J Korean Med Sci.
2017 Jan;32(1):47-53. 10.3346/jkms.2017.32.1.47.
The Role of Pharmacomechanical Endovascular Intervention for Iliofemoral Vein Thrombosis Compared to Conventional Anticoagulation Therapy
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Korea University Ansan Hospital, Ansan, Korea. jowonmin@korea.ac.kr
- KMID: 2417584
- DOI: http://doi.org/10.3346/jkms.2017.32.1.47
Abstract
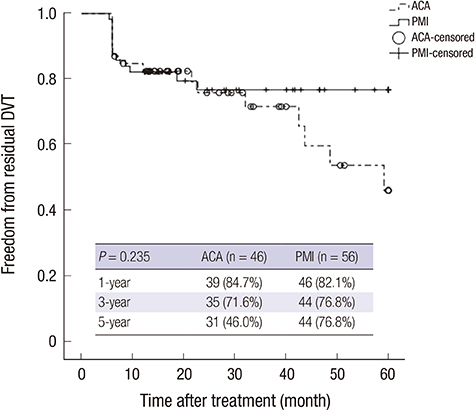
- Although anticoagulation therapy is the primary treatment for deep vein thrombosis (DVT), it has not been associated with the rapid recanalization of the venous occlusion. Moreover, it is associated with long-term disability due to post-thrombotic syndrome (PTS). In contrast, pharmacomechanical endovascular intervention (PMI) results in more rapid clinical improvement in DVT patients, but there are few reports on its long-term outcomes. This retrospective study evaluated the clinical effectiveness of PMI compared to conventional anticoagulation therapy (ACA) for acute and subacute iliofemoral DVT. We reviewed the medical records of 102 patients with iliofemoral DVT. A total of 46 patients for ACA and 56 patients for PMI were enrolled. We analyzed the clinical differences between the PMI and ACA groups by comparing the clinical signs, residual DVT free-rate, and PTS-free rate. There were no statistically significant differences in the demographic characteristics and risk factors except age between the groups (age: ACA, 52.0 ± 18.0 years; PMI, 59.0 ± 17.0 years; P = 0.035). The 1-, 3-, and 5-year residual DVT-free rate (ACA = 84.7%, 71.6%, and 46.0%; PMI = 82.1%, 76.8%, and 76.8%, respectively; P = 0.235) was not significantly different. However, the 1-, 3-, and 5-year PTS-free rate was significantly different (ACA = 93.5%, 74.0%, and 55.7%; PMI = 92.9%, 90.0%, and 90.0%, respectively; P = 0.019). There was no significant difference in the rate of other complications. PMI showed a lower incidence of PTS during the follow-up period. Therefore, PMI should be considered as an effective therapeutic modality for patients with iliofemoral DVT.
Keyword
MeSH Terms
Figure
Reference
-
1. Fowkes FJ, Price JF, Fowkes FG. Incidence of diagnosed deep vein thrombosis in the general population: systematic review. Eur J Vasc Endovasc Surg. 2003; 25:1–5.2. Kahn SR, Comerota AJ, Cushman M, Evans NS, Ginsberg JS, Goldenberg NA, Gupta DK, Prandoni P, Vedantham S, Walsh ME, American Heart Association Council on Peripheral Vascular Disease, Council on Clinical Cardiology, and Council on Cardiovascular and Stroke Nursing, et al. The postthrombotic syndrome: evidence-based prevention, diagnosis, and treatment strategies: a scientific statement from the American Heart Association. Circulation. 2014; 130:1636–1661.3. Hull RD, Raskob GE, Rosenbloom D, Lemaire J, Pineo GF, Baylis B, Ginsberg JS, Panju AA, Brill-Edwards P, Brant R. Optimal therapeutic level of heparin therapy in patients with venous thrombosis. Arch Intern Med. 1992; 152:1589–1595.4. Raschke RA, Reilly BM, Guidry JR, Fontana JR, Srinivas S. The weight-based heparin dosing nomogram compared with a “standard care” nomogram. A randomized controlled trial. Ann Intern Med. 1993; 119:874–881.5. Prandoni P, Prins MH, Lensing AW, Ghirarduzzi A, Ageno W, Imberti D, Scannapieco G, Ambrosio GB, Pesavento R, Cuppini S, AESOPUS Investigators, et al. Residual thrombosis on ultrasonography to guide the duration of anticoagulation in patients with deep venous thrombosis: a randomized trial. Ann Intern Med. 2009; 150:577–585.6. Comerota AJ, Aldridge SC. Thrombolytic therapy for deep venous thrombosis: a clinical review. Can J Surg. 1993; 36:359–364.7. Prandoni P, Frulla M, Sartor D, Concolato A, Girolami A. Vein abnormalities and the post-thrombotic syndrome. J Thromb Haemost. 2005; 3:401–402.8. Plate G, Eklöf B, Norgren L, Ohlin P, Dahlström JA. Venous thrombectomy for iliofemoral vein thrombosis--10-year results of a prospective randomised study. Eur J Vasc Endovasc Surg. 1997; 14:367–374.9. Gänger KH, Nachbur BH, Ris HB, Zurbrügg H. Surgical thrombectomy versus conservative treatment for deep venous thrombosis; functional comparison of long-term results. Eur J Vasc Surg. 1989; 3:529–538.10. Enden T, Kløw NE, Sandvik L, Slagsvold CE, Ghanima W, Hafsahl G, Holme PA, Holmen LO, Njaastad AM, Sandbaek G, CaVenT study group, et al. Catheter-directed thrombolysis vs. anticoagulant therapy alone in deep vein thrombosis: results of an open randomized, controlled trial reporting on short-term patency. J Thromb Haemost. 2009; 7:1268–1275.11. Dasari TW, Pappy R, Hennebry TA. Pharmacomechanical thrombolysis of acute and chronic symptomatic deep vein thrombosis: a systematic review of literature. Angiology. 2012; 63:138–145.12. Karthikesalingam A, Young EL, Hinchliffe RJ, Loftus IM, Thompson MM, Holt PJ. A systematic review of percutaneous mechanical thrombectomy in the treatment of deep venous thrombosis. Eur J Vasc Endovasc Surg. 2011; 41:554–565.13. Kistner RL, Eklof B, Masuda EM. Diagnosis of chronic venous disease of the lower extremities: the “CEAP” classification. Mayo Clin Proc. 1996; 71:338–345.14. Virchow R. Canton, MA: Science History Publications;1998.15. Sevitt S. Pathology and pathogenesis of deep vein thrombi. Proc R Soc Med. 1975; 68:261.16. Mannucci PM, Poller L. Venous thrombosis and anticoagulant therapy. Br J Haematol. 2001; 114:258–270.17. Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, Svensson PJ, Veenstra DL, Crowther M, Guyatt GH, et al. Evidence-based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012; 141:e152S–e184S.18. Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, Jenkins JS, Kline JA, Michaels AD, Thistlethwaite P, American Heart Association Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; American Heart Association Council on Peripheral Vascular Disease; American Heart Association Council on Arteriosclerosis, Thrombosis and Vascular Biology, et al. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011; 123:1788–1830.19. Gogalniceanu P, Johnston CJ, Khalid U, Holt PJ, Hincliffe R, Loftus IM, Thompson MM. Indications for thrombolysis in deep venous thrombosis. Eur J Vasc Endovasc Surg. 2009; 38:192–198.20. Kahn SR, Shrier I, Julian JA, Ducruet T, Arsenault L, Miron MJ, Roussin A, Desmarais S, Joyal F, Kassis J, et al. Determinants and time course of the postthrombotic syndrome after acute deep venous thrombosis. Ann Intern Med. 2008; 149:698–707.21. Kurz X, Kahn SR, Abenhaim L, Clement D, Norgren L, Baccaglini U, Berard A, Cooke JP, Cornu-Thenard A, Depairon M, et al. Chronic venous disorders of the leg: epidemiology, outcomes, diagnosis and management. Summary of an evidence-based report of the VEINES task force. Venous Insufficiency Epidemiologic and Economic Studies. Int Angiol. 1999; 18:83–102.22. Kahn SR, Hirsch A, Shrier I. Effect of postthrombotic syndrome on health-related quality of life after deep venous thrombosis. Arch Intern Med. 2002; 162:1144–1148.23. Brandjes DP, Büller HR, Heijboer H, Huisman MV, de Rijk M, Jagt H, ten Cate JW. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997; 349:759–762.24. Comerota AJ, Paolini D. Treatment of acute iliofemoral deep venous thrombosis: a strategy of thrombus removal. Eur J Vasc Endovasc Surg. 2007; 33:351–360.25. Watson LI, Armon MP. Thrombolysis for acute deep vein thrombosis. Cochrane Database Syst Rev. 2004; (4):CD002783.26. Aziz F, Comerota AJ. Quantity of residual thrombus after successful catheter-directed thrombolysis for iliofemoral deep venous thrombosis correlates with recurrence. Eur J Vasc Endovasc Surg. 2012; 44:210–213.27. Villalta S, Bagatella P, Piccioli A, Lensing AW, Prins MH, Prandoni P. Assessment of validity and reproducibility of a clinical scale for the post-thrombotic syndrome. Haemostasis. 1994; 24:158a.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular intervention for portal vein system thrombosis in a patient with protein S deficiency: A case report
- Interventional Radiologic Treatment of Deep Venous Thrombosis in Lower Extremity
- Thrombectomy Device for Deep Vein Thrombosis
- Interventional Treatment of Deep Vein Thrombosis
- The Efficacy of Endovascular Treatment for Deep Vein Thrombosis