Clin Orthop Surg.
2017 Mar;9(1):19-28. 10.4055/cios.2017.9.1.19.
Cementless Total Hip Arthroplasty Involving Trochanteric Osteotomy without Subtrochanteric Shortening for High Hip Dislocation
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul National University College of Medicine, Seoul, Korea. jjyos@snu.ac.kr
- KMID: 2412299
- DOI: http://doi.org/10.4055/cios.2017.9.1.19
Abstract
- BACKGROUND
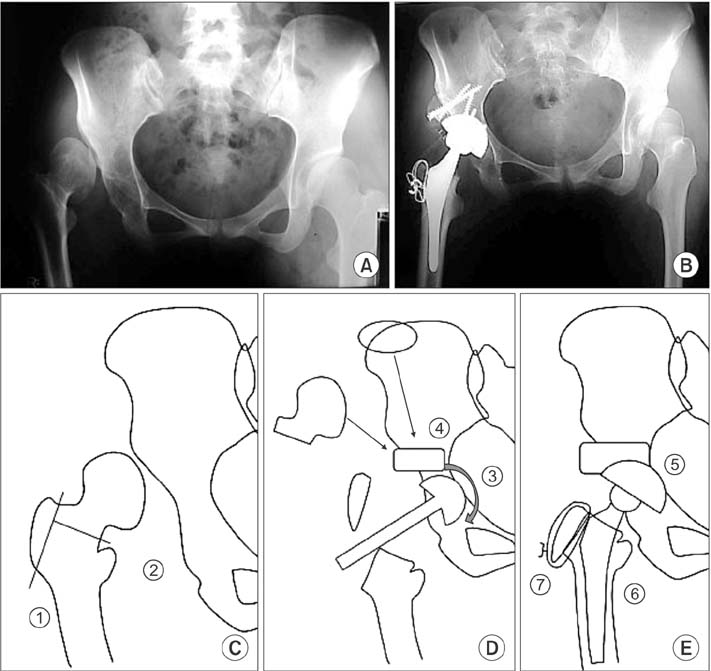
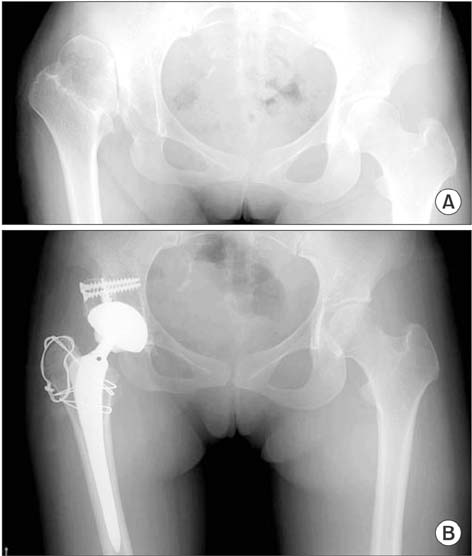
Total hip arthroplasty with subtrochanteric shortening osteotomy is widely performed for high hip dislocation. However, suboptimal leg length discrepancy correction and nonunion of the osteotomy site remain concerns. Although total hip arthroplasty using trochanteric osteotomy without subtrochanteric osteotomy was introduced, cemented implants have been more commonly used than contemporary cementless implants in this procedure. We evaluated the long-term results of cementless total hip arthroplasty with trochanteric osteotomy without subtrochanteric osteotomy for high hip dislocation.
METHODS
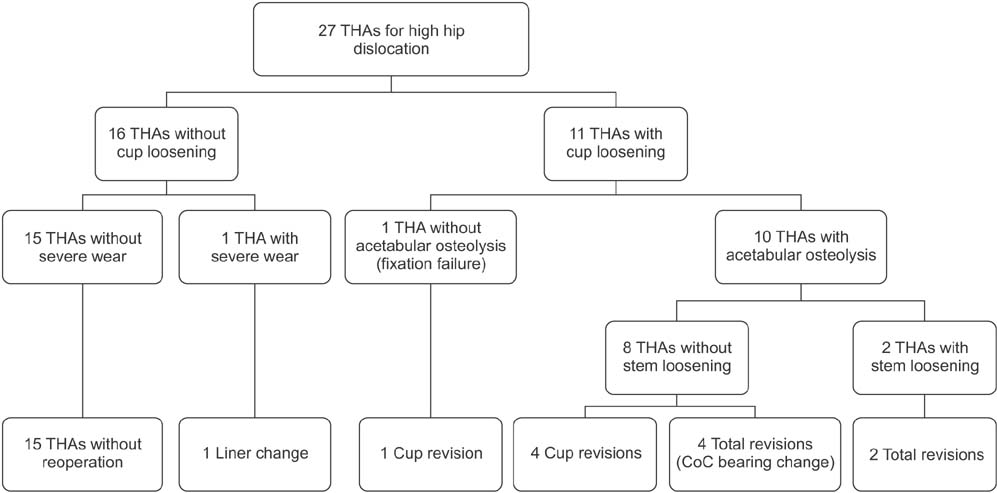
From 1990 to 2002, 27 cementless total hip arthroplasties using trochanteric osteotomy without subtrochanteric osteotomy were performed in 26 patients with Crowe III or IV high hip dislocation and a mean age of 36.4 ± 12.9 years. Seven ceramic-on-ceramic, 8 ceramic-on-polyethylene, 10 metal-on-polyethylene, and 2 metal-on-metal bearings were inserted. Mean follow-up was 15.1 ± 3.7 years. We retrospectively reviewed medical records and radiographic data and evaluated the clinical and radiological results including the Harris hip score, implant survival, correction of leg length discrepancy, and occurrence of complications.
RESULTS
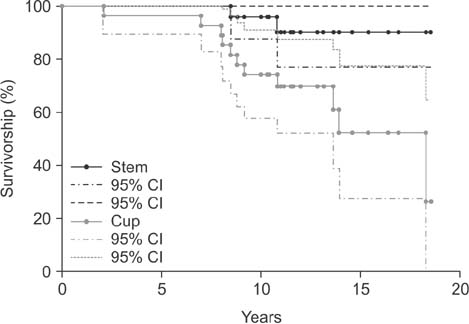
The mean Harris hip score and leg length discrepancy improved significantly from 73.3 to 94.9 points and from 4.3 cm to 1.0 cm, respectively. With revision for loosening set as the end point, implant survival rates at 10 and 15 years postoperatively were 96.0% and 90.9% for stems and 74.1% and 52.3% for cups. In 8 of 10 hips with the metal-on-polyethylene bearing and 4 of 8 hips with the ceramic-on-polyethylene bearing, revision surgery was performed for aseptic loosening. However, no revision was performed in hips with the ceramic-on-ceramic bearing or the metal-on-metal bearing. Implant survival was significantly different by the type of bearing surface. Two permanent neurologic complications occurred in patients with a limb lengthening over 3.5 cm.
CONCLUSIONS
With proper selection of the bearing surface coupled with adjustment of lengthening, cementless total hip arthroplasty using trochanteric osteotomy without subtrochanteric osteotomy might be a favorable treatment option for high hip dislocation.
MeSH Terms
-
Adolescent
Adult
Arthroplasty, Replacement, Hip/instrumentation/*methods
Ceramics
Female
Femur/diagnostic imaging/*surgery
Follow-Up Studies
Hip Dislocation/diagnostic imaging/*surgery
Hip Joint/diagnostic imaging/surgery
*Hip Prosthesis
Humans
Leg Length Inequality/diagnostic imaging/surgery
Male
Metal-on-Metal Joint Prostheses
Middle Aged
Osteotomy/*methods
Polyethylene
Prosthesis Design
Prosthesis Failure
Radiography
Reoperation
Survival Rate
Young Adult
Polyethylene
Figure
Reference
-
1. Weinstein SL. Natural history and treatment outcomes of childhood hip disorders. Clin Orthop Relat Res. 1997; (344):227–242.
Article2. Kim YH, Seo HS, Kim JS. Outcomes after THA in patients with high hip dislocation after childhood sepsis. Clin Orthop Relat Res. 2009; 467(9):2371–2378.
Article3. Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979; 61(1):15–23.
Article4. Sanchez-Sotelo J, Berry DJ, Trousdale RT, Cabanela ME. Surgical treatment of developmental dysplasia of the hip in adults: II. arthroplasty options. J Am Acad Orthop Surg. 2002; 10(5):334–344.
Article5. Eskelinen A, Helenius I, Remes V, Ylinen P, Tallroth K, Paavilainen T. Cementless total hip arthroplasty in patients with high congenital hip dislocation. J Bone Joint Surg Am. 2006; 88(1):80–91.
Article6. Lai KA, Liu J, Liu TK. Use of iliofemoral distraction in reducing high congenital dislocation of the hip before total hip arthroplasty. J Arthroplasty. 1996; 11(5):588–593.
Article7. Krych AJ, Howard JL, Trousdale RT, Cabanela ME, Berry DJ. Total hip arthroplasty with shortening subtrochanteric osteotomy in Crowe type-IV developmental dysplasia. J Bone Joint Surg Am. 2009; 91(9):2213–2221.
Article8. Hartofilakidis G, Stamos K, Karachalios T. Treatment of high dislocation of the hip in adults with total hip arthroplasty: operative technique and long-term clinical results. J Bone Joint Surg Am. 1998; 80(4):510–517.
Article9. Hartofilakidis G, Karachalios T. Total hip arthroplasty for congenital hip disease. J Bone Joint Surg Am. 2004; 86(2):242–250.
Article10. Khanuja HS, Vakil JJ, Goddard MS, Mont MA. Cementless femoral fixation in total hip arthroplasty. J Bone Joint Surg Am. 2011; 93(5):500–509.
Article11. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; (121):20–32.
Article12. Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; (141):17–27.13. Joshi RP, Eftekhar NS, McMahon DJ, Nercessian OA. Osteolysis after Charnley primary low-friction arthroplasty: a comparison of two matched paired groups. J Bone Joint Surg Br. 1998; 80(4):585–590.14. Martell JM, Pierson RH 3rd, Jacobs JJ, Rosenberg AG, Maley M, Galante JO. Primary total hip reconstruction with a titanium fiber-coated prosthesis inserted without cement. J Bone Joint Surg Am. 1993; 75(4):554–571.
Article15. Browne AO, Sheehan JM. Trochanteric osteotomy in Charnley low-friction arthroplasty of the hip. Clin Orthop Relat Res. 1986; (211):128–133.
Article16. Reikeras O, Haaland JE, Lereim P. Femoral shortening in total hip arthroplasty for high developmental dysplasia of the hip. Clin Orthop Relat Res. 2010; 468(7):1949–1955.
Article17. Paavilainen T, Hoikka V, Paavolainen P. Cementless total hip arthroplasty for congenitally dislocated or dysplastic hips: technique for replacement with a straight femoral component. Clin Orthop Relat Res. 1993; (297):71–81.18. Zhao X, Zhu ZA, Xie YZ, Yu B, Yu DG. Total hip replacement for high dislocated hips without femoral shortening osteotomy. J Bone Joint Surg Br. 2011; 93(9):1189–1193.
Article19. Lai KA, Shen WJ, Huang LW, Chen MY. Cementless total hip arthroplasty and limb-length equalization in patients with unilateral Crowe type-IV hip dislocation. J Bone Joint Surg Am. 2005; 87(2):339–345.
Article20. Lerch M, Thorey F, von Lewinski G, Klages P, Wirth CJ, Windhagen H. An alternative treatment method to restore limb-length discrepancy in osteoarthritis with high congenital hip dislocation. Arch Orthop Trauma Surg. 2009; 129(12):1593–1599.
Article21. Holinka J, Pfeiffer M, Hofstaetter JG, Lass R, Kotz RI, Giurea A. Total hip replacement in congenital high hip dislocation following iliofemoral monotube distraction. Int Orthop. 2011; 35(5):639–645.
Article22. Learmonth ID, Hussell JG, Smith EJ. Inadequate polyethylene thickness and osteolysis in cementless hip arthroplasty. J Arthroplasty. 1997; 12(3):305–309.
Article23. Lee PC, Shih CH, Chen WJ, Tu YK, Tai CL. Early polyethylene wear and osteolysis in cementless total hip arthroplasty: the influence of femoral head size and polyethylene thickness. J Arthroplasty. 1999; 14(8):976–981.
Article24. Stans AA, Pagnano MW, Shaughnessy WJ, Hanssen AD. Results of total hip arthroplasty for Crowe Type III developmental hip dysplasia. Clin Orthop Relat Res. 1998; (348):149–157.
Article25. Clarke IC, Good V, Williams P, et al. Ultra-low wear rates for rigid-on-rigid bearings in total hip replacements. Proc Inst Mech Eng H. 2000; 214(4):331–347.
Article26. Hatton A, Nevelos JE, Matthews JB, Fisher J, Ingham E. Effects of clinically relevant alumina ceramic wear particles on TNF-alpha production by human peripheral blood mononuclear phagocytes. Biomaterials. 2003; 24(7):1193–1204.
Article27. Hannouche D, Nich C, Bizot P, Meunier A, Nizard R, Sedel L. Fractures of ceramic bearings: history and present status. Clin Orthop Relat Res. 2003; (417):19–26.28. Hartofilakidis G, Babis GC, Georgiades G, Kourlaba G. Trochanteric osteotomy in total hip replacement for congenital hip disease. J Bone Joint Surg Br. 2011; 93(5):601–607.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Modular Cementless Total Hip Arthroplasty with Subtrochanteric Shortening Osteotomy in Patients with High Hip Dislocation
- Cementless Total Hip Arthroplasty with Subtrochanteric Transverse Shortening Osteotomy in Patients with High Hip Dislocation
- Short Term Results of Cementless Total Hip Arthroplasty with Subtrochanteric Shortening Osteotomy in Severe Dysplasia of Hip
- Total Hip Replacement in Unreduced Hip Dislocation
- Step-Cut Subtrochanteric Osteotomy Combined with Total Hip Arthroplasty for Neglected Traumatic Hip Dislocations