Yonsei Med J.
2018 Mar;59(2):303-309. 10.3349/ymj.2018.59.2.303.
Digital Videoscopic Retrograde Intrarenal Surgeries for Renal Stones: Time-to-Maximal Stone Length Ratio Analysis
- Affiliations
-
- 1Department of Urology, Severance Hospital, Urological Science Institute, Yonsei University College of Medicine, Seoul, Korea. joouro@yuhs.ac
- 2Department of Urology, Inha University School of Medicine, Incheon, Korea.
- KMID: 2418795
- DOI: http://doi.org/10.3349/ymj.2018.59.2.303
Abstract
- PURPOSE
To investigate 100 consecutive cases of videoscopic retrograde intrarenal surgery (RIRS) by a single surgeon and to evaluate factors associated with stone-free status and the learning curve thereof.
MATERIALS AND METHODS
We analyzed the results of videoscopic RIRS in 100 patients who underwent primary treatment for renal stones from January 2015 to August 2016. Videoscopic RIRS were performed with URF-V and URF-V2 flexible video uteroscopes (Olympus) or a Flex-Xc flexible ureterorenoscope (KARL STORZ). Non-contrast computed tomography was taken at 3 months postoperatively to confirm the absence of stones. The stone characteristics included the location, maximal stone length (MSL), stone heterogeneity index (SHI), and mean stone density (MSD). Fragmentation efficacy was calculated as operative time (min) divided by removed MSL (mm), and was evaluated in the sequential order of operations.
RESULTS
The mean age of the total patient was 60.0±14.0 years. The mean MSL was 13.1±6.2 mm. The average MSD was 734.2±327.6 Hounsfield unit (HU) and the SHI was 241.0±120.0 HU. The mean operation time was 65.1±45.7 min considering each renal unit. The stone-free rate at 3 months post-surgery was 87%. The estimated cut-off of the time-to-MSL ratio below 5 min/mm was 50. Multivariate analyses indicated a lower MSD [odds ratio (OR): 0.998; 95% confidence interval (CI): 0.996-0.999; p=0.047) and the last 50 cases (OR: 5.408, 95% CI: 1.337-30.426; p=0.030) as independent predictors of stone-free status after videoscopic RIRS.
CONCLUSION
Low MSDs and the last 50 cases were significant predictors of stone-free rate in videoscopic RIRS.
Keyword
MeSH Terms
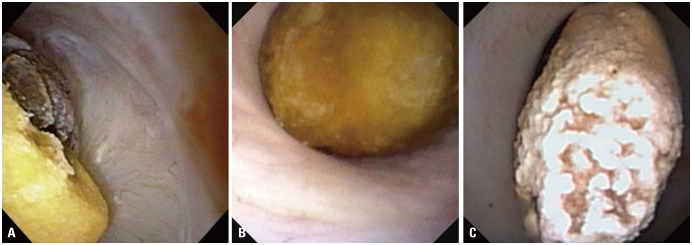
Figure
Reference
-
1. Kang DH, Cho KS, Ham WS, Chung DY, Kwon JK, Choi YD, et al. Ureteral stenting can be a negative predictor for successful outcome following shock wave lithotripsy in patients with ureteral stones. Investig Clin Urol. 2016; 57:408–416.
Article2. Teichman JM. Clinical practice. Acute renal colic from ureteral calculus. N Engl J Med. 2004; 350:684–693. PMID: 14960744.3. Kang SK, Cho KS, Kang DH, Jung HD, Kwon JK, Lee JY. Systematic review and meta-analysis to compare success rates of retrograde intrarenal surgery versus percutaneous nephrolithotomy for renal stones >2 cm: an update. Medicine. 2017; 96:e9119. PMID: 29245347.4. Xu Y, Min Z, Wan SP, Nie H, Duan G. Complications of retrograde intrarenal surgery classified by the modified Clavien grading system. Urolithiasis. 2017; DOI: 10.1007/s00240-017-0961-6.
Article5. Chang KD, Lee JY, Park SY, Kang DH, Lee HH, Cho KS. Impact of pretreatment hydronephrosis on the success rate of shock wave lithotripsy in patients with ureteral stone. Yonsei Med J. 2017; 58:1000–1005. PMID: 28792145.
Article6. Dale J, Kaplan AG, Radvak D, Shin R, Ackerman A, Chen T, et al. Evaluation of a novel single-use flexible ureteroscope. J Endourol. 2017; [Epub]. DOI: 10.1089/end.2016.0237.7. Zilberman DE, Lipkin ME, Ferrandino MN, Simmons WN, Mancini JG, Raymundo ME, et al. The digital flexible ureteroscope: in vitro assessment of optical characteristics. J Endourol. 2011; 25:519–522. PMID: 21361823.
Article8. Multescu R, Geavlete B, Georgescu D, Geavlete P. Improved durability of flex-Xc digital flexible ureteroscope: how long can you expect it to last? Urology. 2014; 84:32–35. PMID: 24703462.
Article9. Sakamoto S. Editorial Comment to Retrograde flexible ureteroscopic approach of upper urinary tract pathology: what is the status in 2014? Int J Urol. 2014; 21:1085. PMID: 25348712.
Article10. Chung DY, Cho KS, Lee DH, Han JH, Kang DH, Jung HD, et al. Impact of colic pain as a significant factor for predicting the stone free rate of one-session shock wave lithotripsy for treating ureter stones: a Bayesian logistic regression model analysis. PLoS One. 2015; 10:e0123800. PMID: 25902059.
Article11. Lee JY, Kim JH, Kang DH, Chung DY, Lee DH, Jung HD, et al. Stone heterogeneity index as the standard deviation of Hounsfield units: A novel predictor for shock-wave lithotripsy outcomes in ureter calculi. Sci Rep. 2016; 6:23988. PMID: 27035621.
Article12. Rizvi SAH, Hussain M, Askari SH, Hashmi A, Lal M, Zafar MN. Surgical outcomes of percutaneous nephrolithotomy in 3402 patients and results of stone analysis in 1559 patients. BJU Int. 2017; 120:702–709. PMID: 28303631.
Article13. Ramón de, García-Tello A, Andrés G, Redondo C, Meilán E, Gimbernat H, et al. Comparative study of retrograde intrarenal surgery and micropercutaneous nephrolithotomy in the treatment of intermediate-sized kidney stones. Actas Urol Esp. 2014; 38:576–583. PMID: 24934458.14. Gao X, Peng Y, Shi X, Li L, Zhou T, Xu B, et al. Safety and efficacy of retrograde intrarenal surgery for renal stones in patients with a solitary kidney: a single-center experience. J Endourol. 2014; 28:1290–1294. PMID: 24892920.
Article15. Baş O, Tuygun C, Dede O, Sarı S, Çakıcı MÇ, Öztürk U, et al. Factors affecting complication rates of retrograde flexible ureterorenoscopy: analysis of 1571 procedures-a single-center experience. World J Urol. 2017; 35:819–826. PMID: 27604373.
Article16. Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016; 69:475–482. PMID: 26344917.
Article17. Binbay M, Yuruk E, Akman T, Ozgor F, Seyrek M, Ozkuvanci U, et al. Is there a difference in outcomes between digital and fiberoptic flexible ureterorenoscopy procedures? J Endourol. 2010; 24:1929–1934. PMID: 21043835.
Article18. Somani BK, Al-Qahtani SM, de Medina SD, Traxer O. Outcomes of flexible ureterorenoscopy and laser fragmentation for renal stones: comparison between digital and conventional ureteroscope. Urology. 2013; 82:1017–1019. PMID: 24001703.
Article19. Cho SY, Choo MS, Jung JH, Jeong CW, Oh S, Lee SB, et al. Cumulative sum analysis for experiences of a single-session retrograde intrarenal stone surgery and analysis of predictors for stone-free status. PLoS One. 2014; 9:e84878. PMID: 24454757.
Article20. Cho KS, Jung HD, Ham WS, Chung DY, Kang YJ, Jang WS, et al. Optimal skin-to-stone distance is a positive predictor for successful outcomes in upper ureter calculi following extracorporeal shock wave lithotripsy: a Bayesian model averaging approach. PLoS One. 2015; 10:e0144912. PMID: 26659086.
Article21. Abdelhamid M, Mosharafa AA, Ibrahim H, Selim HM, Hamed M, Elghoneimy MN, et al. A prospective evaluation of high-resolution CT parameters in predicting extracorporeal shockwave lithotripsy success for upper urinary tract calculi. J Endourol. 2016; 30:1227–1232. PMID: 27597174.
Article22. Assimos D, Crisci A, Culkin D, Xue W, Roelofs A, Duvdevani M, et al. Preoperative JJ stent placement in ureteric and renal stone treatment: results from the Clinical Research Office of Endourological Society (CROES) Ureteroscopy (URS) Global Study. BJU Int. 2016; 117:648–654. PMID: 26237735.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment Outcomes of Retrograde Intrarenal Surgery for Renal Stones and Predictive Factors of Stone-Free
- A case of cystinuria with a heterozygous SLC3A1 mutation presenting with recurrent multiple renal stones in a 14-year-old boy
- Retrograde intrarenal surgery: Past, present, and future
- Efficacy of the Retrograde Intrarenal Surgery in Renal Stone: An Initial Clinical Experience
- The Efficacy of Retrograde Intrarenal Surgery (RIRS) in the Management of Renal Stone Disease