Investig Clin Urol.
2017 Nov;58(6):460-467. 10.4111/icu.2017.58.6.460.
Chlamydia trachomatis versus common uropathogens as a cause of chronic bacterial prostatitis: Is there any difference? Results of a prospective parallel-cohort study
- Affiliations
-
- 1Department of Urology, Santa Chiara Regional Hospital, Trento, Italy. ktommy@libero.it
- 2Department of Urology, University of Turin, Turin, Italy.
- 3Division of Pathological Anatomy, University of Florence, Florence, Italy.
- 4Urology and Sonography Secondary Care Clinic, Azienda Ospedaliera Istituti Clinici di Perfezionamento, Milano, Italy.
- 5Department of Urology, University of Naples Federico II, Naples, Italy.
- 6Biomedical Research Division, Department of Theoretical and Applied Sciences, Universita degli Studi dell'Insubria, Busto Arsizio, Italy.
- 7Department of Translational Research and New Technologies, University of Pisa, Pisa, Italy.
- KMID: 2414775
- DOI: http://doi.org/10.4111/icu.2017.58.6.460
Abstract
- PURPOSE
The role of Chlamydia trachomatis (CT) infection in chronic bacterial prostatitis (CBP) is well known. What is unclear is whether there are any differences in the course or clinical outcome of the disease when the cause is CT or other uropathogens.
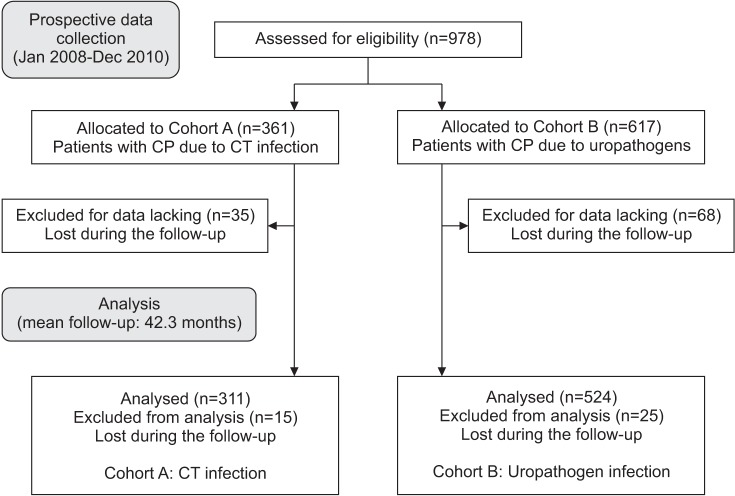
MATERIALS AND METHODS
A series of 311 patients affected by CBP due to CT (cohort A) was compared with a group of 524 patients affected by CBP caused by common uropathogen bacteria (cohort B). All participants completed the following questionnaires: National Institutes of Health Chronic Prostatitis Symptom Index, International Prostate Symptom Score, International Index of Erectile Function-15 erectile function domain (IIEF-15-EFD), Premature Ejaculation Diagnostic Tool (PEDT), and the Short Form 36 (SF-36) Health Survey. All patients were followed with clinical and microbiological evaluations.
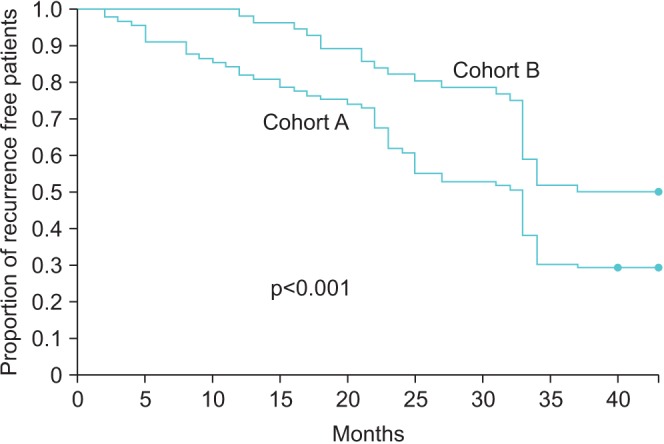
RESULTS
After a mean follow-up time of 42.3 months, the number of symptomatic episodes was significantly higher in patients in cohort A than in cohort B (4.1±1.1 vs. 2.8±0.8, p<0.001), and the mean time to first symptomatic recurrence was shorter in cohort A than in cohort B (3.3±2.3 months vs. 5.7±1.9 months, p<0.001). Moreover, scores on the SF-36 tool were significantly lower in cohort A (96.5±1.0 vs. 99.7±1.9, p<0.001) at the first symptomatic recurrence. Cohort A also showed significantly lower scores on the IIEF-15-EFD and PEDT questionnaires at the end of the follow-up period (26.8±2.9 vs. 27.3±3.3, p=0.02 and 11.5±2.3 vs. 4.5±2.8, p<0.001, respectively).
CONCLUSIONS
Patients affected by CBP due to CT infection have a higher number of symptomatic recurrences with a more severe impact on quality of life.
Keyword
MeSH Terms
Figure
Reference
-
1. World Health Organization. Global prevalence and incidence of selected curable sexually transmitted infections: overview and estimates. Geneva: World Health Organization;2001.2. Cai T, Wagenlehner FM, Mondaini N, D'Elia C, Meacci F, Migno S, et al. Effect of human papillomavirus and Chlamydia trachomatis co-infection on sperm quality in young heterosexual men with chronic prostatitis-related symptoms. BJU Int. 2014; 113:281–287. PMID: 23906072.3. Wagenlehner FM, Naber KG, Weidner W. Chlamydial infections and prostatitis in men. BJU Int. 2006; 97:687–690. PMID: 16536754.
Article4. Ouzounova-Raykova V, Ouzounova I, Mitov IG. May Chlamydia trachomatis be an aetiological agent of chronic prostatic infection? Andrologia. 2010; 42:176–181. PMID: 20500746.
Article5. Mazzoli S, Cai T, Rupealta V, Gavazzi A, Castricchi Pagliai R, Mondaini N, et al. Interleukin 8 and anti-chlamydia trachomatis mucosal IgA as urogenital immunologic markers in patients with C. trachomatis prostatic infection. Eur Urol. 2007; 51:1385–1393. PMID: 17107749.
Article6. Mazzoli S, Cai T, Addonisio P, Bechi A, Mondaini N, Bartoletti R. Chlamydia trachomatis infection is related to poor semen quality in young prostatitis patients. Eur Urol. 2010; 57:708–714. PMID: 19482415.
Article7. Cai T, Pisano F, Magri V, Verze P, Mondaini N, D'Elia C, et al. Chlamydia trachomatis infection is related to premature ejaculation in chronic prostatitis patients: results from a cros-ssectional study. J Sex Med. 2014; 11:3085–3092. PMID: 25256084.8. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999; 282:236–237. PMID: 10422990.
Article9. Abramson JH, Abramson ZH. Survey methods in community medicine: epidemiological research, programme evaluation, clinical trials. 5th ed. London: Livingstone;2000.10. Krieger JN, McGonagle LA. Diagnostic considerations and interpretation of microbiological findings for evaluation of chronic prostatitis. J Clin Microbiol. 1989; 27:2240–2244. PMID: 2584375.
Article11. Naber KG, Bergman B, Bishop MC, Bjerklund-Johansen TE, Botto H, Lobel B, et al. EAU guidelines for the management of urinary and male genital tract infections. Urinary Tract Infection (UTI) Working Group of the Health Care Office (HCO) of the European Association of Urology (EAU). Eur Urol. 2001; 40:576–588. PMID: 11752870.12. Bartoletti R, Cai T, Mondaini N, Dinelli N, Pinzi N, Pavone C, et al. Prevalence, incidence estimation, risk factors and characterization of chronic prostatitis/chronic pelvic pain syndrome in urological hospital outpatients in Italy: results of a multicenter case-control observational study. J Urol. 2007; 178:2411–2415. PMID: 17937946.
Article13. Nickel JC, Alexander RB, Schaeffer AJ, Landis JR, Knauss JS, Propert KJ, et al. Leukocytes and bacteria in men with chronic prostatitis/chronic pelvic pain syndrome compared to asymptomatic controls. J Urol. 2003; 170:818–822. PMID: 12913707.
Article14. Giubilei G, Mondaini N, Crisci A, Raugei A, Lombardi G, Travaglini F, et al. The Italian version of the National Institutes of Health Chronic Prostatitis Symptom Index. Eur Urol. 2005; 47:805–811. PMID: 15925077.
Article15. Badía X, García-Losa M, Dal-Ré R. Ten-language translation and harmonization of the International Prostate Symptom Score: developing a methodology for multinational clinical trials. Eur Urol. 1997; 31:129–140. PMID: 9076454.16. Cappelleri JC, Rosen RC, Smith MD, Mishra A, Osterloh IH. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999; 54:346–351. PMID: 10443736.
Article17. Apolone G, Mosconi P. The Italian SF-36 Health Survey: translation, validation and norming. J Clin Epidemiol. 1998; 51:1025–1036. PMID: 9817120.18. Symonds T, Perelman MA, Althof S, Giuliano F, Martin M, May K, et al. Development and validation of a premature ejaculation diagnostic tool. Eur Urol. 2007; 52:565–573. PMID: 17275165.
Article19. Nickel JC, Downey J, Hunter D, Clark J. Prevalence of prostatitis-like symptoms in a population based study using the National Institutes of Health chronic prostatitis symptom index. J Urol. 2001; 165:842–845. PMID: 11176483.
Article20. Park H, Sim SM, Lee G. The presence of Chlamydia is associated with increased leukocyte counts and pain severity in men with chronic pelvic pain syndrome. Urology. 2015; 85:574–579. PMID: 25733268.
Article21. Koroku M, Kumamoto Y, Hirose T. A study on the role of Chlamydia trachomatis in chronic prostatitis--analysis of anti-Chlamydia trachomatis specific IgA in expressed prostate secretion by western-blotting method. Kansenshogaku Zasshi. 1995; 69:426–437. PMID: 7751752.22. Nickel JC, Downey JA, Nickel KR, Clark JM. Prostatitis-like symptoms: one year later. BJU Int. 2002; 90:678–681. PMID: 12410746.
Article23. Turner JA, Ciol MA, Von Korff M, Berger R. Prognosis of patients with new prostatitis/pelvic pain syndrome episodes. J Urol. 2004; 172:538–541. PMID: 15247724.
Article24. Skerk V, Schönwald S, Krhen I, Banaszak A, Begovac J, Strugar J, et al. Comparative analysis of azithromycin and ciprofloxacin in the treatment of chronic prostatitis caused by Chlamydia trachomatis. Int J Antimicrob Agents. 2003; 21:457–462. PMID: 12727080.
Article25. Serefoglu EC, Yaman O, Cayan S, Asci R, Orhan I, Usta MF, et al. The comparison of premature ejaculation assessment questionnaires and their sensitivity for the four premature ejaculation syndromes: results from the Turkish society of andrology sexual health survey. J Sex Med. 2011; 8:1177–1185. PMID: 21269396.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Isolation of Chlamydia Trachomatis in Non-gonococcal Urethritis and Chronic Prostatitis and the Result of Treatment with Antibiotics
- Detection of Chlamydia Trachomatis in Non-gonococcal Urethritis and Chronic Prostatitis by Enzyme Immunoassay Technique
- Serodiagnosis and Serotyping of Chlamydia Trachomatis in Male Urogenital Organ with Indirect microimmunofluorescence Technique
- Chronic Bacterial Prostatitis
- Detection rate chlamydia trichomatis by enzyme immunoassay technique in the sexually transmitted disease