J Menopausal Med.
2018 Aug;24(2):108-112. 10.6118/jmm.2018.24.2.108.
Comparison of Anogenital Distance and Correlation with Vulvo-vaginal Atrophy: A Pilot Study on Premenopausal and Postmenopausal Women
- Affiliations
-
- 1Department of Gynecological and Obstetric Sciences, and Urological Sciences, University “Sapienza†of Rome, Rome, Italy. lavinia.domenici@uniroma1.it
- KMID: 2419619
- DOI: http://doi.org/10.6118/jmm.2018.24.2.108
Abstract
OBJECTIVES
Anogenital distance (AGD) represents the space between labia posterior commissure and anus. This was pilot study to investigate how menopause and so lack of oestrogens affects AGD.
METHODS
A total of 109 patients were enrolled. AGD was measured in lithotomy position using sterile paper ruler. Anogenital index (AGI) was used to control 2 variables of height and weight (body mass index, kg/m2). Vaginal health index (VHI) was used to evaluate vaginal wellness. Female sexual function index (FSFI) questionnaire was administered to all women to evaluate the impact of menopause on their sexual function.
RESULTS
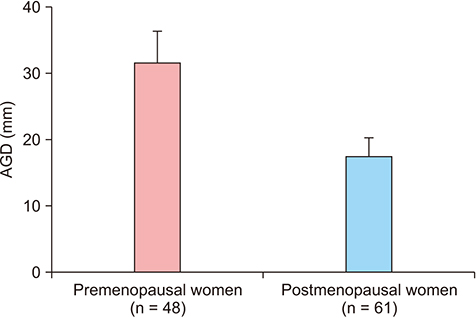
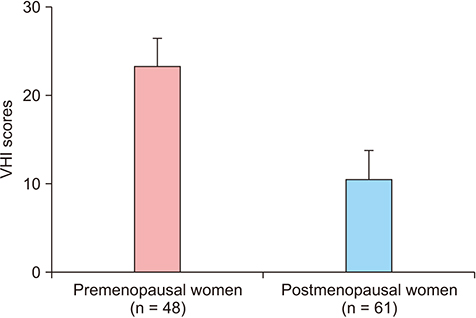
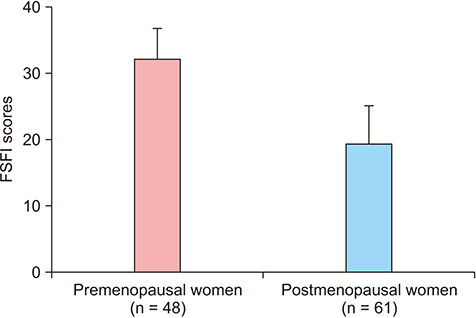
AGD (30.87 ± 2.98 vs. 17.57 ± 2.18; P = 0.0001) and AGI (1.40 ± 0.21 vs. 0.70 ± 0.15; P = 0.0001) were both significantly lower in the postmenopausal group. Postmenopausal women were affected by vulvovaginal atrophy (VVA) significantly. Thus, VHI scores were dramatically worse in postmenopausal group (23.95 ± 1.28 vs. 10.75 ± 3.41; P = 0.0001) as well as FSFI results (32.68 ± 2.25 vs. 19.78 ± 5.46; P = 0.0001).
CONCLUSIONS
This study confirms that AGD in post-menopausal women was significantly shorter than AGD in premenopausal women, correlating with an increase of VVA and sexual impairment. Changes of AGD and AGI demonstrated to predict hormonal changes that may occur after menopause.
Keyword
Figure
Reference
-
1. Mendiola J, Roca M, Mínguez-Alarcón L, Mira-Escolano MP, López-Espín JJ, Barrett ES, et al. Anogenital distance is related to ovarian follicular number in young Spanish women: a cross-sectional study. Environ Health. 2012; 11:90.
Article2. Basaran M, Kosif R, Bayar U, Civelek B. Characteristics of external genitalia in pre- and postmenopausal women. Climacteric. 2008; 11:416–421.
Article3. Dean A, Sharpe RM. Clinical review: anogenital distance or digit length ratio as measures of fetal androgen exposure: relationship to male reproductive development and its disorders. J Clin Endocrinol Metab. 2013; 98:2230–2238.4. Barrett ES, Parlett LE, Redmon JB, Swan SH. Evidence for sexually dimorphic associations between maternal characteristics and anogenital distance, a marker of reproductive development. Am J Epidemiol. 2014; 179:57–66.
Article5. Swan SH, Sathyanarayana S, Barrett ES, Janssen S, Liu F, Nguyen RH, et al. First trimester phthalate exposure and anogenital distance in newborns. Hum Reprod. 2015; 30:963–972.
Article6. Courant F, Antignac JP, Maume D, Monteau F, Andersson AM, Skakkebaek N, et al. Exposure assessment of prepubertal children to steroid endocrine disrupters 1. Analytical strategy for estrogens measurement in plasma at ultratrace level. Anal Chim Acta. 2007; 586:105–114.7. Barrett ES, Parlett LE, Sathyanarayana S, Liu F, Redmon JB, Wang C, et al. Prenatal exposure to stressful life events is associated with masculinized anogenital distance (AGD) in female infants. Physiol Behav. 2013; 114-115:14–20.
Article8. Nappi RE, Palacios S, Particco M, Panay N. The REVIVE (REal Women's VIews of Treatment Options for Menopausal Vaginal ChangEs) survey in Europe: country-specific comparisons of postmenopausal women's perceptions, experiences and needs. Maturitas. 2016; 91:81–90.
Article9. Nappi RE, Particco M, Biglia N, Cagnacci A, Di Carlo C, Luisi S, et al. Attitudes and perceptions towards vulvar and vaginal atrophy in Italian post-menopausal women: evidence from the European REVIVE survey. Maturitas. 2016; 91:74–80.
Article10. Bachmann G. Urogenital ageing: an old problem newly recognized. Maturitas. 1995; 22:Suppl. S1–S5.
Article11. Lee D, Kim TH, Lee HH, Kim JM, Jeon DS, Kim YS. A pilot study of the impacts of menopause on the anogenital distance. J Menopausal Med. 2015; 21:41–46.
Article12. Meston CM. Validation of the female sexual function index (FSFI) in women with female orgasmic disorder and in women with hypoactive sexual desire disorder. J Sex Marital Ther. 2003; 29:39–46.
Article13. Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005; 31:1–20.
Article14. Welsh M, Saunders PT, Fisken M, Scott HM, Hutchison GR, Smith LB, et al. Identification in rats of a programming window for reproductive tract masculinization, disruption of which leads to hypospadias and cryptorchidism. J Clin Invest. 2008; 118:1479–1490.
Article15. Parks LG, Ostby JS, Lambright CR, Abbott BD, Klinefelter GR, Barlow NJ, et al. The plasticizer diethylhexyl phthalate induces malformations by decreasing fetal testosterone synthesis during sexual differentiation in the male rat. Toxicol Sci. 2000; 58:339–349.
Article16. Gray LE Jr, Wilson VS, Stoker T, Lambright C, Furr J, Noriega N, et al. Adverse effects of environmental antiandrogens and androgens on reproductive development in mammals. Int J Androl. 2006; 29:96–104. discussion 5-8.17. Salazar-Martinez E, Romano-Riquer P, Yanez-Marquez E, Longnecker MP, Hernandez-Avila M. Anogenital distance in human male and female newborns: a descriptive, cross-sectional study. Environ Health. 2004; 3:8.
Article18. Wilson VS, Blystone CR, Hotchkiss AK, Rider CV, Gray LE Jr. Diverse mechanisms of anti-androgen action: impact on male rat reproductive tract development. Int J Androl. 2008; 31:178–187.
Article19. Mendiola J, Stahlhut RW, Jorgensen N, Liu F, Swan SH. Shorter anogenital distance predicts poorer semen quality in young men in Rochester, New York. Environ Health Perspect. 2011; 119:958–963.
Article20. Pasterski V, Acerini CL, Dunger DB, Ong KK, Hughes IA, Thankamony A, et al. Postnatal penile growth concurrent with mini-puberty predicts later sex-typed play behavior: evidence for neurobehavioral effects of the postnatal androgen surge in typically developing boys. Horm Behav. 2015; 69:98–105.
Article21. Thankamony A, Lek N, Carroll D, Williams M, Dunger DB, Acerini CL, et al. Anogenital distance and penile length in infants with hypospadias or cryptorchidism: comparison with normative data. Environ Health Perspect. 2014; 122:207–211.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Pilot Study of the Impacts of Menopause on the Anogenital Distance
- Changes in Atrophic Symptoms, the Vaginal Maturation Index, and Vaginal pH in Postmenopausal Women Treated with Vaginal Estrogen Tablets
- Urodynamic Characterization of Postmenopausal Women with Stress Urinary Incontinence: Retrospective Study in Incontinent Pre- and Post-menopausal Women
- Factors Affecting Bone Mineral Density in Korean Women by Menopause
- Comparison of Bone Mineral Density and Lipid Profiles in Pre and Postmenopausal Women