J Korean Ophthalmol Soc.
2018 Aug;59(8):797-801. 10.3341/jkos.2018.59.8.797.
Abducens Nerve Palsy and Optic Perineuritis Caused by Fungal Sphenoidal Sinusitis
- Affiliations
-
- 1Department of Neurosurgery, Yeungnam University College of Medicine, Daegu, Korea.
- 2Department of Pathology, Yeungnam University College of Medicine, Daegu, Korea.
- 3Department of Ophthalmology, Yeungnam University College of Medicine, Daegu, Korea. eyekwj@ynu.ac.kr
- KMID: 2418509
- DOI: http://doi.org/10.3341/jkos.2018.59.8.797
Abstract
- PURPOSE
To report a case of abducens nerve palsy and optic perineuritis caused by fungal sphenoidal sinusitis.
CASE SUMMARY
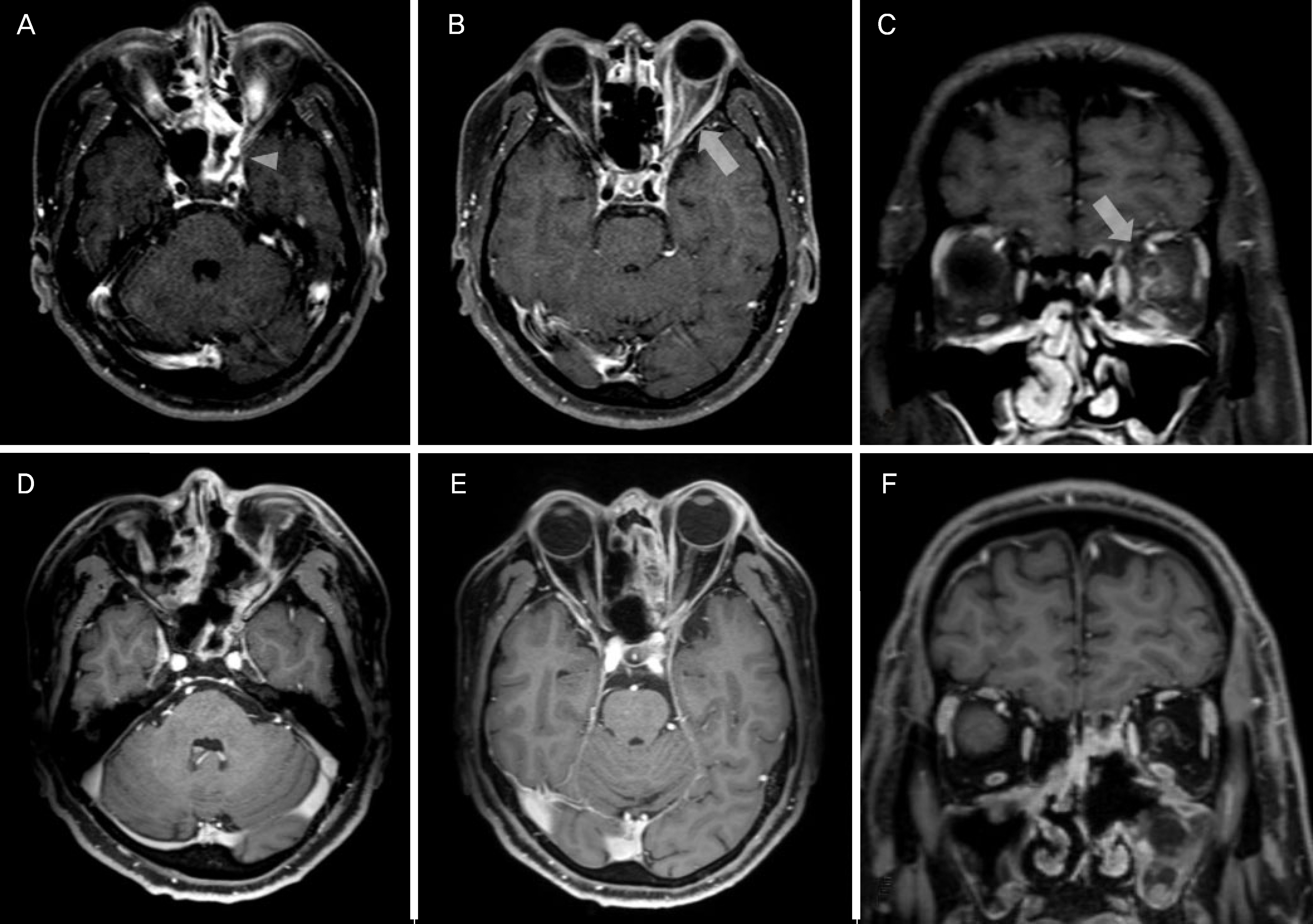
A 48-year-old male visited emergency department for retrobulbar pain, decreased vision, and horizontal diplopia for 3 days. He reported that previous medical history was non-specific, however, blood glucose level was 328 mg/dL (70-110). He had experienced severe headache for 7 days. The best corrected visual acuity was 20/20 at right eye and 20/25 at left eye. The pupil of left eye did not have relative afferent pupillary defect. Left mild proptosis was noted. The extraocular examination showed 30 prism diopters left esotropia at primary gaze and −4 abduction limitation of left eye. The left eye showed mild optic disc swelling and inferior field defect by field test. Brain magnetic resonance imaging showed enhancement of sphenoidal sinus, ethmoidal sinus, and around optic nerve at left eye. Three days after antibiotics treatment, the vision of left eye deteriorated to 20/40 and periorbital pain developed. The drainage and biopsy of sphenoidal sinus were performed. The histopathologic examination showed hyphae consistent with aspergillosis. The ocular symptoms were improved with anti-fungal treatment. Follow-up magnetic resonance imaging performed 1 month after treatment showed improvement of lesion at left orbit. Five months after surgery, the visual acuity of left eye was improved to 20/25. The patient showed orthotropia at primary gaze without limitation.
CONCLUSIONS
The abducens nerve palsy and optic perineuritis can be caused by fungal sphenoidal sinusitis. The early diagnosis and appropriate treatment can lead to favorable outcome.
MeSH Terms
-
Abducens Nerve Diseases*
Abducens Nerve*
Anti-Bacterial Agents
Aspergillosis
Biopsy
Blood Glucose
Brain
Diplopia
Drainage
Early Diagnosis
Emergency Service, Hospital
Esotropia
Ethmoid Sinus
Exophthalmos
Follow-Up Studies
Fungi
Headache
Humans
Hyphae
Magnetic Resonance Imaging
Male
Middle Aged
Optic Nerve
Orbit
Pupil
Pupil Disorders
Sphenoid Sinusitis*
Visual Acuity
Anti-Bacterial Agents
Blood Glucose
Figure
Cited by 2 articles
-
Delayed Onset Abducens Nerve Palsy and Horner Syndrome after Treatment of a Traumatic Carotid-cavernous Fistula
Won Jae Kim, Cheol Won Moon, Myung Mi Kim
J Korean Ophthalmol Soc. 2019;60(9):905-908. doi: 10.3341/jkos.2019.60.9.905.Rapid progression from trochlear nerve palsy to orbital apex syndrome as an initial presentation of advanced gastric cancer
Eunjung Kong, Sung Ae Koh, Won Jae Kim
Yeungnam Univ J Med. 2019;36(2):159-162. doi: 10.12701/yujm.2019.00129.
Reference
-
References
1. Witterick IJ, Vescan AD. Complications of rhinosinusitis. Kennedy DW, Hwang PH, editors. Rhinology. 1st ed.New York: Thieme Medical Publishers;2012. chap. 21.2. Miller NR, Subramanian PS, Patel VR. Walsh and Hoyt's Clinical Neuro-Ophthalmology: the Essentials. 3rd ed.Philadelphia: Wolters Kluwer;2016. p. 341–71.3. Chen L, Jiang L, Yang B, Subramanian PS. Clinical features of visual disturbances secondary to isolated sphenoid sinus inflammatory diseases. BMC Ophthalmol. 2017; 17:237.
Article4. Kline LB, Foroozan R. Neuro-Ophthalmology Review Manual. 7th ed.Thorofare: SLACK;2013. p. 83–92.5. Jang JH, Kim YC, Chang SD, et al. A case of optic neuritis in acute sphenoid sinusitis. J Korean Ophthalmol Soc. 2007; 48:1742–6.
Article6. Kim DH, Kim HK, Nam JK, Park JG. A case of isolated aspergillus sphenoid sinusitis. J Korean Neurol Assoc. 2005; 23:402–4.7. Lee HR, Kim HJ, Seong SY, Chang JH. A case of orbital apex syndrome related to sphenoid fungal sinusitis. Korean J Otorhinolaryngol-Head Neck Surg. 2010; 53:644–7.
Article8. Biousse V, Newman NJ. Neuro-ophthalmology Illustrated. 2nd ed.New York: Thieme;2016. p. 321–465.9. Pane A, Miller NR, Burdon M. The neuro-ophthalmology survival guide. 2nd ed.Beijing: Elsevier;2017. p. 170–239.10. Tamhankar MA, Biousse V, Ying GS, et al. Isolated third, fourth, and sixth cranial nerve palsies from presumed microvascular versus other causes: a prospective study. Ophthalmology. 2013; 120:2264–9.11. Purvin V, Kawasaki A, Jacobson DM. Optic perineuritis: clinical and radiographic features. Arch Ophthalmol. 2001; 119:1299–306.12. Lim HC, Choi HY, Choi JH, Jung JH. Clinical manifestations and treatment of idiopathic optic perineuritis. J Korean Ophthalmol Soc. 2014; 55:891–7.
Article13. Miller C, Suh JD, Henriquez OA, et al. Prognosis for sixth nerve palsy arising from paranasal sinus disease. Am J Rhinol Allergy. 2013; 27:432–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Fungal Sphenoidal Sinusitis Involving Optic Nerve
- A Case of Abducens Nerve Palsy Caused by Isolated Sphenoid Fungal Sinusitis
- Acute Rhinosinusitis in Prominently Pneumatized Sphenoid Sinus Presenting with Unilateral Abducens Nerve Palsy
- A Case of Isolated Unilateral Abducens Nerve Palsy Caused by Clival Metastasis from Rectal Cancer
- Clinical Manifestations of Idiopathic Optic Perineuritis in Korea