Korean J Radiol.
2018 Oct;19(5):838-848. 10.3348/kjr.2018.19.5.838.
Consensus Statements by Korean Society of Interventional Neuroradiology and Korean Stroke Society: Hyperacute Endovascular Treatment Workflow to Reduce Door-to-Reperfusion Time
- Affiliations
-
- 1Department of Neurology, Dong-A University Hospital, Busan 49201, Korea.
- 2Department of Radiology, Korea University Anam Hospital, Seoul 02841, Korea.
- 3Department of Radiology, Seoul National University Bundang Hospital, Seongnam 13620, Korea.
- 4Department of Neurology, Yonsei University Severance Hospital, Seoul 03722, Korea.
- 5Department of Neurology, Ajou University School of Medicine, Suwon 16499, Korea.
- 6Department of Radiology, Inje Univeristy Ilsan Paik Hospital, Goyang 10380, Korea.
- 7Department of Radiology, Chung-Ang University Hospital, Seoul 06973, Korea.
- 8Department of Neurology, Sungkyunkwan University, Samsung Medical Center, Seoul 06351, Korea.
- 9Department of Radiology, Pusan National University Yangsan Hospital, Yangsan 50612, Korea.
- 10Department of Radiology, Yonsei University Severance Hospital, Seoul 03722, Korea. bmoon21@hanmail.net
- 11Department of Neurology, Inha University Hospital, Incheon 22332, Korea. jhrha@inha.ac.kr
- KMID: 2418546
- DOI: http://doi.org/10.3348/kjr.2018.19.5.838
Abstract
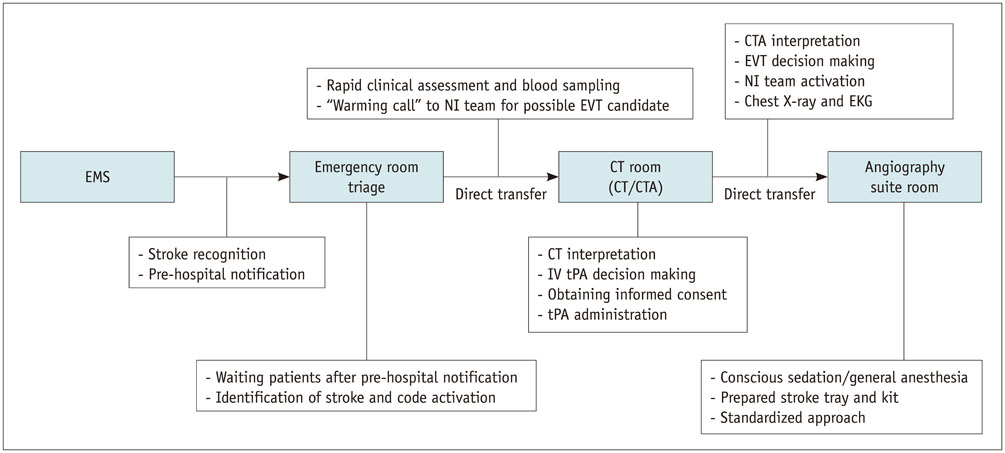
- Recent clinical trials demonstrated the clinical benefit of endovascular treatment (EVT) in patients with acute ischemic stroke due to large vessel occlusion. These trials confirmed that good outcome after EVT depends on the time interval from symptom onset to reperfusion and that in-hospital delay leads to poor clinical outcome. However, there has been no universally accepted in-hospital workflow and performance benchmark for rapid reperfusion. Additionally, wide variety in workflow for EVT is present between each stroke centers. In this consensus statement, Korean Society of Interventional Neuroradiology and Korean Stroke Society Joint Task Force Team propose a standard workflow to reduce door-to-reperfusion time for stroke patients eligible for EVT. This includes early stroke identification and pre-hospital notification to stroke team of receiving hospital in pre-hospital phase, the transfer of stroke patients from door of the emergency department to computed tomography (CT) room, warming call to neurointervention (NI) team for EVT candidate prior to imaging, NI team preparation in parallel with thrombolysis, direct transportation from CT room to angiography suite following immediate decision of EVT and standardized procedure for rapid reperfusion. Implementation of optimized workflow will improve stroke time process metrics and clinical outcome of the patient treated with EVT.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Factors Contributing to an Efficacious Endovascular Treatment for Acute Ischemic Stroke in Asian Population
Jin Soo Lee, Yang-Ha Hwang, Sung-Il Sohn
Neurointervention. 2021;16(2):91-110. doi: 10.5469/neuroint.2020.00339.The effectiveness of systemic and endovascular intra-arterial thrombectomy protocol for decreasing door-to-recanalization time duration
Su Chel Kim, Chang-Young Lee, Chang-Hyun Kim, Sung-Il Sohn, Jeong-Ho Hong, Hyungjong Park
J Cerebrovasc Endovasc Neurosurg. 2022;24(1):24-35. doi: 10.7461/jcen.2021.E2021.07.009.
Reference
-
1. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016; 316:1279–1288.
Article2. Aghaebrahim A, Streib C, Rangaraju S, Kenmuir CL, Giurgiutiu DV, Horev A, et al. Streamlining door to recanalization processes in endovascular stroke therapy. J Neurointerv Surg. 2017; 9:340–345.
Article3. Mehta BP, Leslie-Mazwi TM, Chandra RV, Bell DL, Sun CH, Hirsch JA, et al. Reducing door-to-puncture times for intra-arterial stroke therapy: a pilot quality improvement project. J Am Heart Assoc. 2014; 3:e000963.
Article4. Brandler ES, Sharma M, Sinert RH, Levine SR. Prehospital stroke scales in urban environments: a systematic review. Neurology. 2014; 82:2241–2249.
Article5. Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke. 2000; 31:71–76.6. Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati prehospital stroke scale: reproducibility and validity. Ann Emerg Med. 1999; 33:373–378.
Article7. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44:870–947.8. Choi B, Tsai D, McGillivray CG, Amedee C, Sarafin JA, Silver B. Hospital-directed feedback to emergency medical services improves prehospital performance. Stroke. 2014; 45:2137–2140.
Article9. Wojner-Alexandrov AW, Alexandrov AV, Rodriguez D, Persse D, Grotta JC. Houston paramedic and emergency stroke treatment and outcomes study (HOPST). Stroke. 2005; 36:1512–1518.10. Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes. 2012; 5:514–522.
Article11. Patel MD, Rose KM, O'Brien EC, Rosamond WD. Prehospital notification by emergency medical services reduces delays in stroke evaluation: findings from the North Carolina stroke care collaborative. Stroke. 2011; 42:2263–2268.12. Kim DH, Nah HW, Park HS, Choi JH, Kang MJ, Huh JT, et al. Impact of prehospital intervention on delay time to thrombolytic therapy in a stroke center with a systemized stroke code program. J Stroke Cerebrovasc Dis. 2016; 25:1665–1670.
Article13. Nam HS, Park E, Heo JH. Facilitating stroke management using modern information technology. J Stroke. 2013; 15:135–143.
Article14. Kim SK, Lee SY, Bae HJ, Lee YS, Kim SY, Kang MJ, et al. Pre-hospital notification reduced the door-to-needle time for IV t-PA in acute ischaemic stroke. Eur J Neurol. 2009; 16:1331–1335.
Article15. Lin CB, Peterson ED, Smith EE, Saver JL, Liang L, Xian Y, et al. Patterns, predictors, variations, and temporal trends in emergency medical service hospital prenotification for acute ischemic stroke. J Am Heart Assoc. 2012; 1:e002345.
Article16. Hong KS, Bang OY, Kim JS, Heo JH, Yu KH, Bae HJ, et al. Stroke statistics in Korea: part II stroke awareness and acute stroke care, a report from the Korean Stroke Society and Clinical Research Center for Stroke. J Stroke. 2013; 15:67–77.
Article17. Heo JH, Kim YD, Nam HS, Hong KS, Ahn SH, Cho HJ, et al. A computerized in-hospital alert system for thrombolysis in acute stroke. Stroke. 2010; 41:1978–1983.
Article18. Kansagra AP, Meyers GC, Kruzich MS, Cross DT 3rd, Moran CJ. Wide variability in prethrombectomy workflow practices in the united states: a multicenter survey. AJNR Am J Neuroradiol. 2017; 38:2238–2242.
Article19. Heldner MR, Zubler C, Mattle HP, Schroth G, Weck A, Mono ML, et al. National institutes of health stroke scale score and vessel occlusion in 2152 patients with acute ischemic stroke. Stroke. 2013; 44:1153–1157.
Article20. Rajajee V, Kidwell C, Starkman S, Ovbiagele B, Alger JR, Villablanca P, et al. Early MRI and outcomes of untreated patients with mild or improving ischemic stroke. Neurology. 2006; 67:980–984.
Article21. Wang H, Thevathasan A, Dowling R, Bush S, Mitchell P, Yan B. Streamlining workflow for endovascular mechanical thrombectomy: lessons learned from a comprehensive stroke center. J Stroke Cerebrovasc Dis. 2017; 26:1655–1662.
Article22. Schrock JW, Lum M. Drill down analysis of door-to-needle time of acute ischemic stroke patients treated with intravenous tissue plasminogen activator. Am J Emerg Med. 2014; 32:1330–1333.
Article23. Zerna C, Assis Z, d'Esterre CD, Menon BK, Goyal M. Imaging, intervention, and workflow in acute ischemic stroke: the calgary approach. AJNR Am J Neuroradiol. 2016; 37:978–984.
Article24. Goyal M, Menon BK, Hill MD, Demchuk A. Consistently achieving computed tomography to endovascular recanalization <90 minutes: solutions and innovations. Stroke. 2014; 45:e252–e256.
Article25. Lev MH, Farkas J, Rodriguez VR, Schwamm LH, Hunter GJ, Putman CM, et al. Ct angiography in the rapid triage of patients with hyperacute stroke to intraarterial thrombolysis: accuracy in the detection of large vessel thrombus. J Comput Assist Tomogr. 2001; 25:520–528.
Article26. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46:3020–3035.27. Casaubon LK, Boulanger JM, Blacquiere D, Boucher S, Brown K, Goddard T, et al. Canadian stroke best practice recommendations: hyperacute stroke care guidelines, update 2015. Int J Stroke. 2015; 10:924–940.
Article28. Lee JS, Demchuk AM. Choosing a hyperacute stroke imaging protocol for proper patient selection and time efficient endovascular treatment: lessons from recent trials. J Stroke. 2015; 17:221–228.
Article29. Brinjikji W, Demchuk AM, Murad MH, Rabinstein AA, McDonald RJ, McDonald JS, et al. Neurons over nephrons: systematic review and meta-analysis of contrast-induced nephropathy in patients with acute stroke. Stroke. 2017; 48:1862–1868.
Article30. Sharma J, Nanda A, Jung RS, Mehta S, Pooria J, Hsu DP. Risk of contrast-induced nephropathy in patients undergoing endovascular treatment of acute ischemic stroke. J Neurointerv Surg. 2013; 5:543–545.
Article31. Tu JV, Willison DJ, Silver FL, Fang J, Richards JA, Laupacis A, et al. Impracticability of informed consent in the Registry of the Canadian Stroke Network. N Engl J Med. 2004; 350:1414–1421.
Article32. Korean law for emergency medical services. Web site. Updated 2017. Accessed January 15, 2018. http://www.law.go.kr/lsInfoP.do?lsiSeq=199337&efYd=20171203#0000.33. Ribo M, Molina CA, Cobo E, Cerda N, Tomasello A, Quesada H, et al. Association between time to reperfusion and outcome is primarily driven by the time from imaging to reperfusion. Stroke. 2016; 47:999–1004.34. Sun CH, Nogueira RG, Glenn BA, Connelly K, Zimmermann S, Anda K, et al. “Picture to puncture”: a novel time metric to enhance outcomes in patients transferred for endovascular reperfusion in acute ischemic stroke. Circulation. 2013; 127:1139–1148.35. Menon BK, Sajobi TT, Zhang Y, Rempel JL, Shuaib A, Thornton J, et al. Analysis of workflow and time to treatment on thrombectomy outcome in the endovascular treatment for small core and proximal occlusion ischemic stroke (ESCAPE) randomized, controlled trial. Circulation. 2016; 133:2279–2286.
Article36. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.37. Menon BK, Almekhlafi MA, Pereira VM, Gralla J, Bonafe A, Davalos A, et al. Optimal workflow and process-based performance measures for endovascular therapy in acute ischemic stroke: analysis of the solitaire FR thrombectomy for acute revascularization study. Stroke. 2014; 45:2024–2029.38. Qureshi AI, Egila H, Adil MM, Siddiqi H, Mian N, Hassan AE, et al. “No turn back approach” to reduce treatment time for endovascular treatment of acute ischemic stroke. J Stroke Cerebrovasc Dis. 2014; 23:e317–e323.
Article39. Menon BK, Demchuk AM. Computed tomography angiography in the assessment of patients with stroke/TIA. Neurohospitalist. 2011; 1:187–199.
Article40. Frei D, McGraw C, McCarthy K, Whaley M, Bellon RJ, Loy D, et al. A standardized neurointerventional thrombectomy protocol leads to faster recanalization times. J Neurointerv Surg. 2017; 9:1035–1040.
Article41. Leifer D, Bravata DM, Connors JJ 3rd, Hinchey JA, Jauch EC, Johnston SC, et al. Metrics for measuring quality of care in comprehensive stroke centers: detailed follow-up to brain attack coalition comprehensive stroke center recommendations: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; 42:849–877.
Article42. Almekhlafi MA, Hockley A, Desai JA, Nambiar V, Mishra S, Volny O, et al. Overcoming the evening/weekend effects on time delays and outcomes of endovascular stroke therapy: the Calgary Stroke Program experience. J Neurointerv Surg. 2014; 6:729–732.
Article43. Rai AT, Smith MS, Boo S, Tarabishy AR, Hobbs GR, Carpenter JS. The ‘pit-crew’ model for improving door-to-needle times in endovascular stroke therapy: a Six-Sigma project. J Neurointerv Surg. 2016; 8:447–452.
Article44. Tai YJ, Weir L, Hand P, Davis S, Yan B. Does a ‘code stroke’ rapid access protocol decrease door-to-needle time for thrombolysis. Intern Med J. 2012; 42:1316–1324.
Article45. Barba R, Losa JE, Velasco M, Guijarro C, Garcia de Casasola G, Zapatero A. Mortality among adult patients admitted to the hospital on weekends. Eur J Intern Med. 2006; 17:322–324.
Article46. McTaggart RA, Ansari SA, Goyal M, Abruzzo TA, Albani B, Arthur AJ, et al. Initial hospital management of patients with emergent large vessel occlusion (ELVO): report of the standards and guidelines committee of the society of neurointerventional surgery. J Neurointerv Surg. 2017; 9:316–323.
Article47. Abou-Chebl A, Lin R, Hussain MS, Jovin TG, Levy EI, Liebeskind DS, et al. Conscious sedation versus general anesthesia during endovascular therapy for acute anterior circulation stroke preliminary results from a retrospective, multicenter study. Stroke. 2010; 41:1175–1179.48. Brinjikji W, Murad MH, Rabinstein AA, Cloft HJ, Lanzino G, Kallmes DF. Conscious sedation versus general anesthesia during endovascular acute ischemic stroke treatment: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2015; 36:525–529.
Article49. McDonald JS, Brinjikji W, Rabinstein AA, Cloft HJ, Lanzino G, Kallmes DF. Conscious sedation versus general anaesthesia during mechanical thrombectomy for stroke: a propensity score analysis. J Neurointerv Surg. 2015; 7:789–794.
Article50. Schönenberger S, Uhlmann L, Hacke W, Schieber S, Mundiyanapurath S, Purrucker JC, et al. Effect of conscious sedation vs general anesthesia on early neurological improvement among patients with ischemic stroke undergoing endovascular thrombectomy: a randomized clinical trial. JAMA. 2016; 316:1986–1996.51. Löwhagen Hendén P, Rentzos A, Karlsson JE, Rosengren L, Leiram B, Sundeman H, et al. General anesthesia versus conscious sedation for endovascular treatment of acute ischemic stroke: the AnStroke trial (anesthesia during stroke). Stroke. 2017; 48:1601–1607.
Article52. Schregel K, Behme D, Tsogkas I, Knauth M, Maier I, Karch A, et al. Effects of workflow optimization in endovascularly treated stroke patients - a pre-post effectiveness study. PLoS One. 2016; 11:e0169192.
Article53. Samore MH, Wessolossky MA, Lewis SM, Shubrooks SJ Jr, Karchmer AW. Frequency, risk factors, and outcome for bacteremia after percutaneous transluminal coronary angioplasty. Am J Cardiol. 1997; 79:873–877.
Article54. Culver DA, Chua J, Rehm SJ, Whitlow P, Hertzer NR. Arterial infection and staphylococcus aureus bacteremia after transfemoral cannulation for percutaneous carotid angioplasty and stenting. J Vasc Surg. 2002; 35:576–579.
Article55. Sun CH, Ribo M, Goyal M, Yoo AJ, Jovin T, Cronin CA, et al. Door-to-puncture: a practical metric for capturing and enhancing system processes associated with endovascular stroke care, preliminary results from the rapid reperfusion registry. J Am Heart Assoc. 2014; 3:e000859.
Article56. Eesa M, Menon BK, Hill MD, Demchuk A, Goyal M. Achieving faster recanalization times by IA thrombolysis in acute ischemic stroke: where should we direct our efforts? Interv Neuroradiol. 2011; 17:228–234.
Article57. Eesa M, Almekhlafi MA, Mitha AP, Wong JH, Goyal M. Manual aspiration thrombectomy through balloon-tipped guide catheter for rapid clot burden reduction in endovascular therapy for ICA L/T occlusion. Neuroradiology. 2012; 54:1261–1265.
Article58. Berkhemer OA, Fransen PS, Beumer D, van den, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.
Article59. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003; 34:e109–e137.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Consensus Statements by Korean Society of Interventional Neuroradiology and Korean Stroke Society: Hyperacute Endovascular Treatment Workflow to Reduce Door-to-Reperfusion Time
- Guideline for intra-arterial thrombolysis of hyperacute ischemic stroke patients: Preliminary Report
- Perspectives on Fellowship Training Standard in Interventional Neuroradiology
- The Comparison of Outcome between Thromboaspiration and Aggressive Mechanical Clot Disruption in Treating Hyperacute Stroke Patients
- Erratum: Susceptibility Vessel Sign in the ASTER Trial: Higher Recanalization Rate and More Favourable Clinical Outcome after First Line Stent Retriever Compared to Contact Aspiration