung JY, Moon CS. Management of preterm premature rupture of membrane. Korean J Fetal Med. 2008; 4:199–207.3. Gupta A, Aneja A, Arora R, Sheghal R, Gupta P. Amniopatch: way forward for mid-trimester Premature Rupture of Membranes (PROM). J Fetal Med. 2014; 1:45–48.
Article4. Merenstein GB, Weisman LE. Premature rupture of the mem-branes: neonatal consequences. Semin Perinatol. 1996; 20:375–380.
Article5. Veille JC. Management of preterm premature rupture of membranes. Clin Perinatol. 1988; 15:851–862.
Article6. Moon SO, Koo YA, Choi SJ, Kim Hs, Oh SY, Roh CR, Kim JH. The optimal limit of gestational age for conservative management in preterm premature rupture of membranes. Korean J Fetal Med. 2005; 1:54–64.7. Quintero RA, Romero R, Dzieczkowski J, Mammen E, Evans MI. Sealing of ruptured amniotic membranes with intra-amniotic platelet-cryoprecipitate plug. Lancet. 1996; 347:1117.
Article8. Quintero RA. New horizons in the treatment of preterm premature rupture of membranes. Clin Perinatol. 2001; 28:861–875.
Article9. Deprest J, Emonds MP, Richter J, DeKoninck P, Van Mieghem T, Van Schoubroeck D, Devlieger R, De Catte L, Lewi L. Amniopatch for iatrogenic rupture of the fetal membranes. Prenat Diagn. 2011; 31:661–666.
Article10. Kwak HM, Choi HJ, Cha HH, Yu HJ, Lee JH, Choi SJ, Oh SY, Roh CR, Kim JH. Amniopatch treatment for spontaneous previable, preterm premature rupture of membranes associated or not with incompetent cervix. Fetal Diagn Ther. 2013; 33:47–54.
Article11. Quintero RA, Morales WJ, Allen M, Bornick PW, Arroyo J, LeParc G. Treatment of iatrogenic previable premature rupture of membranes with intra-amniotic injection of platelets and cryoprecipitate (amniopatch): preliminary experience. Am J Obstet Gynecol. 1999; 181:744–749.
Article12. Quintero RA, Morales WJ, Kalter CS, Allen M, Mendoza G, Angel JL, Romero R. Transabdominal intra-amniotic endoscopic assessment of previable premature rupture of membranes. Am J Obstet Gynecol. 1998; 179:71–76.
Article13. Ferianec V, Krizko M Jr, Papcun P, Svitekova K, Cizmar B, Holly I, Holoman K. Amniopatch: possibility of successful treatment of spontaneous previable rupture of membranes in the second trimester of pregnancy by transabdominal intraamiotic application of platelets and cryoprecipitate. Neuro Endocrinol Lett. 2011; 32:449–452.14. Louis-Sylvestre C, Rand JH, Gordon RE, Salafia CM, Berkowitz RL. In vitro studies of the interactions between platelets and amniotic membranes: a potential treatment for preterm premature rupture of the membranes. Am J Obstet Gynecol. 1998; 178:287–293.
Article15. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009; 62:1006–1012.
Article16. Scottish Intercollegiate Guidelines Network. Methodology checklists [Internet]. Edinburgh: Scottish Intercollegiate Guidelines Network;2011. cited 2014 Oct 17. Available from: http://www.sign.ac.uk/methodology/checklists.html.17. Quintero RA, Kontopoulos EV, Chmait R, Bornick PW, Allen M. Management of twin-twin transfusion syndrome in pregnancies with iatrogenic detachment of membranes following therapeutic amniocentesis and the role of interim amniopatch. Ultrasound Obstet Gynecol. 2005; 26:628–633.
Article18. Richter J, Henry A, Ryan G, DeKoninck P, Lewi L, Deprest J. Amniopatch procedure after previable iatrogenic rupture of the membranes: a two-center review. Prenat Diagn. 2013; 33:391–396.
Article19. Pathak B, Khan A, Assaf SA, Miller DA, Chmait RH. Amniopatch as a treatment for rupture of membranes following laser surgery for twin-twin transfusion syndrome. Fetal Diagn Ther. 2010; 27:134–137.
Article20. Cobo T, Borrell A, Fortuny A, Hernandez S, Perez M, Palacio M, Pereira A, Coll O. Treatment with amniopatch of premature rupture of membranes after first-trimester chorionic villus sampling. Prenat Diagn. 2007; 27:1024–1027.
Article21. Sipurzynski-Budrass S, Macher S, Haeusler M, Lanzer G. Successful treatment of premature rupture of membranes after genetic amniocentesis by intra-amniotic injection of platelets and cryoprecipitate (amniopatch): a case report. Vox Sang. 2006; 91:88–90.
Article22. Contino B, Armellino F, Brokaj L, Patroncini S. Amniopatch, a repairing technique for premature rupture of amniotic mem-branes in second trimester. Acta Biomed. 2004; 75:Suppl 1. 27–30.23. Lewi L, Van Schoubroeck D, Van Ranst M, Bries G, Emonds MP, Arabin B, Welch R, Deprest J. Successful patching of iatrogenic rupture of the fetal membranes. Placenta. 2004; 25:352–356.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Critical Appraisal of Systematic Review/Meta-analysis
- Systematic Review and Meta-Analysis of Studies Evaluating Diagnostic Test Accuracy: A Practical Review for Clinical Researchers-Part I. General Guidance and Tips
- Systematic review for new health technology assessment
- An introduction to systematic review
- Guidelines for the Treatment of Osteoarthritis of the Knee