Allergy Asthma Respir Dis.
2018 May;6(3):179-183. 10.4168/aard.2018.6.3.179.
Isolated pulmonary Langerhans cell histiocytosis in a 10-month-old infant
- Affiliations
-
- 1Department of Pediatrics, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea. CJ@yuhs.ac
- KMID: 2412522
- DOI: http://doi.org/10.4168/aard.2018.6.3.179
Abstract
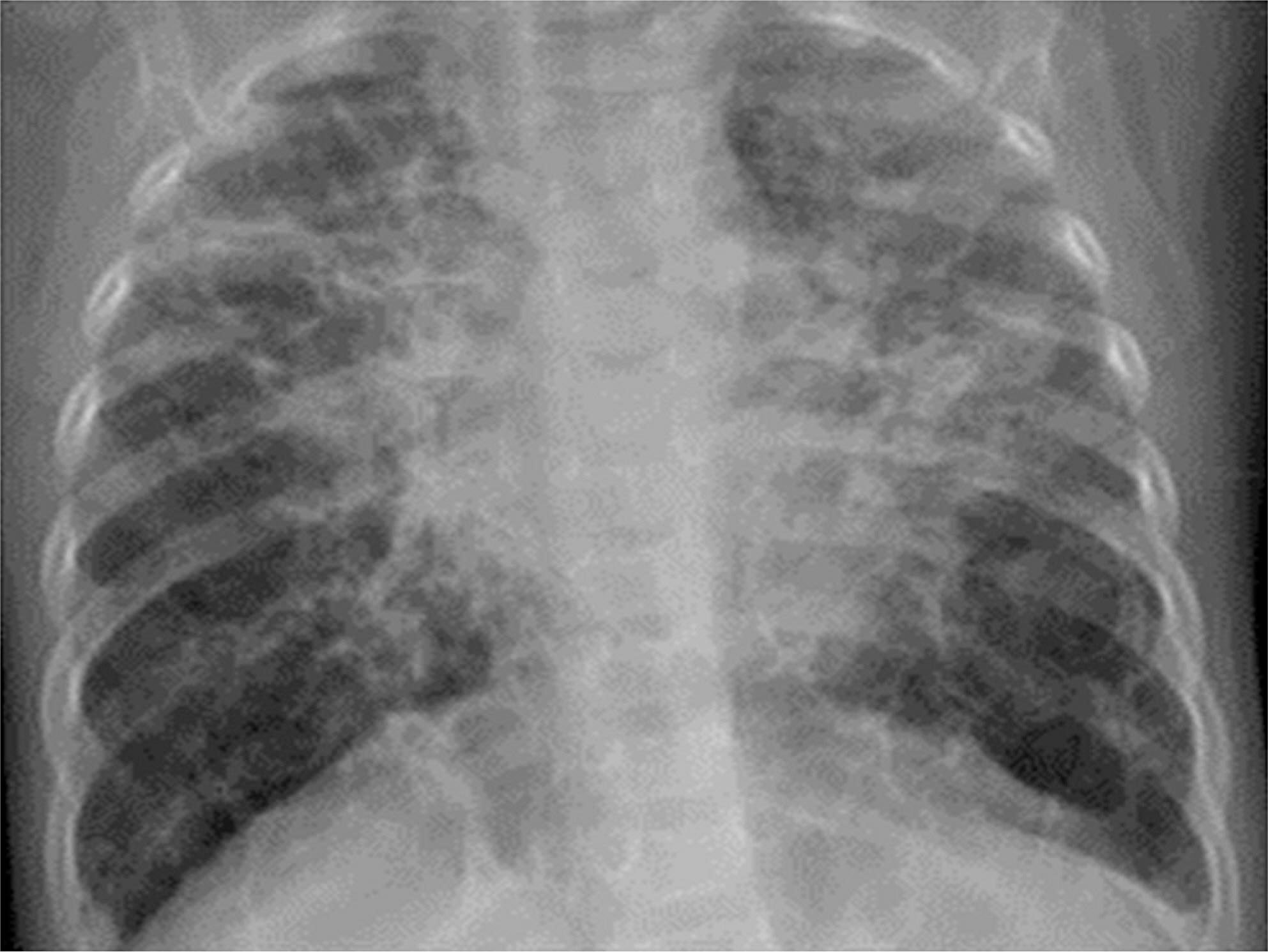
- Langerhans cell histiocytosis (LCH) is characterized by clonal proliferation and accumulation of abnormal dendritic (Langerhans) cells in various organs. Pulmonary involvement, although rare in children, has been reported in 20%-50% of childhood cases of multisystem LCH. Isolated pulmonary LCH in children, especially in infants, is still rarer, but should be suspected in those with cystic lung disease. We report a case of a 10-month-old boy who presented with chronic dyspnea and whose chest computed tomography (CT) scan demonstrated cystic lesions. Lung biopsy established the diagnosis of LCH; microscopy revealed a background of lymphocytes and eosinophils with kidney-shaped abnormal cells. These abnormal cells were positive for S-100, CD207 (Langerin), and CD1a on immunohistochemical staining. Chemotherapy was administered using a cytotoxic agent (vinblastine) and a steroid. After 12 weeks of induction chemotherapy, although no significant change in cyst size was noted on chest CT, clinical symptoms improved. Consolidation chemotherapy was then administered for 1 year. Thereafter, chest CT findings demonstrated a significant decrease in cyst size and a significant increase in the volume of normal lung parenchyma. Therefore, aggressive treatment of isolated pulmonary LCH in infants with severe tissue destruction and symptoms seems warranted.
MeSH Terms
Figure
Reference
-
1. Picarsic J, Jaffe R. Nosology and pathology of Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 2015; 29:799–823.
Article2. Weitzman S, Egeler RM. Langerhans cell histiocytosis: update for the pe-diatrician. Curr Opin Pediatr. 2008; 20:23–9.
Article3. El Demellawy D, Young JL, de Nanassy J, Chernetsova E, Nasr A. Langerhans cell histiocytosis: a comprehensive review. Pathology. 2015; 47:294–301.
Article4. Elia D, Torre O, Cassandro R, Caminati A, Harari S. Pulmonary Langerhans cell histiocytosis: a comprehensive analysis of 40 patients and literature review. Eur J Intern Med. 2015; 26:351–6.
Article5. Odame I, Li P, Lau L, Doda W, Noseworthy M, Babyn P, et al. Pulmonary Langerhans cell histiocytosis: a variable disease in childhood. Pediatr Blood Cancer. 2006; 47:889–93.
Article6. Braier J, Latella A, Balancini B, Castaños C, Rosso D, Chantada G, et al. Outcome in children with pulmonary Langerhans cell Histiocytosis. Pediatr Blood Cancer. 2004; 43:765–9.
Article7. Sawalha L, Kumar A, Arshad A, Mador MJ. Pulmonary Langerhans cell histiocytosis: radiologic resolution following cessation of second hand smoking. Clin Respir J. 2017; 11:1063–7.
Article8. Kasmani R, Narwal-Chadha R, Naveed S, Sahoo D. Isolated pulmonary Langerhans cell histiocytosis. QJM. 2009; 102:741–2.
Article9. Kanik-Yuksek S, Ozkaya-Parlakay A, Gulhan B, Ozyoruk D, Karakus E, Cinel G, et al. A rare diagnosis in children: isolated pulmonary Langerhans cell histiocytosis. Clin Respir J. 2018; 12:355–6.
Article10. Mukhopadhyay S, Eckardt SM, Scalzetti EM. Diagnosis of pulmonary Langerhans cell histiocytosis by CT-guided core biopsy of lung: a report of three cases. Thorax. 2010; 65:833–5.
Article11. Aricò M, Girschikofsky M, Généreau T, Klersy C, McClain K, Grois N, et al. Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society. Eur J Cancer. 2003; 39:2341–8.12. Minami M, Shima T, Kato K, Yamamoto H, Tsuchihashi K, Oku S, et al. Successful treatment of adult Langerhans cell histiocytosis with intensi-fied chemotherapy. Int J Hematol. 2015; 102:244–8.
Article13. Kim HJ, Lee KS, Johkoh T, Tomiyama N, Lee HY, Han J, et al. Pulmonary Langerhans cell histiocytosis in adults: high-resolution CT-pathology comparisons and evolutional changes at CT. Eur Radiol. 2011; 21:1406–15.
Article14. Varkki S, Tergestina M, Bhonsle VS, Moses PD, Mathai J, Korula S. Isolated pulmonary Langerhans cell histiocytosis. Indian J Pediatr. 2013; 80:700–3.
Article15. Wang Q, Xia W, Zhao DY. Isolated pulmonary Langerhans cell histiocytosis in a two-year-old child: case report and literature review. Zhonghua Er Ke Za Zhi. 2012; 50:146–50.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary Langerhans Cell Histiocytosis Accompanied by Active Pulmonary Tuberculosis
- Isolated Thymic Langerhans Cell Histiocytosis
- A Case of Pulmonary Langerhans Cell Histiocytosis with Pneumothorax
- Infant Langerhans Cell Histiocytosis Presented as Isolated Splenomegaly and Prolonged Fever
- Spontaneous Pneumothorax due to Pulmonary Invasion in Multisystemic Langerhans Cell Histiocytosis: A case report