Cancer Res Treat.
2018 Jul;50(3):757-767. 10.4143/crt.2017.050.
Trend Analysis for the Choice and Cost of Lung Cancer Treatment in South Korea, 2003-2013
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, College of Medicine, Chungbuk National University and Chungbuk National University Hospital, Cheongju, Korea.
- 2Department of Public Health and Preventive Medicine, Chungbuk National University Hospital, Cheongju, Korea.
- 3College of Medicine/Graduate School of Health Science Business Convergence, Chungbuk National University, Cheongju, Korea. jonghyock@gmail.com
- 4Department of Family Medicine, Seoul National University Hospital, Seoul, Korea.
- KMID: 2417865
- DOI: http://doi.org/10.4143/crt.2017.050
Abstract
- PURPOSE
Our study aimed to report the annual changes in lung cancer statistics and analyze trends in sociodemographic, medical, and financial factors from 2003 to 2013 in the national database from the Korean National Health Insurance (KNHI).
MATERIALS AND METHODS
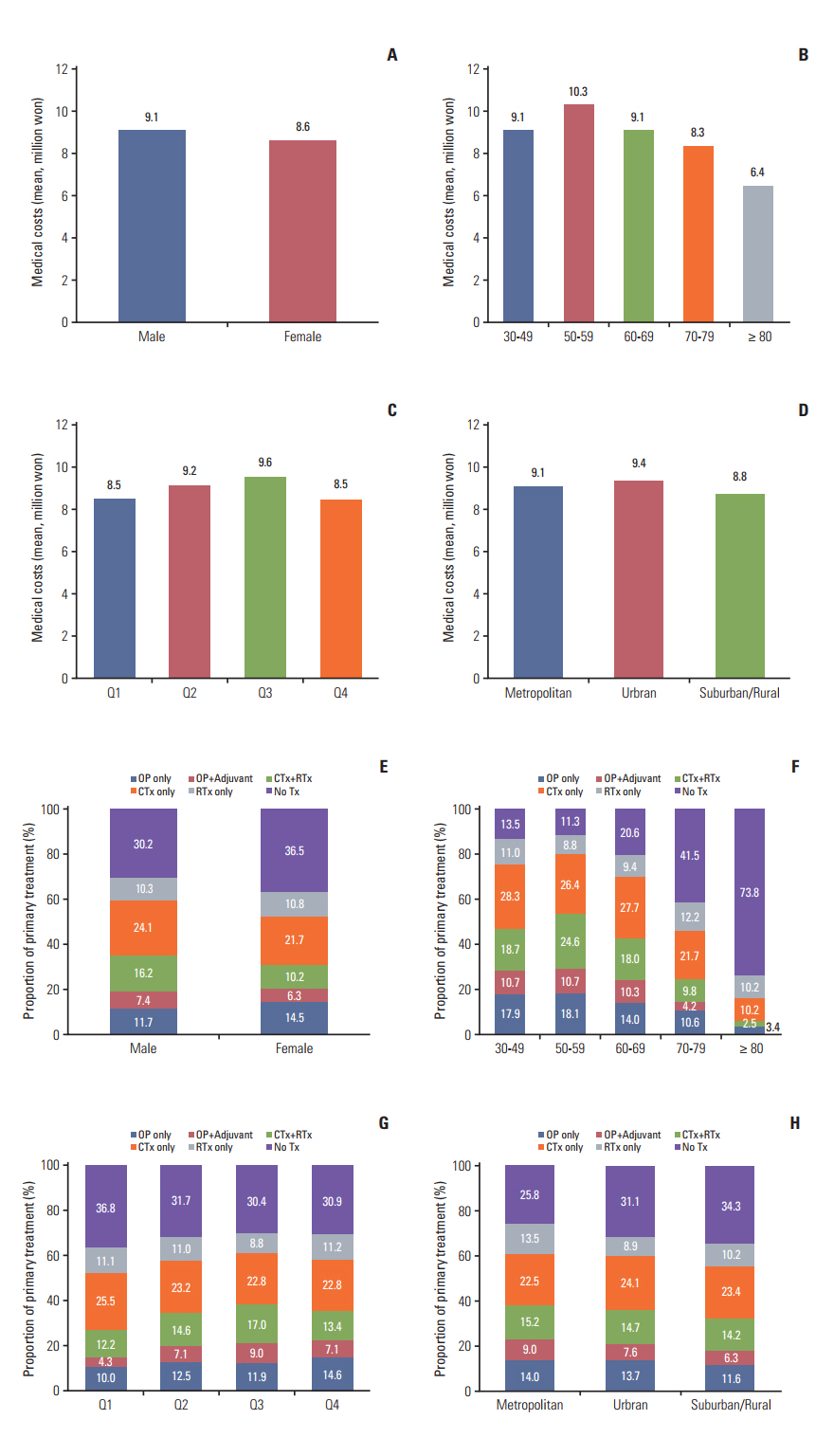
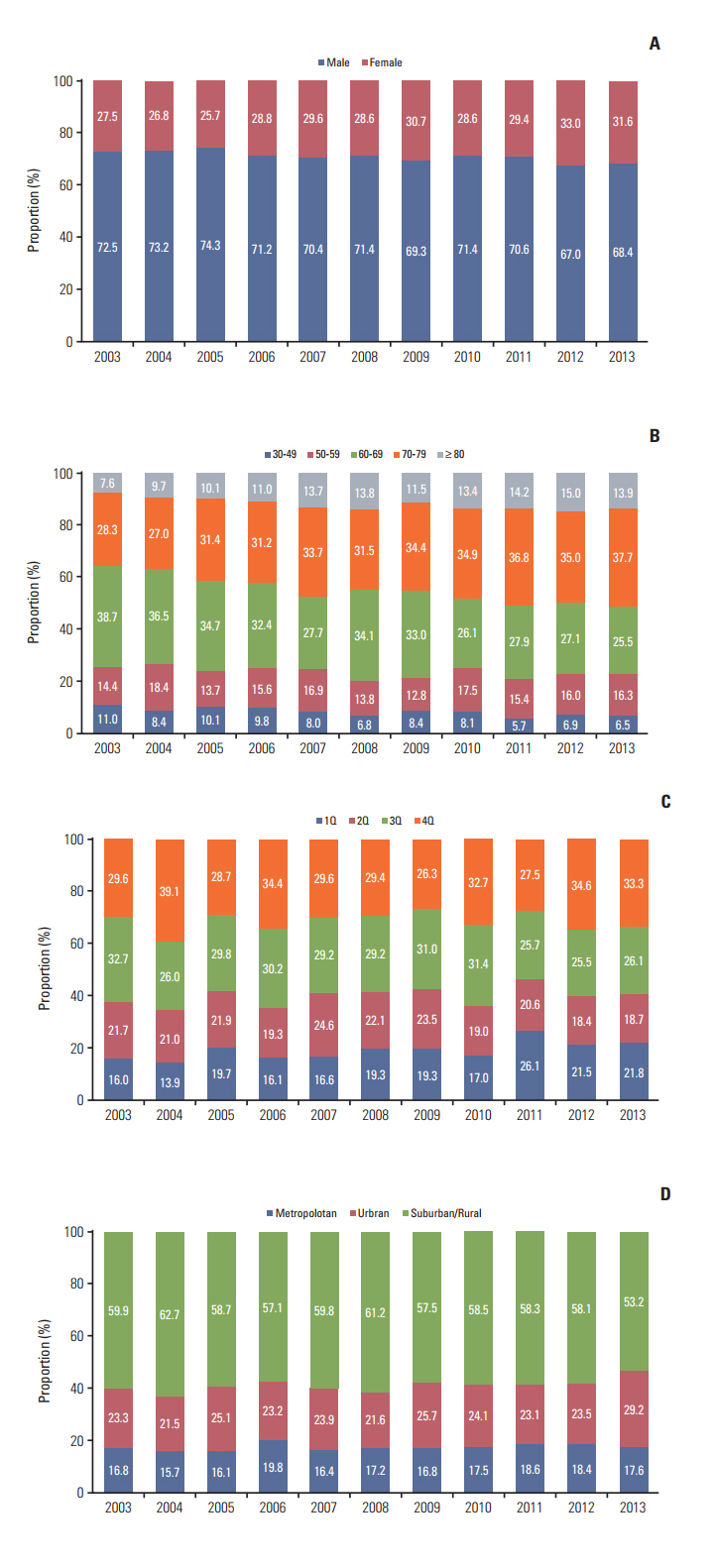
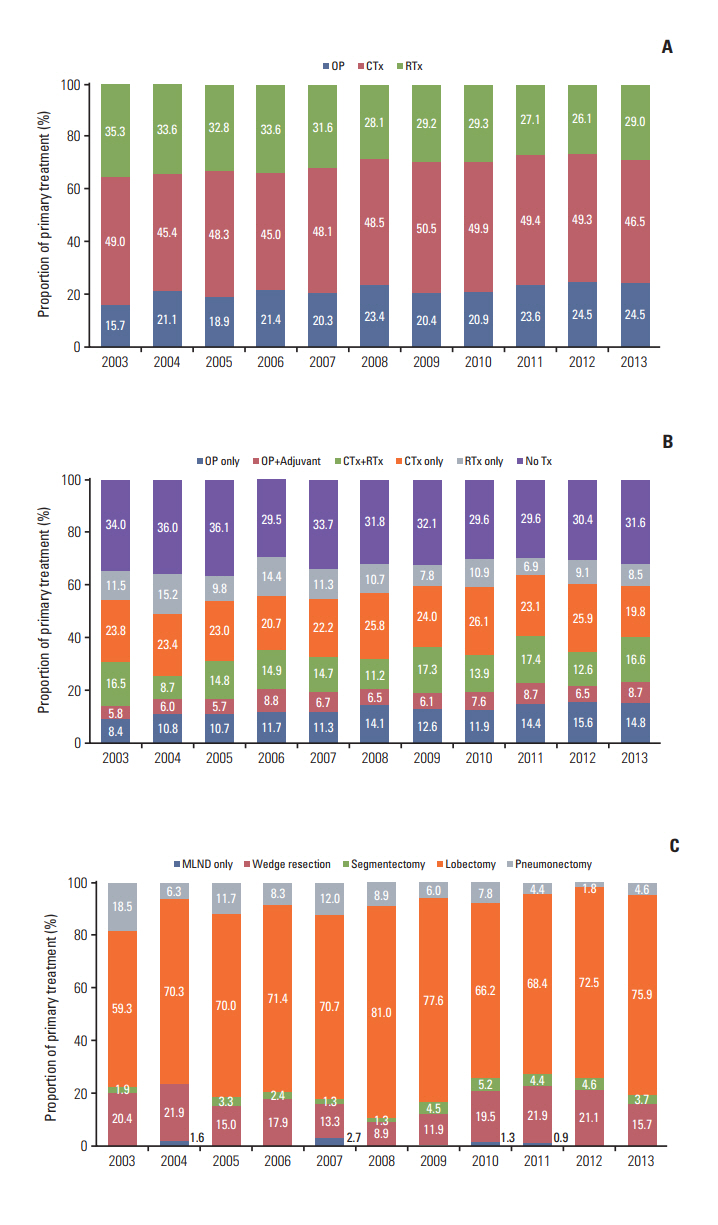
Among 7,489 patients with code C34 in KNHI database, only lung cancer patients newly diagnosed after 2003 were included in the study population, for a total of 4,582 patients. Descriptive statistics were used to characterize treatment patterns and medical costs according to sociodemographic factors.
RESULTS
Approximately 70% of subjects were male, and the mean age was 67 years. Around 46% of patients were over 70 years old, and 12% were over 80 years old. The medical costs were highest for patients younger than 60 and lowest for those over 80 years old. Surgery was more common in younger patients, while "no treatment" increased greatly with age. In trend analysis, the proportions of aging (p for trend < 0.001), female (p for trend=0.003), metropolitan/urban (p for trend=0.041), and lowest or highest-income patients (p for trend=0.004) increased over time, along with the prevalence of surgery as the primary treatment (p for trend < 0.001). There was also a trend with regard to change in medical costs (p for trend < 0.001), in that those of surgery and radiotherapy increased.
CONCLUSION
Surgery as a curative treatment has increased over the past decade. However, the elderly, suburban/rural residents, and low-income patients were more likely to be untreated. Therefore, active measures are required for these increasingly vulnerable groups.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015; 47:127–41.
Article2. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65:87–108.
Article3. Miller DL, Mayfield WR, Luu TD, Helms GA, Muster AR, Beckler VJ, et al. Community-based multidisciplinary computed tomography screening program improves lung cancer survival. Ann Thorac Surg. 2016; 101:1864–9.
Article4. Patz EF Jr, Greco E, Gatsonis C, Pinsky P, Kramer BS, Aberle DR. Lung cancer incidence and mortality in National Lung Screening Trial participants who underwent low-dose CT prevalence screening: a retrospective cohort analysis of a randomised, multicentre, diagnostic screening trial. Lancet Oncol. 2016; 17:590–9.
Article5. Islami F, Torre LA, Jemal A. Global trends of lung cancer mortality and smoking prevalence. Transl Lung Cancer Res. 2015; 4:327–38.6. Choi MS, Park JS, Kim HK, Choi YS, Kim J, Shim YM, et al. Analysis of 1,067 cases of video-assisted thoracic surgery lobectomy. Korean J Thorac Cardiovasc Surg. 2011; 44:169–77.
Article7. Ikeda N, Saji H, Hagiwara M, Ohira T, Usuda J, Kajiwara N. Recent advances in video-assisted thoracoscopic surgery for lung cancer. Asian J Endosc Surg. 2013; 6:9–13.
Article8. Salama JK, Vokes EE. New radiotherapy and chemoradiotherapy approaches for non-small-cell lung cancer. J Clin Oncol. 2013; 31:1029–38.
Article9. Chang JY, Senan S, Paul MA, Mehran RJ, Louie AV, Balter P, et al. Stereotactic ablative radiotherapy versus lobectomy for operable stage I non-small-cell lung cancer: a pooled analysis of two randomised trials. Lancet Oncol. 2015; 16:630–7.
Article10. Cheng TY, Cramb SM, Baade PD, Youlden DR, Nwogu C, Reid ME. The international epidemiology of lung cancer: latest trends, disparities, and tumor characteristics. J Thorac Oncol. 2016; 11:1653–71.
Article11. Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008-2030): a population-based study. Lancet Oncol. 2012; 13:790–801.
Article12. Jung KW, Won YJ, Oh CM, Kong HJ, Cho H, Lee JK, et al. Prediction of cancer incidence and mortality in Korea, 2016. Cancer Res Treat. 2016; 48:451–7.
Article13. Lim D, Ha M, Song I. Trends in major cancer mortality in Korea, 1983-2012, with a joinpoint analysis. Cancer Epidemiol. 2015; 39:939–46.
Article14. Gwon SH, Jeong S. Factors influencing adolescent lifetime smoking and current smoking in South Korea: using data from the 10th (2014) Korea Youth Risk Behavior Web-Based Survey. J Korean Acad Nurs. 2016; 46:552–61.15. Eckel SP, Cockburn M, Shu YH, Deng H, Lurmann FW, Liu L, et al. Air pollution affects lung cancer survival. Thorax. 2016; 71:891–8.
Article16. Chen G, Wan X, Yang G, Zou X. Traffic-related air pollution and lung cancer: a meta-analysis. Thorac Cancer. 2015; 6:307–18.
Article17. Wang A, Qin F, Hedlin H, Desai M, Chlebowski R, Gomez S, et al. Physical activity and sedentary behavior in relation to lung cancer incidence and mortality in older women: The Women's Health Initiative. Int J Cancer. 2016; 139:2178–92.
Article18. Koshy M, Fedewa SA, Malik R, Ferguson MK, Vigneswaran WT, Feldman L, et al. Improved survival associated with neoadjuvant chemoradiation in patients with clinical stage IIIA(N2) non-small-cell lung cancer. J Thorac Oncol. 2013; 8:915–22.
Article19. Kim HK, Cho JH, Choi YS, Zo JI, Shim YM, Park K, et al. Outcomes of neoadjuvant concurrent chemoradiotherapy followed by surgery for non-small-cell lung cancer with N2 disease. Lung Cancer. 2016; 96:56–62.
Article20. Herskovic A, Chitti B, Christos P, Wernicke AG, Parashar B. Addition of surgery after radiation significantly improves survival in stage IIIB non-small cell lung cancer: a populationbased analysis. World J Surg. 2017; 41:758–62.
Article21. Janet-Vendroux A, Loi M, Bobbio A, Lococo F, Lupo A, Ledinot P, et al. Which is the role of pneumonectomy in the era of parenchymal-sparing procedures? Early/long-term survival and functional results of a single-center experience. Lung. 2015; 193:965–73.
Article22. Park BJ, Flores RM, Rusch VW. Robotic assistance for videoassisted thoracic surgical lobectomy: technique and initial results. J Thorac Cardiovasc Surg. 2006; 131:54–9.
Article23. Hirsch FR, Suda K, Wiens J, Bunn PA Jr. New and emerging targeted treatments in advanced non-small-cell lung cancer. Lancet. 2016; 388:1012–24.
Article24. Shin A, Oh CM, Kim BW, Woo H, Won YJ, Lee JS. Lung cancer epidemiology in Korea. Cancer Res Treat. 2017; 49:616–26.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Quality Assessment and Trend for Breast Cancer Treatment Practice across South Korea Based on Nationwide Analysis of Korean Health Insurance Data during 2013-2017
- Time Trends for Prostate Cancer Incidence from 2003 to 2013 in South Korea: An Age-Period-Cohort Analysis
- Economic Evaluation of Gemcitabine-cisplatin Chemotherapy for Non Small-Cell Lung Cancer Patient in an Outpatient Setting
- Chemotherapy in Lung Cancer
- The Impact of Time-to-Treatment for Outcome in Cancer Patients, and Its Differences by Region and Time Trend